Research Article
Predictive Value of 1 Month Postoperative MRSI and FDG-PET Evaluations of Glioblastomas
| Dorra Ben Sellem1#, Waisse Waissi2#, Mojdeh Dormishian1, Caroline Bund1, Jean-Louis Dietemann3, Marie-Pierrette Chenard4, Georges Noël2 and Izzie-Jacques Namer1,5,6* | |
| 1Department of Biophysics and Nuclear Medicine, Hautepierre Hospital, University Hospital of Strasbourg , Strasbourg, France | |
| 2Department of Radiotherapy, Centre Paul Strauss, Strasbourg, France | |
| 3Department of Radiology, Hautepierre Hospital, University Hospital of Strasbourg, Strasbourg, France | |
| 4Anatomical pathology service, Hautepierre Hospital, University Hospital of Strasbourg, Strasbourg, France | |
| 5ICube, University of Strasbourg/CNRS UMR 7357, Strasbourg, France | |
| 6FMTS - Faculty of Medicine, Strasbourg, France | |
| #Authors contributed equally | |
| *Corresponding Author : | Izzie-Jacques Namer Department of Biophysics and Nuclear Medicine, Hautepierre Hospital University Hospital of Strasbourg, Strasbourg, France Tel: +33 388 127 550 Fax: +33 388 128 342 E-mail: Izzie.Jacques.NAMER@chru-strasbourg.fr |
| Received date: February 26, 2016; Accepted date: April 04, 2016; Published date: April 08, 2016 | |
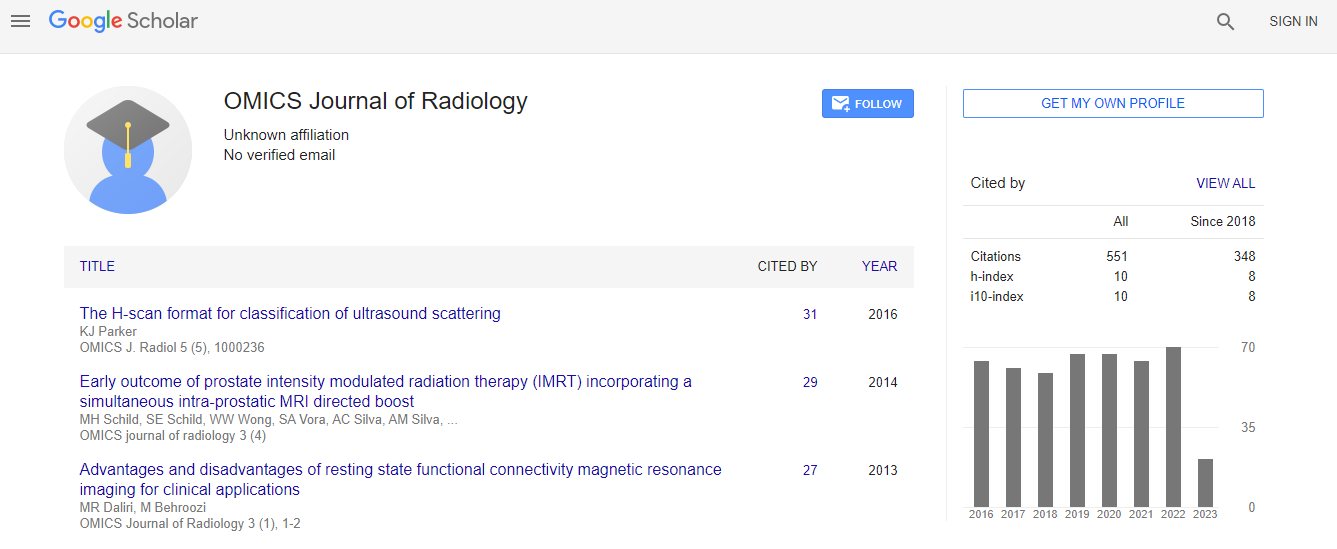
| Citation: Sellem DB, Waissi W, Dormishian M, Bund C, Dietemann JL, et al. (2016) Predictive Value of 1 Month Postoperative MRSI and FDGPET Evaluations of Glioblastomas. OMICS J Radiol 5:220. doi:10.4172/2167-7964.1000220 | |
| Copyright: © 2016 Sellem DB, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. | |
Abstract
Aim: The purpose of this study was to investigate prospectively the predictive value of positron emission tomography with proton magnetic resonance spectroscopic imaging (MRSI) and 18F-fluorodeoxyglucose (FDG-PET) performed the 1st month after surgery and before radio- chemotherapy in 43 patients with glioblastoma (GBM).
Patients and methods: Metabolite concentrations were quantified using LCModel. Overall survival (OS) and progression free survival (PFS) were calculated including all 43 patients using Kaplan-Meier curves, and the Cox proportional hazard model was used to calculate the predictor of survival.
Results: At the end of the follow-up period, all patients died within a period of 1–70.2 months. In 32 patients (74.4%), increased FDG-uptake was seen around the resection cavity and abnormal metabolic profiles on MRSI, indicative of residual disease, were present in all patients. There was no significant difference between the median OS in patients with hypometabolic FDG lesions compared to patients with hypermetabolic FDG lesions. On univariate analysis, normalized choline-containing compounds/creatine (nCho/Cr) and normalized lactate/creatine (nLac/Cr) were significantly predictive of OS and nLac/Cr and normalized N-Acetylaspartylglutamate and NAcetylaspartate/ creatine (NAA/Cr) were significantly predictive of PFS.
Conclusions: nCho/Cr and nLac/Cr ratio after surgery and before radio-chemotherapy were independent metabolic predictive factors of OS times in newly diagnosed patients with GBM.

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi