Research Article
Parent and Provider Decision-Making for Infants with Hypoxic-Ischemic Encephalopathy
| Allen KA1*, Brandon DH2,3, Holditch-Davis D2, Cotten CM3, Docherty SL2,3 | |
| 1Department of Biobehavioral Nursing and Health Science, University of Washington, School of Nursing, USA | |
| 2Duke University School of Nursing, Duke University, Department of Pediatrics, School of Medicine, USA | |
| 3Department of Pediatrics, Duke University, School of Medicine, USA | |
| Corresponding Author : | Kimberly A. Allen University of Washington School of Nursing, USA Tel: 312-355-5182 E-mail: kimberly.allen2@gmail.com |
| Received July 14, 2014; Accepted August 14, 2014; Published August 20, 2014 | |
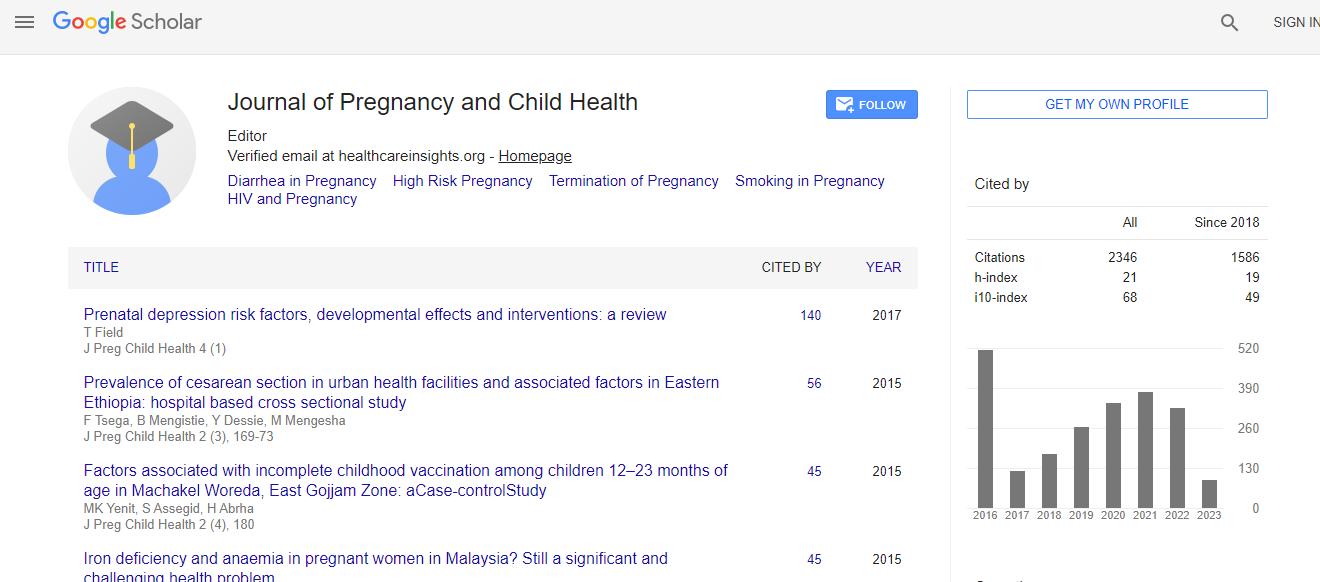
| Citation: Allen KA, Brandon DH, Holditch-Davis D, Cotten CM, Docherty SL (2014) Parent and Provider Decision-Making for Infants with Hypoxic-Ischemic Encephalopathy. J Preg Child Health 1:106. doi: 10.4172/2376-127X.1000106 | |
| Copyright: © 2014 Allen KA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. | |
Abstract
Background: Hypoxic ischemic encephalopathy (HIE) is one of the most serious complications of full term birth that can lead to long-term neurological consequences or death. Parents and providers are faced with making complex decisions about which therapies to pursue within hours of birth.
Purpose: The purpose of this study was to describe the decisions made for infants with HIE, who participated in the decision-making process, and what factors influenced the decision-making process.
Design: A longitudinal, prospective, multiple case study design was used to study infant illness trajectories and parental responses (parental distress and hope) associated with caring for infants with HIE.
Results: Two groups of parent decision-making emerged: standard care and experimental care. The decisionmaking groups appear to be dictated by the treatment the infants received within hours of birth. Parents within each group shared specific responses including similar hope and distress, which continued over the first 2 postnatal months.
Conclusions: The results indicate that the type of medical therapy the infant receives determines the level of parental participation in decision-making. In the group of parents, in which providers obtained consent for study interventions parents had less hope for their infant even though the infant had a lower severity of illness compared to the infants receiving standard therapies. The reverse was true for parents of infants receiving standard therapy, parents were more hopeful even though their infants had a higher severity of illness.

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi