High Platelet-Lymphocyte Ratio may Predict Poor Therapeutic Response in Breast Cancer Patients Treated with Neoadjuvant Chemotherapy
*Corresponding Author:Received Date: Dec 10, 2024 / Published Date: Jan 09, 2024
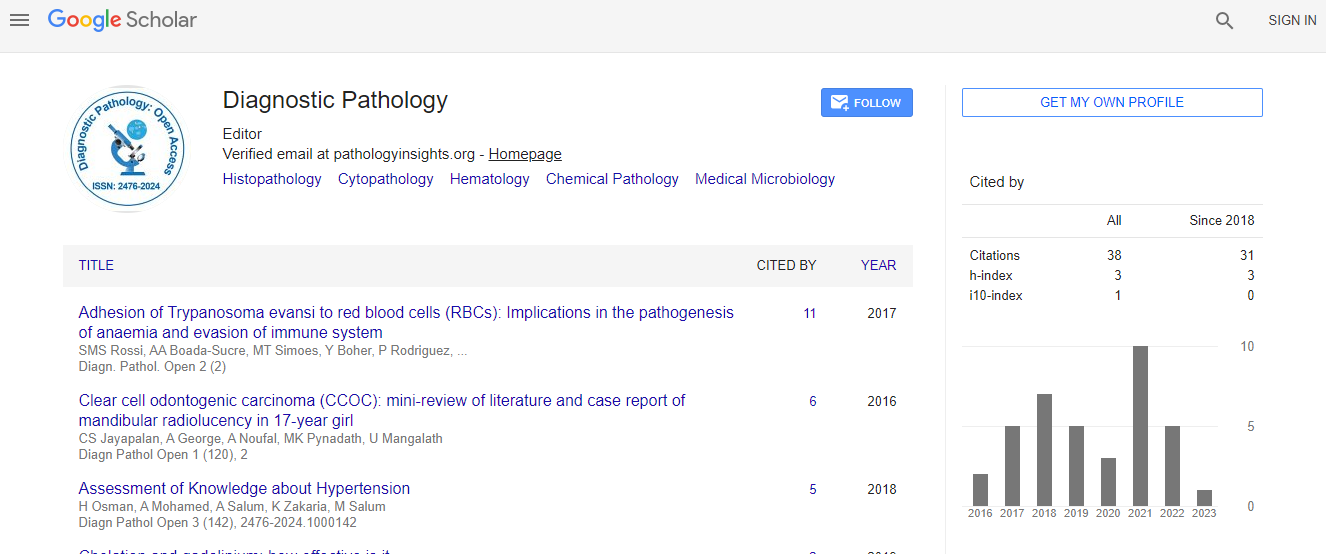
Citation: Wang W, Chen H, Zhao R, Yao Y (2024) High Platelet-Lymphocyte Ratio may Predict Poor Therapeutic Response in Breast Cancer Patients Treated with Neoadjuvant Chemotherapy. Diagnos Pathol Open 9:243
Copyright: © 2024 Wang W, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited
Abstract
Abstract Background: To investigate the correlation between Blood Inflammatory Markers (BIMs), including Neutrophil to Lymphocyte Ratio (NLR), Monocyte to Lymphocyte Ratio (MLR) and Platelet to Lymphocyte Ratio (PLR), and the efficacy of Neoadjuvant Chemotherapy (NACT) in BC patients. Besides, the relationship between Tumor Infiltrating Inflammatory cells (TIIs) and BIMs has also been preliminarily studied. Methods: A total of 315 BC patients between January 2018 and September 2022 were recruited. Receiver operating characteristic curve was used to determine the cut-off value of each BIM. Logistic regression analysis was used to evaluate the predictive power of BIMs for pathological Complete Response (pCR). TIIs were assessed by immunohistochemistry and their relationships with BIMs also were analyzed. Results: NLR, MLR, PLR in the pCR group were significantly lower than those in the non-pCR group after NACT (p ≤ 0.05). PLR had the largest Area Under the Curve (AUC) (0.73) compared to NLR (0.57) and MLR (0.67) (p< 0.01). Univariate analysis showed ER, PR, HER2, NLR, MLR, PLR were significantly associated with pCR, but multivariate analysis found only HER2 and PLR were independently predictors for pCR (p<0.01). PLR was positively correlated with the expression of P-selectin in tumor tissue (r: 0.26, p<0.01). Survival analysis showed that NLR, MLR, PLR had no significant correlation with disease prognosis. Conclusion: PLR after NACT could serve as a predictor for pCR and it correlated with the imbalance of the tumor-infiltrating platelet to lymphocyte ratio, which might cause drug resistance.

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi