Case Report
Immune Reconstitution Inflammatory Syndrome (IRIS) in a Child with Disseminated Tuberculosis
Ba ID*, Thiongane A, Ba A, Faye PM, Sow A, Deme/Ly I and Ba MDepartment of Pediatric Pulmonology, University Cheikh Anta Diop of Dakar, BP 16109 Dakar-Fann, Senegal
- *Corresponding Author:
- Idrissa Demba BA
M.D. Pediatric Pulmonology
University Cheikh Anta Diop of Dakar
BP 16109 Dakar-Fann
Senegal
Tel: (+221)777647125
E-mail: docteuridy@hotmail.com
Received date: August 31, 2015; Accepted date: September 25, 2015; Published date: October 5, 2015
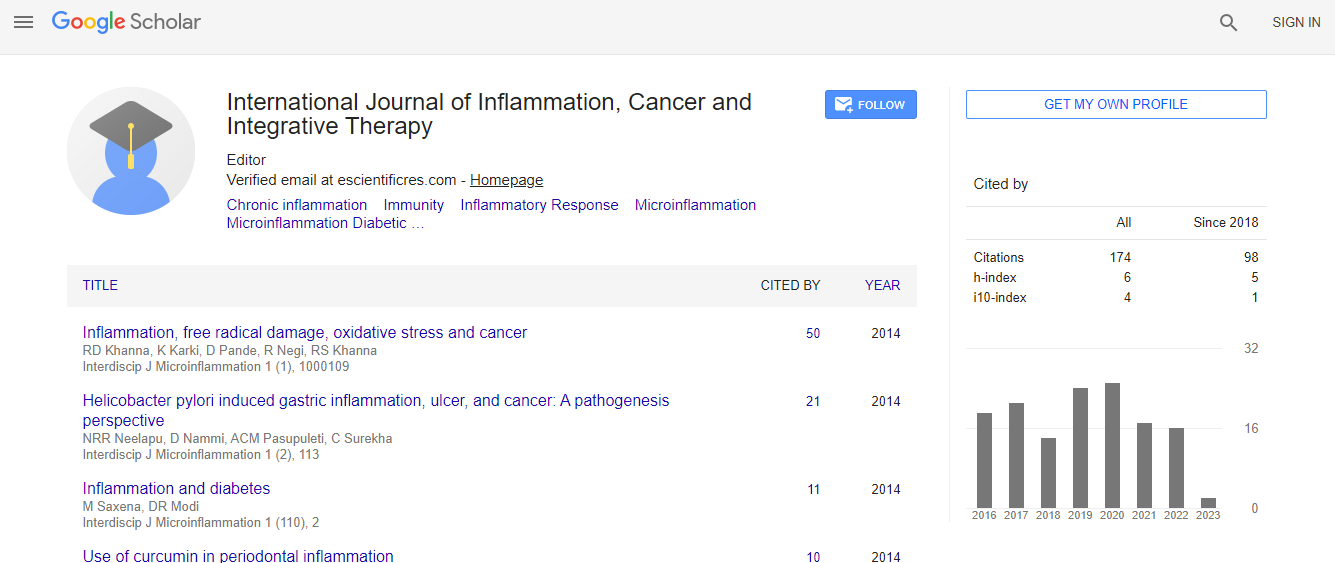
Citation: Ba ID, Thiongane A, Ba A, Faye PM, Sow A, et. al (2015) Immune Reconstitution Inflammatory Syndrome (IRIS) in a Child with Disseminated Tuberculosis. Interdiscip J Microinflammation 3:134. doi: 10.4172/2381-8727.1000134
Copyright: © 2015 Ba ID et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
IRIS is a paradoxical reaction occurring in HIV-infected patient after initiation of highly active antiretroviral therapy (HAART). Incidence is estimated 12 to 19% of child starting HAART. IRIS with tuberculosis in non-HIV patients has not been reported in the literature. We report the case of an HIV negative 8 years-old girl who did develop IRIS and dilated cardiomyopathy during her treatment for severe disseminated TB (lungs, mediastinal lymph nodes, spleen, liver and kidneys). An appropriate antibiotic treatment was begun against the multiple sensitive mycobacterium tuberculosis strain retrieved: RHZE for 2 months followed by RH 10 months. The child appeared stable the 2 first weeks on treatment but not apyretic. She remained in the hospital for 6 months and experienced daily recurrent fever 39-40°C with rigors, diffuse bone pains, elevated transaminases and deterioration of chest infiltrates. Sequential abdominal CT and Gallium scans demonstrated a progressive involvement of liver, spleen, kidneys, medullar bones and abdomen lymph nodes for 2 weeks to 5 months. Then she gradually improved. Her complete immunological work-up at that point was considered normal. We concluded from an extensive review of the literature that this case highlights a paradoxical immune mediated reaction to Mycobacterium tuberculosis during an appropriate anti-TB treatment. IRIS results in clinical deterioration but is not a failure to treatment. Early recognition of IRIS could prevent unnecessary changes in anti-TB regimen.

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi