Research Article
Risk Factors and Clinical Presentation of Uterine Rupture in the Unscarred Uterus: A Case Control Study
Anne Pinton*, Eric Boudier, Arnaud Joal, Nicolas Sananes, François Severac, Bruno Langer and Cherif Youssef
Department Obstetrics and Gynecology, Strasbourg University, Strasbourg, France
- *Corresponding Author:
- Anne Pinton
Department Obstetrics and Gynecology
Strasbourg University, Strasbourg, France
Tel: 33388128311
E-mail: anne.pinton@gmail.com
Received date: August 25, 2015; Accepted date: October 14, 2016; Published date: October 19, 2016
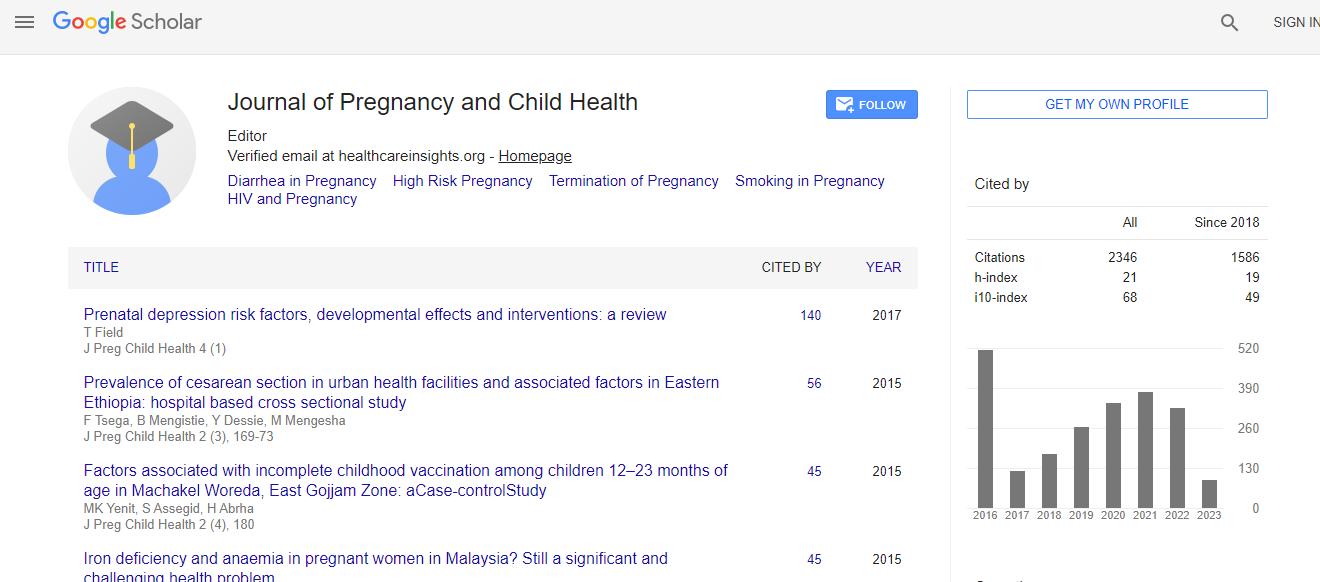
Citation: Pinton A, Boudier E, Joal A, Sananes N, Severac F, et al. (2016) Risk Factors and Clinical Presentation of Uterine Rupture in the Unscarred Uterus: A Case Control Study. J Preg Child Health 3:284. doi:10.4172/2376-127X.1000284
Copyright: ©2016 Pinton A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Purpose: The aim of our study was to determine the risk factors and to describe the clinical presentation of women with uterine rupture without previous caesarean delivery. Methods: Case-control study involving all cases of uterine rupture in the unscarred uterus detected during labour or in the post-partum between January 1, 2004 and April 1, 2016. For the control we included four controls for one case among all the patients with no record of previous caesarean delivery and planned vaginal delivery in the same period. For each woman we collected the maternal and labour characteristics. We evaluate the risk factors of uterine rupture, using Bayesian’s method. Each result is presented as a differential with a 95% credibility interval and the probability that the difference is greater or less than 0 (or 1 for the odds ratio). Results: We identified seven cases of spontaneous rupture. Deep and variable decelerations were the most frequent abnormal fetal rhythm. There was not maternal death but one neonatal death. Multiparity (estimated difference of 1.59 (95% CI=0.55, 2.95) Pr (diff>0)=1); use of oxytocin (OR=26.4 (95% CI=1.79-103) Pr (diff>0)=0.99), induced labour (OR=14 (95% CI=2.5, 122) Pr (diff>0)=1) ultrasound macrosomia (OR 30.0 (95% CI=4.3-327) Pr (diff>0)=0.99), were associated with uterine rupture. Conclusion: Even in developed countries, uterine rupture remains a serious complication with high maternal and fetal morbidity. We identified some risk factors like multiparity, induction of labour and macrosomia. These factors can help us to detect earlier this complication.

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi