Spontaneous Thrombosis of a Ruptured Pial Arteriovenous Malformation and an Associated Large Intranidal Aneurysm with Perianeurysmal Edema in an Infant: A Case Report
*Corresponding Author: Iampreechakul Prasert, Department of Neurological Surgery, Prasat Neurological Institute, 312 Ratchawithi Road, Khwaeng Thung Phaya Thai, Bangkok 10400, Thailand, Tel: 6623069899, Email: bangruad@hotmail.comReceived Date: Apr 30, 2019 / Accepted Date: May 10, 2019 / Published Date: May 17, 2019
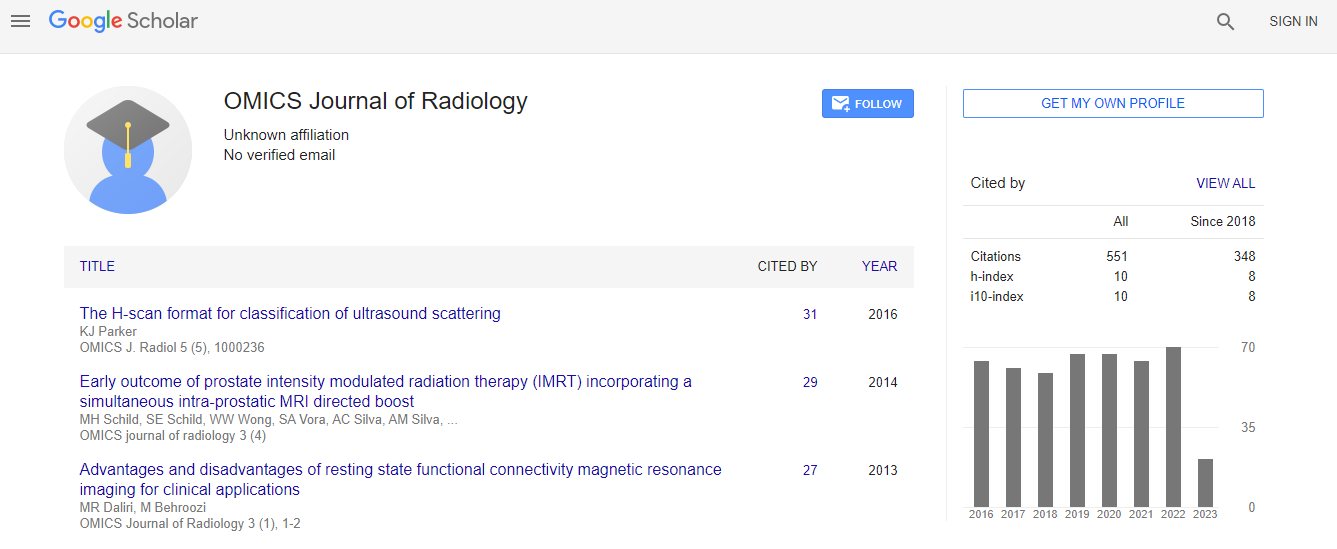
Citation: Iampreechakul P, Wangtanaphat K, Tirakotai W, Lertbutsayanukul P, Wattanasen Y, et al. (2019) Spontaneous Thrombosis of a Ruptured Pial Arteriovenous Malformation and an Associated Large Intranidal Aneurysm with Perianeurysmal Edema in an Infant: A Case Report. OMICS J Radiol 8: 309. doi: 10.4172/2167- 7964.1000309
Copyright: © 2019 Iampreechakul P, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
The authors reported an extremely rare case of complete spontaneous thrombosis of a pial arteriovenous malformation associated with a large intranidal aneurysm in an infant. A 10-month-old infant experienced nocturnal seizure witnessed by her mother. Computed tomography scan and magnetic resonance imaging (MRI) of the brain disclosed a ruptured intranidal aneurysm resulting in acute hemorrhage in left anterior interhemispheric subdural space with extension along posterior interhemispheric space, tentorium, bilateral tentorial cerebelli, and hemispheric
convexities. MRI and magnetic resonance angiography (MRA) showed a pial arteriovenous malformation (AVM), at medial side of the left superior frontal gyrus, associated with a large partially thrombosed aneurysm with perianeurysmal edema. Cerebral angiography confirmed a small pial AVM arising from left middle internal frontal branches of the left anterior cerebral artery (ACA) with early venous drainage into medial frontal veins and forward to the superior sagittal sinus. Subseletive injection of the left ACA injection clearly demonstrated multiple indirect small feeders, unsuitable for endovascular treatment. Sequential MRI of the brain revealed the evolution of a large partially thrombosed intranidal aneurysm with surrounding parenchymal edema. Follow-up MRI and contrasted MRA, obtained at the age of 7 years, demonstrated complete obliteration of the pial AVM and large thrombosed intranidal aneurysm. At the age of 11 years, control angiography confirmed total disappearance of the pial arteriovenous malformation and a large thrombosed intranidal aneurysm. The factors associated with spontaneous regression of a ruptured pial AVM and an associated intranidal aneurysm in the present case was the presence of intracranial hemorrhage and small nidus.

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi