Research Article
Shame, Psychiatric Disorders and Health Promoting Life Style after Bariatric Surgery
| Haldis Økland Lier1*, Eva Biringer1, Jofrid Bjørkvik1, Jan H. Rosenvinge2, Bjarte Stubhaug1,3 and Tone Tangen3 | |
| 1Section of Mental Health Research, Haugesund Hospital, Helse Fonna HF, Haugesund, Norway | |
| 2Department of Psychology, Faculty of Health Sciences, University of Tromsø, Tromsø, Norway | |
| 3Section of Psychiatry, Institute of Clinical Medicine, University of Bergen, Bergen, Norway | |
| This study was supported by a grant from the Western Regional Health Authority, Norway. | |
| Corresponding Author : | Dr. Haldis Økland Lier Section of Mental Health Research Haugesund Hospital, Helse Fonna HF P.O.Box 2170, N-5504 Haugesund, Norway Tel: 004752733782 / 004752732700 E-mail: haldis.johanne.oekland.lier@helse-fonna.no |
| Received December 27, 2011; Accepted January 23, 2012; Published January 28, 2012 | |
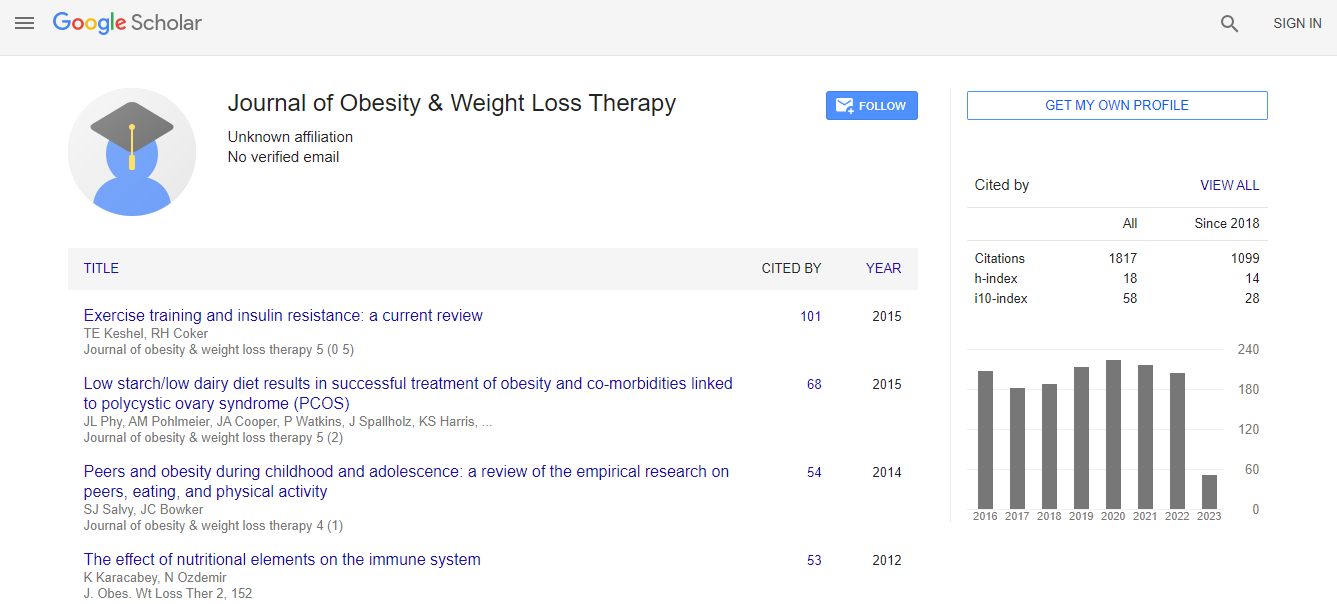
| Citation: Lier HØ, Biringer E, Bjørkvik J, Rosenvinge JH, Stubhaug B, et al. (2012) Shame, Psychiatric Disorders and Health Promoting Life Style after Bariatric Surgery. J Obes Weig los Ther 2:113. doi:10.4172/2165-7904.1000113 | |
| Copyright: © 2012 Lier HØ, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. | |
Abstract
Objective: Postoperative outcomes after bariatric surgery depend greatly on engagement in health promoting behaviour, including regular physical activity and healthy eating behaviour. Adherence to these guidelines varies among patients after bariatric surgery. The present study examined associations between shame, psychiatric disorders and engagement in health promoting behaviour in patients with severe obesity that have undergone bariatric surgery.
Method:One-hundred and twenty-seven patients (F/M: 74/ 26) with median Body Mass Index (BMI) 44.1 kg/m2 (IQR=6.0) and median age 40.0 years (IQR=15.0) were examined for psychiatric disorders and personality disorders. The participants completed the Eating Disorder Examination Questionnaire (EDE-Q) and Internalized Shame Scale (ISS) pre- and postoperatively. At one year follow-up, they also reported their compliance with postoperative guidelines regarding eating habits and physical activity.
Results: The median ISS-score was significantly higher in patients with comorbid psychiatric disorders compared to patients without comorbid psychiatric disorders (median ISS score 36.0 and 9.0 respectively, p<.001). ISS score and self-evaluation based on body shape and weight were significantly correlated. Furthermore, preoperative ISS score was negatively correlated with level of physical activity (r=-.25, p=.022) one year after surgery.
Conclusion:The present findings suggest that patients with a high level of shame should be given priority for postoperative follow-up, in order to improve the patients’ ability to establish life-style changes associated with sustained positive postoperative outcome.

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi