Research Article
Late Entry into Antenatal Care in a Southern Rural Area of Vietnam and Related Factors
Ngo Thi-Thuy-Dung1,4*, Nguyen Ha-Duc2, Truong Quang-Dinh2, Nguyen The-Dung1, Philippe Goyens3 and Annie Robert41Pham Ngoc Thach University of Medicine, Ho Chi Minh City, Vietnam
2Pediatric Hospital Number 2, Ho Chi Minh City, Vietnam
3Université Libre de Bruxelles, Nutrition and Métabolisme Unit and Laboratory of Pediatrics, Brussels, Belgium
4Université Catholique de Louvain, Institute of Experimental and Clinical Research, Center for Epidemiology and Biostatistics and Public Health School, Brussels, Belgium
- Corresponding Author:
- Ngo Thi-Thuy-Dung
Pham Ngoc Thach University of Medicine
Ho Chi Minh City, Vietnam
Tel: 84937157967
E-mail: dungngo.yhcd@gmail.com
Received date: May 22, 2017; Accepted date: June 05, 2017; Published date: June 10, 2017
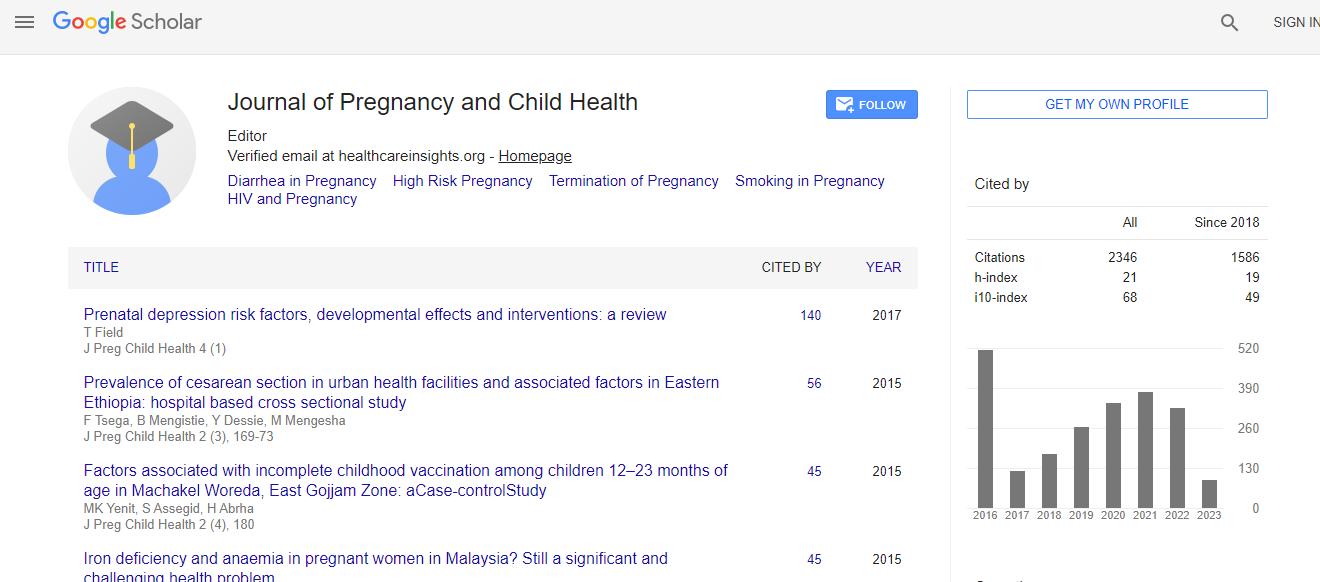
Citation: Thi-Thuy-Dung N, Ha-Duc N, Quang-Dinh T, The-Dung N, Goyens P, et al. (2017) Late Entry into Antenatal Care in a Southern Rural Area of Vietnam and Related Factors. J Preg Child Health 4: 334. doi:10.4172/2376-127X.1000334
Copyright: © 2017 Thi-Thuy-Dung N, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Aim: The aim of this study were to assess the proportion of pregnant women who attended ANC late in pregnancy and to identify factors associated with late entry in communities in South Vietnam. Background: Antenatal care (ANC) in Vietnam remains a problem suboptimal in Vietnam and there is limited information of on late entry into ANC. A study conducted in 2008 in the North of Vietnam showed 2.8% of late entry into ANC in 2.8% of women in an urban area, against versus 30.9% of women in a rural area. The aims of the present study were to assess the proportion of pregnant women attending ANC late in their pregnancy and to identify factors associated with late entry in ANC in rural communities of South Vietnam in 2014. Methods: This community-based study enrolled 1,448 pregnant women who were identified by 72 village health workers in 17 communities. First initiation to ANC after first trimester of pregnancy was considered as a late entry. Related factors were selected and analysed based on the Andersen Health Seeking Behaviour model. Multivariate logistic regression was used to identify independent factors associated with late ANC. Results: The prevalence of late ANC attendance was 8.2%. Having a poverty certificate (26.9%), having a history of abortion (19.4%), living in an ethnic minority community (17.2%) and being a teenager (15.5%) were the factors associated with late entry into ANC for pregnant women. Conclusion: The proportion of pregnant women entering late into ANC in rural Southern Vietnam remains higher than in urban areas (8.2% vs. 2.8%). Health education on the importance of attending ANC early should focus on poor people, on women who have an abortion history, on ethnic minorities, and on teenagers to promote significant early entry into antenatal care, thus improving maternal and child health.

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi