Review Article
Iron Deficiency and Anaemia in Pregnant Women in Malaysia - Still a Significant and Challenging Health Problem
| Nils Milman* | |
| Departments of Clinical Biochemistry and Obstetrics, Naestved Hospital, University of Copenhagen, Naestved, Denmark | |
| Corresponding Author : | Nils Milman Lindevangen 87B DK-2830 Denmark Tel: +45 20103577 Fax: +45 32719401 E-mail: nils.milman@webspeed.dk |
| Received April 08, 2014; Accepted May 22, 2015; Published May 27, 2015 | |
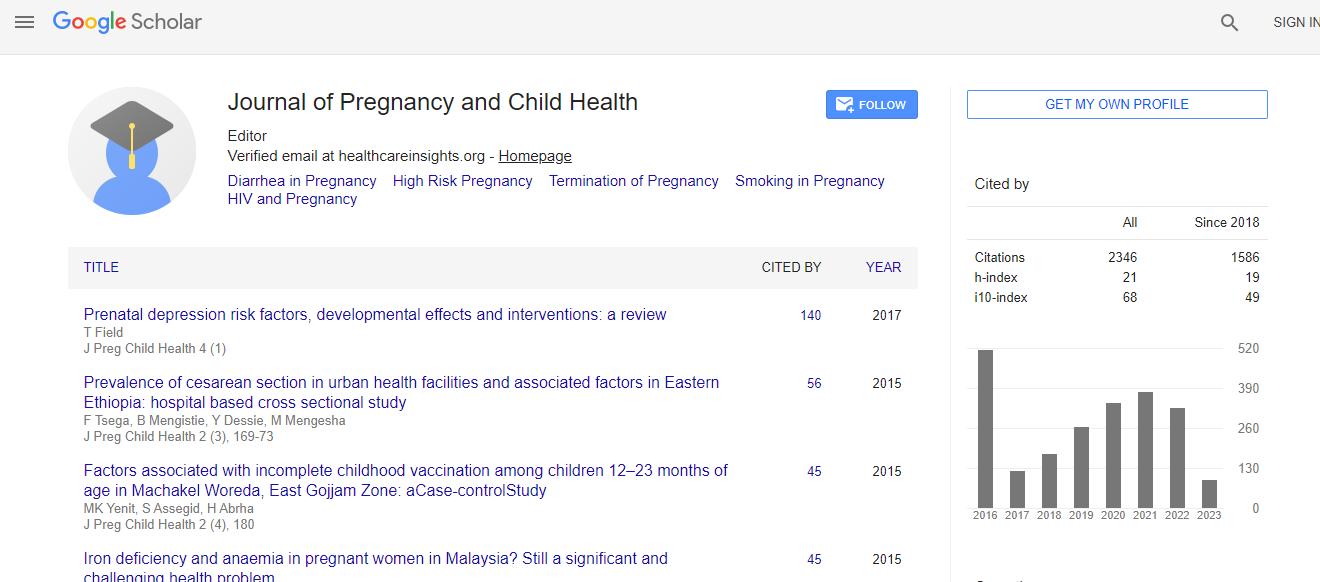
| Citation: Milman N (2015) Iron Deficiency and Anaemia in Pregnant Women in Malaysia – Still a Significant and Challenging Health Problem. J Preg Child Health 2:168. doi: 10.4172/2376-127X.1000168 | |
| Copyright: © 2015 Milman N, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. | |
Abstract
Background: Iron deficiency (ID) is the most frequent cause of anaemia (IDA) in women of reproductive age and pregnant women. Recommended cut-off value for anaemia in women of reproductive age is haemoglobin (Hb) <12.0 g/dL and in pregnancy Hb <11.0 g/dL. Serum ferritin <15-20 μg/L is consistent with ID; Hb below cut-off values and ferritin <12-15 μg/L is consistent with IDA. Methods: Literature survey on publications and guidelines on the frequency of ID and IDA in Malaysia compared with Western countries. Results: Prevalence of anaemia in women of reproductive age is ~30% and in pregnant women ~40%. With advancing pregnancy the frequency of anaemia increases, due to deficiency of iron and hematinic vitamins (folate, vitamin B12). Iron demands in pregnancy cannot be fulfilled by dietary iron intake but require oral iron supplementation. If the mother has IDA, the newborn has a high risk of ID and IDA. ID and IDA have multiple negative effects in both infants and adults. Oral iron prophylaxis should start at 10-12 weeks gestation. Among pregnant women in Malaysia 80-90%, have low iron status and 38-42% develop anaemia. Consequently, the prophylactic oral iron dose should be 100 mg ferrous iron/day. IDA is treated with oral ferrous iron 180-200 mg/day and Hb should be checked after 2-3 weeks. If there is no increase in Hb, due to poor compliance and/or impaired iron absorption, or the anaemia is severe (Hb <8.0 g/dL) treatment with intravenous iron is indicated. Conclusions: In Malaysia, anaemia in pregnant women still constitute a major and challenging health problem. We are aware of the causes for anaemia and we know the solutions, so efforts should focus on better implementation of early oral iron and vitamin prophylaxis, early diagnosis of anaemia, and on increasing the low compliance of the women to the prophylaxis programs.

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi