Research Article
Factors Influencing Pregnancy Decision Making among Known HIV Positive Women of Reproductive Age in Busia County, Western Kenya
Hudson Inyangala1*, Judith A Makwali2 and Sylvia O Aluku31Jhpiego Corporation, Nairobi, Kenya - An Affiliate of Johns Hopkins University, Kenya
2University of Eldoret, Department of Biological Sciences, Kenya
3Ministry of Health, Busia County, Kenya
- *Corresponding Author:
- Hudson Inyangala
Jhpiego Corporation
Nairobi, Kenya
An Affiliate of Johns Hopkins University, Kenya
Centre for Global Research RMIT Universit,Australia
Tel: 254721727398
E-mail: hudson.inyangala@jhpiego.org
Received date: September 06, 2016; Accepted date: September 16, 2016; Published date: September 30, 2016
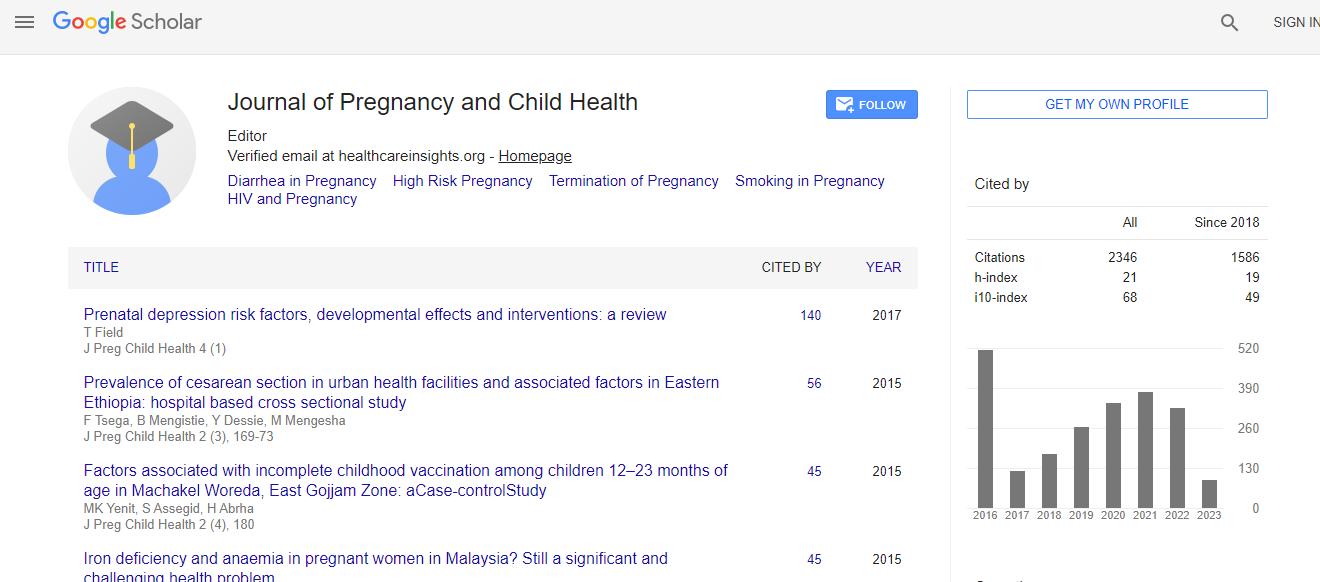
Citation: Inyangala H, Makwali JA, Aluku SO (2016) Factors Influencing Pregnancy Decision Making among Known HIV Positive Women of Reproductive Age in Busia County, Western Kenya. J Preg Child Health 3:281. doi: 10.4172/2376-127X.1000281
Copyright: © 2016 Inyangala H, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Kenya is one of the six HIV ‘high burden’ countries in Africa with about 1.6 million people living with HIV infection by 2013. Women in Kenya are more vulnerable to HIV infection compared to men, with the national HIV prevalence at 7.6% for women and 5.6% for men. There were about 1441 pregnant women living with HIV in Busia County in 2013, with an estimated 57 new paediatric infections. HIV positive mothers, have a constitutional; human right and may want to have children but the timing has to be right to minimize the chances of transmission. Aim: To establish the factors that influence pregnancy decision making amongst known HIV positive women of reproductive age in Busia County, Western Kenya. Methods: Desk review of existing PMTCT data in DHIS2, structured focused group discussions (FGDs) and health facility questionnaire based cross-sectional survey among known HIV positive pregnant women of reproductive age, and those with infants aged below 6 months attending antenatal (ANC)/PMTCT and child welfare clinics (CWC) were used. Results: Among the 128 women interviewed, 98 (77%) knew their HIV positive status prior to becoming pregnant, while 17 (13%) discovered their status at first ANC, 8 (6%) at labour and delivery and 5 (4%) at 2 weeks post-partum. Overall, the women shared similarities in their socio-demographic profile. Over 60% of the respondents were cognizant of the risk involved in getting pregnant. Regardless of women’s pregnancy experiences or intentions, considerations in pregnancy decision-making was based on desire for motherhood; religious values; stigma; attitudes of partners and health care providers. Conclusion: The younger HIV positive women, with 1 or 2 children were three times more likely to get pregnant than older ones (OR=2.67) despite their HIV positive status and the risks involved to fulfil societal concerns.

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi