Research Article
Illicit and Prescription Opiate Dependence: The Impact of Axis II Psychiatric Comorbidity on Detoxification Outcome
Sarah Coupland, Ronald Fraser, Jorge Palacios-Boix, Dara A Charney, Juan-Carlos Negrete and Kathryn J Gill*Addictions Unit, McGill University Health Centre and the Department of Psychiatry, McGill University, Montreal, Canada
- Corresponding Author:
- Kathryn Gill Ph.D.
Addictions Unit, McGill University Health Centre
1547 Pine Avenue West, Montreal, Quebec, Canada, H3G 1B3
Tel: 514 934 1934, ext 42395
Fax: 514 934 8262
E-mail: kathryn.gill@mcgill.ca
Received date: January 19, 2014; Accepted date: April 28, 2014; Published date: April 30, 2014
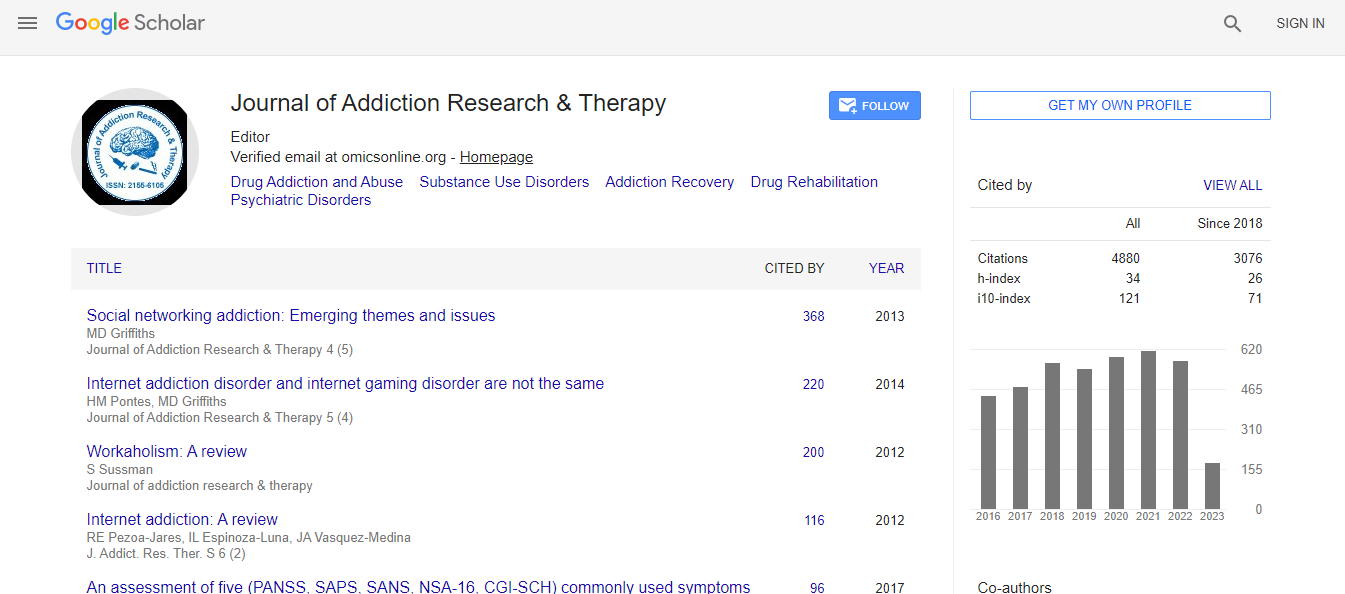
Citation: Coupland S, Fraser R, Palacios-Boix J, Charney DA, Negrete JC, et al. (2014) Illicit and Prescription Opiate Dependence: The Impact of Axis II Psychiatric Comorbidity on Detoxification Outcome. J Addict Res Ther S10:008.doi:10.4172/2155-6105.S10-008
Copyright: © 2014 Coupland S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Objective: The current study examined the predictors of inpatient detoxification failure among illicit and prescription opiate dependent patients. Outcomes for the treatment of opiate dependence were compared to those with sedativehypnotic dependence.
Methods: Data from 203 consecutive detoxification admissions included results of urine toxicology screens, length of stay, and outcomes. All detoxification protocols were designed to manage withdrawal throughout the tapering process and medical/psychiatric monitoring was provided daily.
Results: Opiate-dependent patients were significantly less likely to complete detoxification and more likely to dropout against medical advice or to be discharged for non-compliance compared to sedative-hypnotic dependent patients. Those with opiate dependence were also more likely to be polysubstance abusers, and to report that they suffered some form of chronic pain syndrome (e.g. fibromyalgia) compared to the non-opiate group. Additionally, a large percentage of the sample was diagnosed with a personality disorder (PD), primarily Cluster B PD. There was considerable overlapping comorbidity between PD, pain syndromes and opiate abuse; 31.6% of the opiate-dependent patients suffered from both a chronic pain condition and a PD compared to 4.0% of the non-opiate patients. A hierarchical logistic regression revealed that treatment failure was predicted by three significant variables – younger age, opiate dependence and the presence of a Cluster B personality disorder. Illicit opiate (IO) users differed significantly from prescription opiate (PO) users in that they were significantly younger at first use of opiates and at the time of detoxification. Time between first use and detoxification admission did not significantly differ between the groups and rates of detoxification completion were comparable.
Conclusions: Overall, these findings suggest a complex interaction between opiate dependence, pain syndromes, and affective dysregulation, which may lead to early termination from treatment.Further understanding of treatment failure may lead to specific, targeted interventions for thisdifficult to treat population.

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi