Research Article
Epidural versus Intravenous Patient Controlled Analgesia after Laparoscopic Gastric Bypass Surgery
| Stefan Neuwersch1, Michael Zink2, Vanessa Stadlbauer-Köllner3 and Karl Mrak4* | |
| 1Department of Anaesthesiology and Intensive Care Medicine, General Hospital Klagenfurt, Austria | |
| 2Department of Anaesthesiology and Intensive Care Medicine, General public Hospital of the Brothers of St. John of God St.Veit/Glan, Austria | |
| 3Department of Internal Medicine, Division of Gastroenterology and Hepatology, Medical University of Graz, Austria | |
| 4Department of Surgery, Division of General surgery, Medical University of Graz, Austria | |
| *Corresponding Author : | Karl Mrak Department of Surgery, Division of General surgery Medical University of Graz,Auenbruggerplatz 29, 8036-Graz, Austria Tel: 43-316-385-81548 E-mail: karl.mrak@klinikum-graz.at |
| Received: March 25, 2016 Accepted: April 19, 2016 Published: April 22, 2016 | |
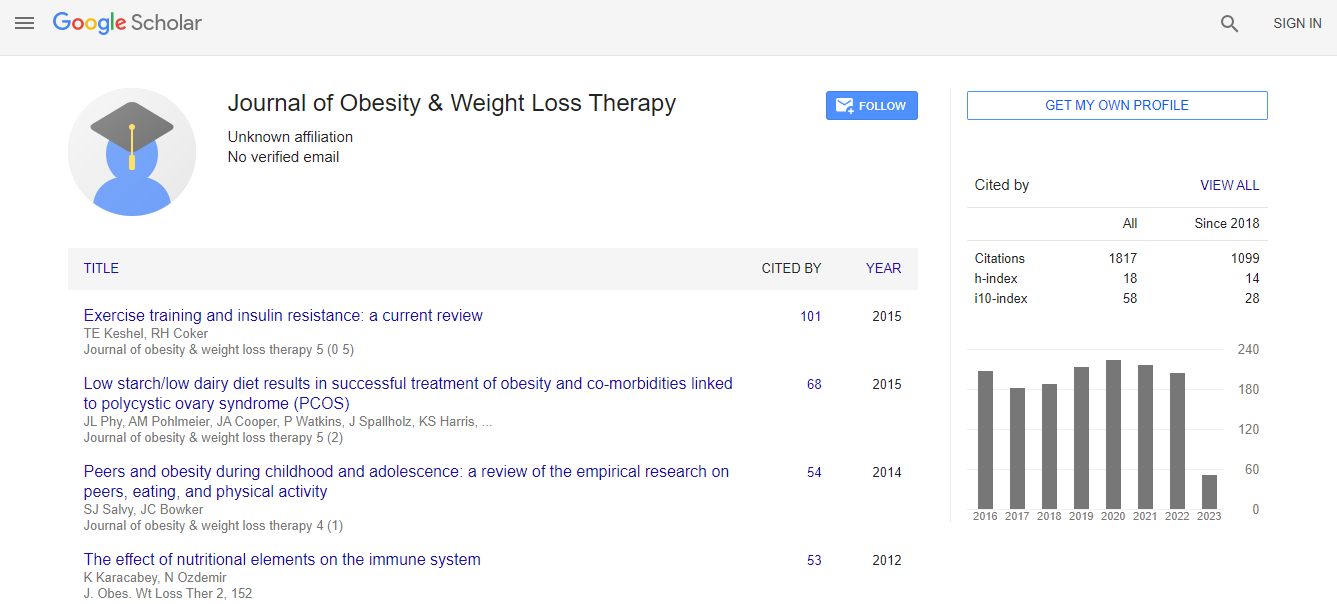
| Citation: Neuwersch S, Zink M, Stadlbauer-Köllner V, Mrak K (2016) Epidural versus Intravenous Patient Controlled Analgesia after Laparoscopic Gastric Bypass Surgery. J Obes Weight Loss Ther 6:307. doi:10.4172/2165-7904.1000307 | |
| Copyright: © 2016 Neuwersch S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. | |
Abstract
Introduction: There is no clear consensus about the optimal postoperative pain management in morbidly obese patients undergoing bariatric surgery. The aim of this study was to evaluate the effects of Patient-Controlled- Epidural-Analgesia (PCEA) compared to Intravenous-Patient-Controlled-Analgesia (IV-PCA) in patients undergoing laparoscopic gastric bypass surgery. Methods: Between January 2013 and December 2014, 154 obese patients underwent laparoscopic gastric bypass surgery. Included in our analyses were all patients receiving either IV-PCA or PCEA in their postoperative course. Group comparison with respect to patient demographics, co-morbidities, details of surgical procedure, details of postoperative course, NRS-scores at rest, and medical follow-ups were performed. Results: Overall 63 (44.4%) patients were treated by PCEA, 79 (55.6%) patients by IV-PCA. We observed no differences across the groups with respect to sex, age, ASA-score, co-morbidities, postoperative BMI, body height, pre- and postoperative weight, ideal weight, weight loss, duration of surgery and postoperative ward. Patient´s BMI (p=0.025) and excess weight before surgery (p=0.029) were significantly higher in the IV-PCA-group. Surgical complications occurred significantly more often in the IV-PCA group (p=0.045). Concerning the postoperative pain management there was no statistically significant difference between different NRS-scores throughout the study period. However, individuals in the IV-PCA-group received significantly more paracetamol (p<0.0001) and diclofenac combined with orphenadrine (p=0.003). Duration of PCA was longer in the PCEA-group compared to patients treated with IV-PCA (p<0.01). Conclusions: Particularly for obese patients, PCEA is more beneficial than IV-PCA, which is borne out by a significantly lower incidence of surgical complications observed in patients receiving PCEA.

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi