Commentary
Predictive Factors for Cesarean Delivery - A Retrospective Study
| Sónia Duarte1, Alexandra Saraiva1, Filipa Lagarto1, Maria João Susano1, Ricardo Oliveira1, Catarina S Nunes2, Pedro Pina1, Paulo Lemos1 and Humberto S Machado1* |
|
| 1Anesthesiology Department, Centro Hospitalar do Porto, Porto, Portugal | |
| 2Open University, Department of Science and Technology and Anesthesiology Department, Centro Hospitalar do Porto, Porto, Portugal | |
| Corresponding Author : | Humberto S Machado Anesthesiology Department, Centro Hospitalar do Porto Largo Abel Salazar, 4099-001 Porto, Portugal Tel: 351 935848475 Fax: 351 220900644 E-mail: hjs.machado@gmail.com |
| Received April 21, 2015; Accepted June 02, 2015; Published June 04, 2015 | |
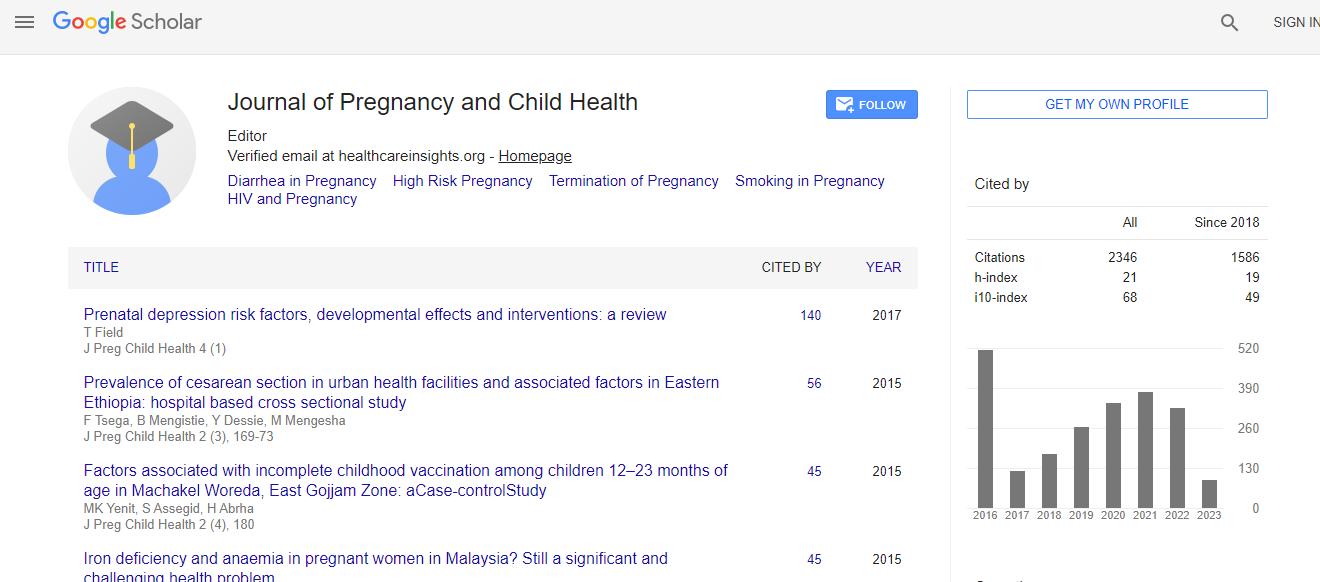
| Citation: Duarte S, Saraiva A, Lagarto F, Susano MJ, Oliveira R, et al. (2015) Predictive Factors for Cesarean Delivery – A Retrospective Study. J Preg Child Health 2:170. doi: 10.4172/2376-127X.1000170 | |
| Copyright: © 2015 Duarte S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. | |
Abstract
Background: Cesarean section rates have risen markedly worldwide. Considering the potential harm caused by this mode of delivery, and the general concern in reducing its incidence, it would be useful to individualize the risk of non-planned cesareans, and if there is any possibility, reduce that risk, and anesthesiologists should take part of this risk evaluation. In recent studies, many factors have been related with a higher risk of cesarean, and controversy still surrounds labor analgesia impact on cesarean risk. The aim of this study was to search for predictive factors for nonplanned cesarean delivery. Methods: Retrospective analysis of all labors occurred in our Obstetric Department during 2014. Maternal related factors, previous obstetric history, birth weight and factors related to labor analgesia and labor progression were studied. Our primary outcome was cesarean delivery. Results: We identified two independent predictive factors for cesarean delivery: birth weight (p=0,007 OR= 1,001 CI 95% [1,0003; 1,002]) and labor length since beginning of analgesia (p<0,0001 OR= 1,00005 CI 95%[1,00003; 1,00007]). Searching correlation between registered variables, maternal body mass index was positively associated with newborn birth weight (p<0.0001, R=0.157). Conclusion: Our study showed that birth weight and labor length since beginning of epidural analgesia are independent predictor factors of non-planned cesarean delivery. Furthermore, birth weight was associated with maternal body mass index, providing health professionals a modifiable factor in which we can intervene to improve outcome. As labor progression to cesarean is of major obstetric and anesthetic concern, multidisciplinary initiatives are warranted to clearly identify important variables concurring to operative delivery.

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi