Research Article
Enhanced Recovery after Surgery for Gastric Cancer
| Boris E Sakakushev* | |
| Assistant Professor, Faculty of Medicine, Consultant Surgeon, Chair of Surgical Propedeutics, University Hospital St George Plovdiv 4002, Bulgaria | |
| Corresponding Author : | Boris E Sakakushev Assistant Professor, Faculty of Medicine Consultant Surgeon, Chair of Surgical Propedeutics University Hospital St George Plovdiv 4002, Bulgaria E-mail: bsakakushev@gmail.com |
| Received March 20, 2013; Accepted April 04, 2013; Published April 06, 2013 | |
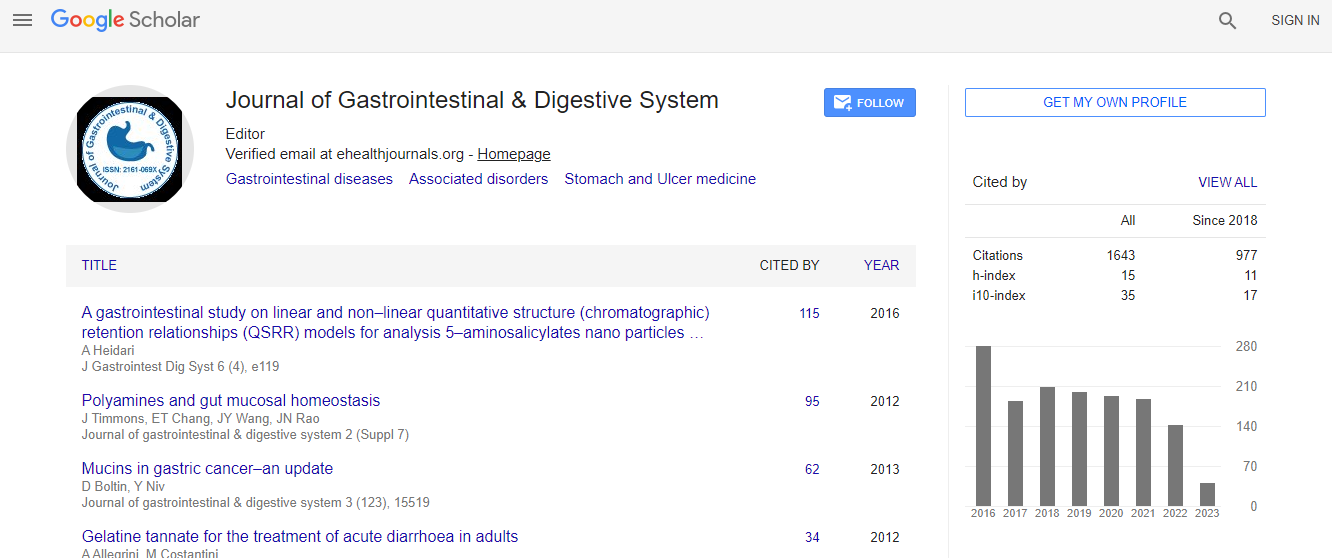
| Citation: Sakakushev BE (2013) Enhanced Recovery after Surgery for Gastric Cancer. J Gastroint Dig Syst S12:003. doi:10.4172/2161-069X.S12-003 | |
| Copyright: © 2013 Sakakushev BE. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. | |
Abstract
Introduction: While FTS programs are developing in colo-rectal surgery, in upper gastrointestinal surgery they are rare. ERAS programs can be planned and performed in gastric cancer surgery as pre-, intra- and post-operative. Materials and methods: We have studied 178 gastric cancer patients operated radically in our clinic between 2000 and 2011, comparing outcomes of surgical strategies containing FTS elements. Standard gastrectomies with D2 lymph node dissection were made: esophago-cardial resections - 32; total gastrectomies - 78, proximal gastrectomies - 21; distal gastrectomies - 47. Patient’s files were inspected for 19 perioperative indicators applicable to FT surgery. Data for abdominal complaints and early postoperative complications were also collected and analyzed. Results: Only 42 patients fulfilled the criteria for ERAS intervention, having at least 5 ERAS indicators. The most common FT elements were: lack or removing naso-gastric tube, oral intake and mobilization on postoperative day 1 - 2 and one shot AB prophylaxis. From the 8 types of complications studied, most common were: wound infection - 12.9% and anastomosis dehiscence - 4.5%. Lethality was 6.2%. Six patients died from pulmonary embolism, bronchopneumonia and heart attack. Reoperations for complications were performed in 19 patients, 5 of whom died. Mean hospital stay was - 15.2 days. Discussion and conclusions: In patients mobilized early, fed orally and deprived from nasogastric tube and urinary catheter on day 1-2, flatus and defecation appeared earlier, wound infections, pulmonary hypostasis and pneumonia rate were lower and hospital stay was less, which coincides with other reports. Usual insertion of nasogastric tubes, urinary catheters and intra-abdominal drains after gastric cancer resection should be avoided. FTS in gastrectomy for gastric cancer is safe and efficient approach, which hasten return of gut function and shorten postoperative hospital stay.

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi