Research Article
Neurotoxin-Induced Catecholaminergic Loss in the Colonic Myenteric Plexus of Rhesus Monkeys
Jeanette M Shultz1, Henry Resnikoff2, Viktorya Bondarenko2, Valerie Joers2, Andres Mejia2, Heather Simmons2 and Marina E Emborg3*1Wisconsin National Primate Research Center (WNPRC) and Cellular and Molecular Pathology (CMP) Graduate Program, University of Wisconsin-Madison, Madison, WI, USA
2WNPRC, University of Wisconsin-Madison, Madison, WI, USA
3WNPRC, CMP Graduate Program and Department of Medical Physics, University of Wisconsin-Madison, Madison, WI, USA
- *Corresponding Author:
- Marina Emborg
Wisconsin National Primate Research Center
University of Wisconsin–Madison, 1220 Capitol Court
Madison, WI, USA, 53715
Tel: 608-262-9714
E-mail: emborg@primate.wisc.edu
Received date: August 10, 2016; Accepted date: October 27, 2016; Published date: November 03, 2016
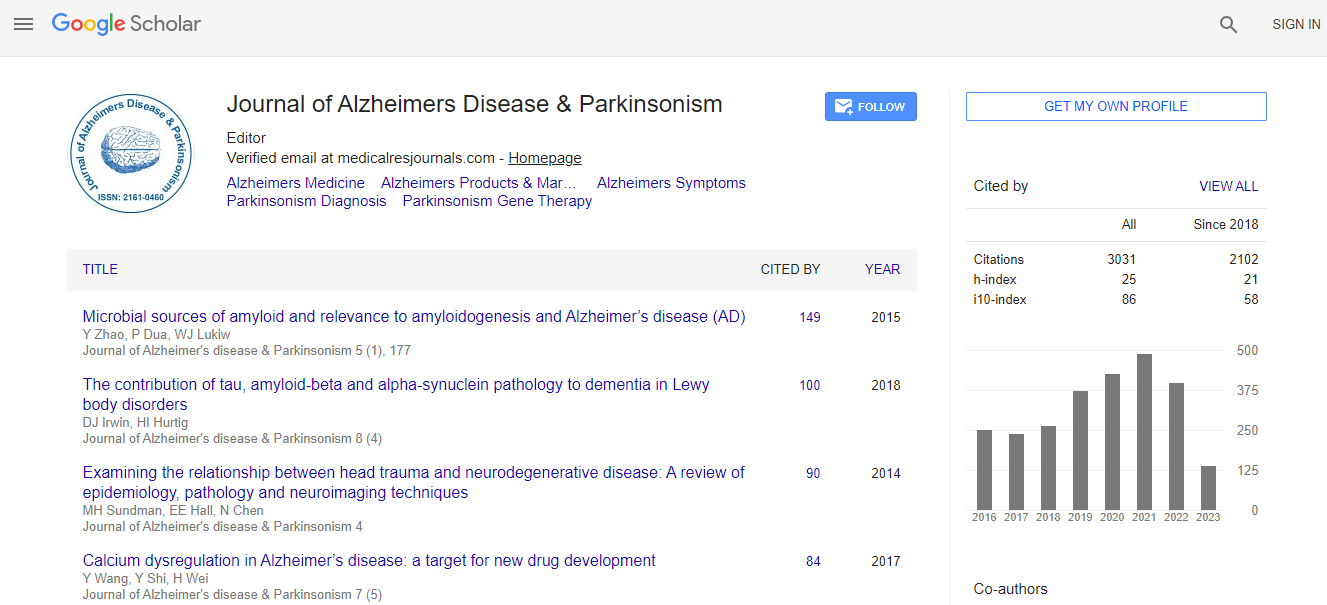
Citation: Shultz JM, Resnikoff H, Bondarenko V, Joers V, Mejia A, et al. (2016) Neurotoxin-Induced Catecholaminergic Loss in the Colonic Myenteric Plexus of Rhesus Monkeys. J Alzheimers Dis Parkinsonism 6:279. doi:10.4172/2161-0460.1000279
Copyright: © 2016 Shultz JM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Objective: Constipation is a common non-motor symptom of Parkinson’s disease (PD). Although pathology of the enteric nervous system (ENS) has been associated with constipation in PD, the contribution of catecholaminergic neurodegeneration to this symptom is currently debated. The goal of this study was to assess the effects of the neurotoxin 6-hydroxydopamine (6-OHDA) on the colonic myenteric plexus and shed light on the role of catecholaminergic innervation in gastrointestinal (GI) function. Methods: Proximal colon tissue from 6-OHDA-treated (n=5) and age-matched control (n=5) rhesus monkeys was immunostained and quantified using ImageJ software. All animals underwent routine daily feces monitoring to assess for constipation or other GI dysfunction. Results: Quantification of tyrosine hydroxylase (TH) and aromatic L-amino acid decarboxylase (AADC)- immunoreactivity (-ir) revealed significant reduction in myenteric ganglia of 6-OHDA-treated animals compared to controls (TH-ir: 87.8%, P<0.0001; AADC-ir: 61.7% P=0.0034). Analysis of pan-neuronal markers (PGP9.5, HuC/D), other neurochemical phenotypes (VIP, nNOS), PD-associated pathology proteins (α-synuclein, phosphorylated α-synuclein), glial marker GFAP and neuroinflammation and oxidative stress (HLA-DR, CD45, Nitrotyrosine) did not show significant differences. Monitoring of feces revealed frequent (>30% days) soft stool or diarrhea in 2 of the 5 6-OHDA-treated animals and 0 of the 5 control animals during the 2 months prior to necropsy, with no animals exhibiting signs of constipation. Conclusion: Systemic administration of 6-OHDA to rhesus monkeys significantly reduced catecholaminergic expression in the colonic myenteric plexus without inducing constipation. These findings support the concept that ENS catecholaminergic loss is not responsible for constipation in PD.

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi