Heart Failure with Preserved Ejection Fraction (HFpEF): Unraveling the Pathophysiology, Diagnosis, and Emerging Therapeutic Strategies
*Corresponding Author: Francis R. Limkakeng, Department of Emergency Medicine, Kilimanjaro Christian Medical Centre, Tanzania, Email: francis.R.L@gmail.comReceived Date: Nov 05, 2024 / Published Date: Nov 29, 2024
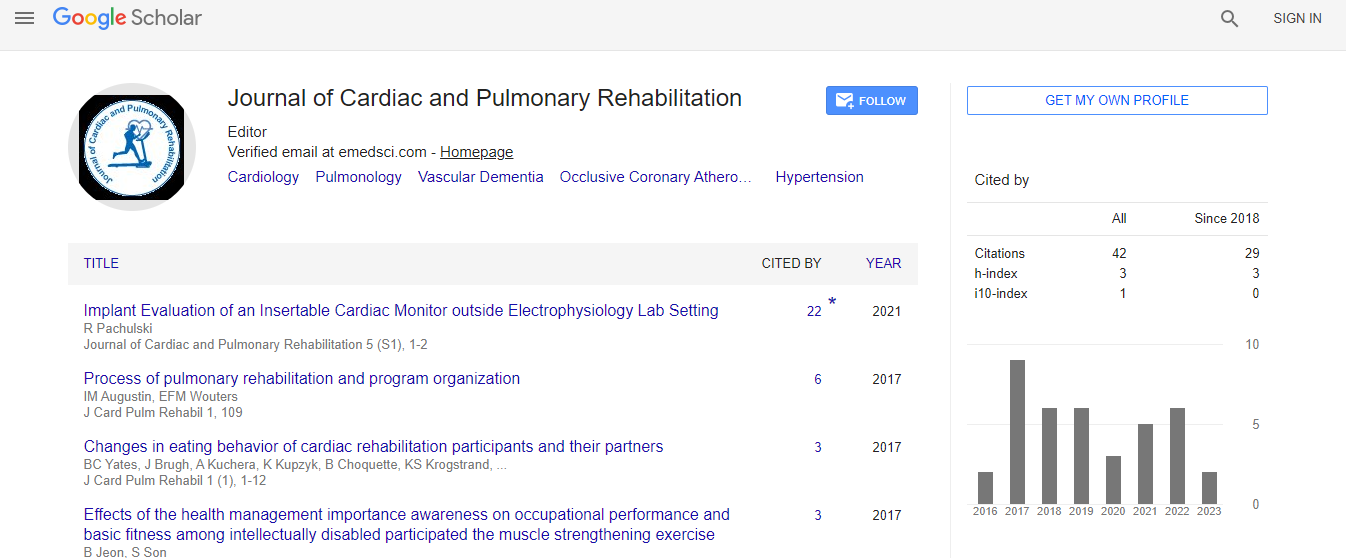
Citation: Limkakeng FR (2024) Heart Failure with Preserved Ejection Fraction (HFpEF): Unraveling the Pathophysiology, Diagnosis, and Emerging Therapeutic Strategies. J Card Pulm Rehabi 8: 294.
Copyright: © 2024 Limkakeng FR. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Heart Failure with Preserved Ejection Fraction (HFpEF) represents a complex clinical syndrome characterized by heart failure symptoms despite a normal or near-normal left ventricular ejection fraction (LVEF). This condition is increasingly recognized as a major contributor to the global burden of heart failure, particularly in the aging population. HFpEF is associated with a heterogeneous pathophysiology, including impaired ventricular relaxation, increased stiffness of the myocardium, and altered diastolic filling, often resulting from comorbidities such as hypertension, diabetes, and obesity. The diagnostic evaluation of HFpEF remains challenging due to the lack of specific biomarkers and imaging criteria. Advanced echocardiographic techniques, cardiac MRI, and biomarker profiling are helping to enhance diagnosis and risk stratification. Despite significant progress in understanding its pathophysiology, the management of HFpEF has proven difficult, with few therapies showing clear benefit. However, emerging strategies targeting key molecular pathways, including anti-fibrotic agents, vasodilators, and therapies aimed at improving diastolic function, offer hope for future treatment options. This review aims to provide a comprehensive overview of the current understanding of HFpEF's pathophysiology, diagnostic approaches, and the evolving landscape of therapeutic interventions

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi