The Pattern of Neurological Emergencies: Frequency, Etiology and Outcome, for Patients Admitted to Intensive Care Unit at Khartoum State Hospitals
*Corresponding Author: Mahmoud Hussien Daoud, Department of Internal Medicine, University of Gezira, Wad Madani, Sudan, Email: dr.mhs.24@hotmail.comReceived Date: Dec 15, 2023 / Published Date: Jan 15, 2024
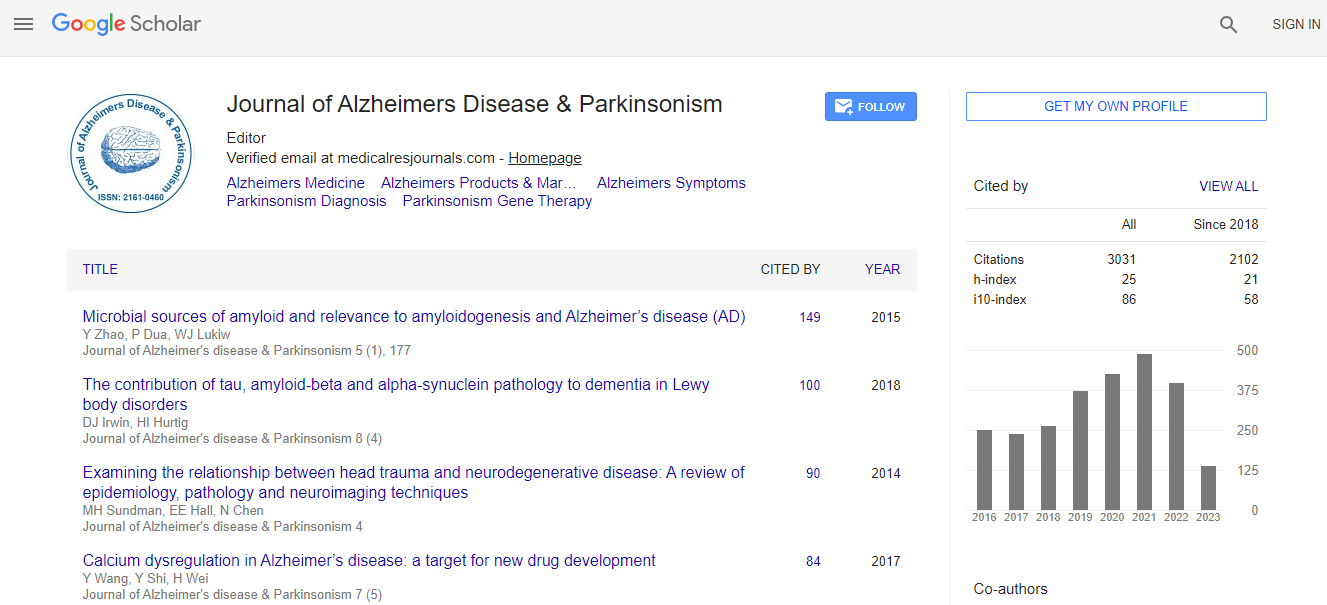
Citation: Daoud MH, Abuobieda H, Abdelhalim SI, Mohmed MHA, Elamin AEA (2024) The Pattern of Neurological Emergencies: Frequency, Etiology and Outcome, for Patients Admitted to Intensive Care Unit at Khartoum State Hospitals. J Alzheimers Dis Parkinsonism 14:590.DOI: 10.4172/2161-0460.1000590
Copyright: © 2024 Daoud MH, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Neurological emergencies are frequent presentations and often end with devastating short and long term consequences. Neurological disorders are increasingly prevalent in Sub-Saharan Africa with paucity of data on adult neurological emergencies in our context.
Methods: A prospective cross-sectional study enrolled 103 patients with neurologic emergencies admitted to Intensive Care Unit (ICU) Khartoum state intensive care departments during the period from October 2019 to April 2020. Data regarding demographics, presentations, clinical examinations, laboratory investigations, indications of ICU admission, diagnosis of neurological conditions, length of ICU stay, patterns of medications and outcomes were collected. Data was analyzed by using Statistical Package for the Social Sciences (SPSS) v. 21.0.
Results: Among 103 patients with neurologic emergencies admitted to ICU, 56% were Males (M) and 44% were Females (F). Patients are categorized into central nervous system diseases in which intracranial hemorrhage 28.1%, meningitis 27.2%, encephalitis 27.2%, ischemic stroke 18.4% were the common diagnoses. Whereas, in the peripheral nervous system Guillain-Barré Syndrome (GBS) 15.5%, Myasthenia Gravis (MG) crisis 3.88% were the common diseases. The common symptoms were altered mental status 64.1%, seizures 34%, motor weakness 27.2%, headache 18.4%, dysphagia 16.5%, fever 16.5%, shortness of breath 9.7% and mutism 7.8%. Hypertension 43.7% and diabetes mellitus 21.4% were the major co morbidities. Indications for ICU admission were mostly decreased level of consciousness 74.8%, accelerated hypertension 21.4%, respiratory failure 19.4%, aspiration pneumonia 10.7% and intractable seizures 2.9%. Majority of the patients 83.5% received antibiotics, 36% received Low Molecular Weight Heparin (LMWH), 32% received Proton Pump Inhibitors (PPI) and 10.6% received mechanical ventilation. 44% of patients improved and discharged, 41% developed complications mainly aspiration pneumonia 24.3% and 15% died.
Conclusion: Sudanese patients with neurologic emergencies admitted to ICU were older and mostly males. Intracranial hemorrhage and meningoencephalitis were the main diagnosis. Patients commonly presented with altered mental status. A decreased level of consciousness low Glasgow Coma Scale (GCS) was the foremost indication of ICU admission. Half of the patients were improved and aspiration pneumonia observed in a quarter of the patients.

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi