Mini Review
Ophthalmic Artery Flow and Cognitive Performance in Patients with Carotid Artery Stenosis
Kuo Lun Huang1,2, Meng Yang Ho1,3 and Tsong-Hai Lee1,2*1Stroke Center and Department of Neurology, Linkou Chang Gung Memorial Hospital, Taoyuan, Taiwan
2College of Medicine, Chang Gung University, Taoyuan, Taiwan
3Clinical Psychology Program, Department of Occupational Therapy, Chang Gung University, Taoyuan, Taiwan
- *Corresponding Author:
- Tsong Hai Lee
Stroke Center and Department of Neurology
Linkou Chang Gung Memorial Hospital, 5
Fuxing Street, Guishan, Taoyuan
33305 Taiwan
Tel: +886 3 3281200
Fax: +886 3 328 7226
E-mail: thlee@adm.cgmh.org.tw
Received date: June 21, 2017; Accepted date: July 07, 2017; Published date: July 14, 2017
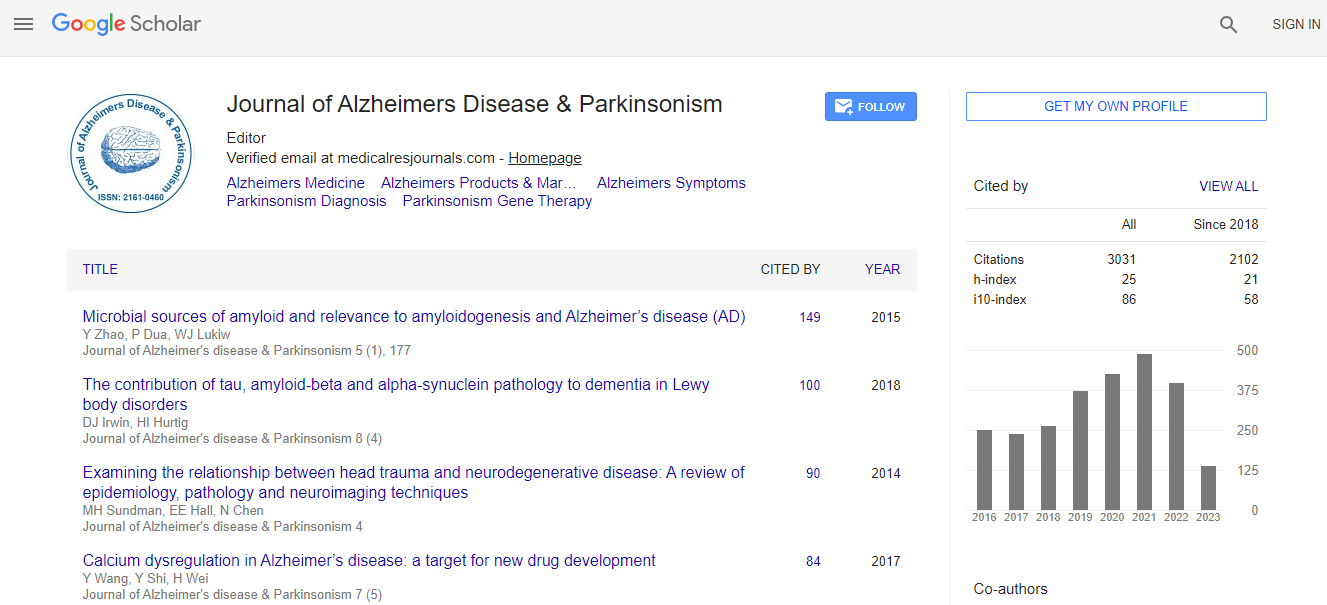
Citation: Huang KL, Ho MY, Lee TH (2017) Ophthalmic Artery Flow and Cognitive Performance in Patients with Carotid Artery Stenosis. J Alzheimers Dis Parkinsonism 7:350. doi:10.4172/2161-0460.1000350
Copyright: © 2017 Huang KL, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
The circle of Willis is regarded as the primary collaterals in patients with severe carotid artery stenosis (CAS), while the secondary collaterals from the reversed ophthalmic artery (OA) flow would be recruited when the primary collaterals are inadequate to maintain cerebral perfusion. Even though some reports suggest patients with reversed OA flow are more vulnerable to cerebral ischemic injury, whether reversed OA flow is adequate to maintain cognitive function or can be employed as a surrogate marker of cognitive impairment remains elusive. The purpose of this article is to review the dynamic behavior of collateral flow and to assess the relationship between OA hemodynamics, cerebral perfusion and cognitive performance in patients with CAS. There is evidence that the OA flow patterns behave dynamically according to the hemodynamic, metabolic, and neural demands. Patients with reversed OA flow have compensatory increased cerebral blood volume and timerelated perfusion parameters, while cerebral blood flow usually remains unchanged. Despite of the evidence having been scarce, the associations between hemodynamics of OA flow and cognitive performance have been observed in several recent studies. Furthermore, our previous study demonstrated a tendency for specific cognitive impairment observed in patients with reversed OA flow, depending on the side of reversed OA flow. However, the impacts of the OA flow patterns on cognition may be modified when the other pathogenic factors of stroke are taken into account. Concurrent application of multimodality neuroimaging findings about perfusion status and neural activities will greatly enhance our understanding of the relationships between the hemodynamics of OA flow and cognition.

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi