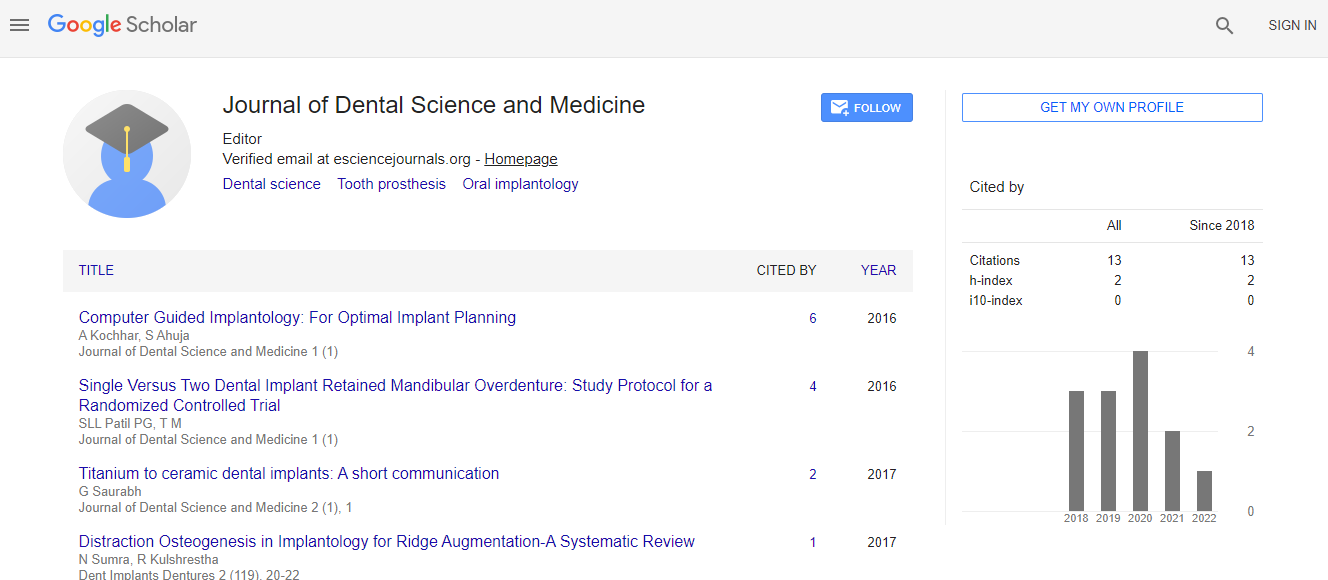
Photobiomodulation for Dental Extractions: Enhancing Postoperative Pain Relief and Accelerating Wound Healing
*Corresponding Author: James Ding, Dental Materials Science, Division of Applied Oral Sciences & Community Dental Care, Hong Kong SARReceived Date: Nov 03, 2024 / Published Date: Nov 30, 2024
Citation: James D (2024) Photobiomodulation for Dental Extractions: Enhancing Postoperative Pain Relief and Accelerating Wound Healing. J Dent Sci Med 7: 279.DOI: 10.4172/did.1000279
Copyright: © 2024 James D. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Dental extractions, whether for impacted wisdom teeth or tooth decay, often result in postoperative complications such as pain, swelling, and delayed healing. Photobiomodulation (PBM) therapy has recently garnered attention as an effective modality for enhancing the healing process and alleviating pain following dental procedures, including extractions. This review aims to explore the efficacy of PBM in reducing postoperative pain and promoting wound healing in patients undergoing dental extractions. We examine the mechanisms underlying PBM, the evidence from clinical studies, and its potential benefits in clinical dentistry. Furthermore, the safety and practicality of PBM therapy in routine dental practice are discussed, along with future perspectives for its broader application in oral surgery

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi