Research Article
Emergency Department Intervention Program for Enhancing Choice at the End of Life: A Quality Improvement Project at a Comprehensive Cancer Center
Maria T Cruz-Carreras1*, Patrick Chaftari1, Carmen Gonzalez1, Rowena Enojo2 and Jayne Viets-Upchurch1
1Department of Emergency Medicine, The University of Texas MD Anderson Cancer Center, Houston, Texas
2Department of Emergency Center, The University of Texas MD Anderson Cancer Center, Houston, Texas
- *Corresponding Author:
- Maria T. Cruz-Carreras
Department of Emergency Medicine
The University of Texas MD Anderson Cancer Center, Houston, Texas
Tel: (713) 745-4516
Email: mcruz3@mdanderson.org
Received date: January 26, 2017; Accepted date: February 22, 2017; Published date: February 27, 2017
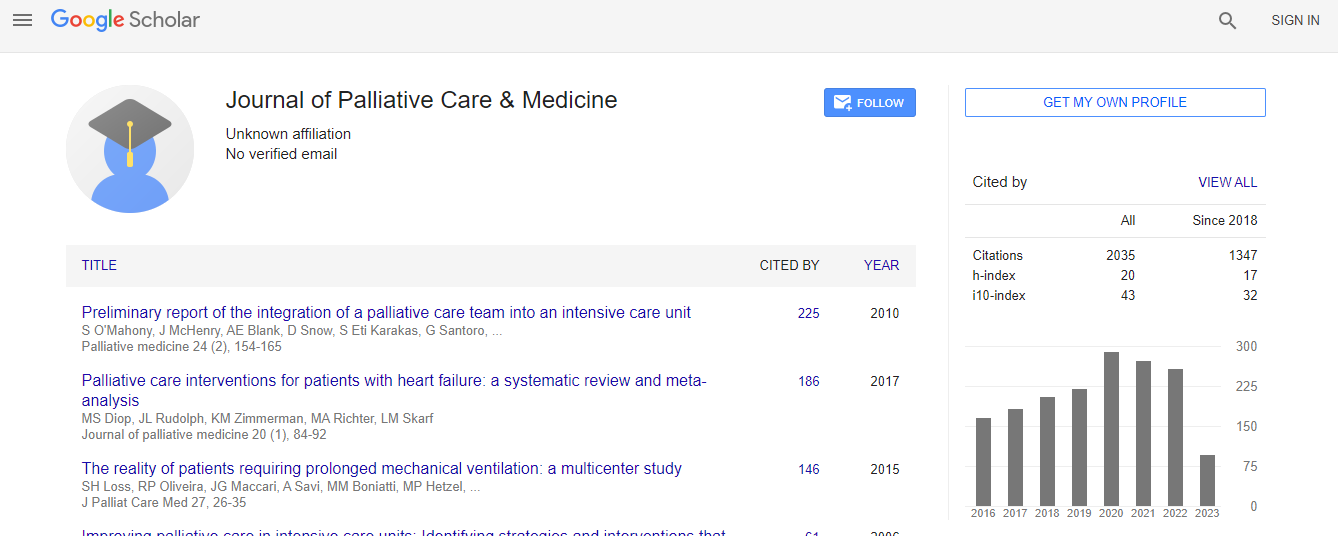
Citation: Cruz-Carreras MT, Chaftari P, Gonzalez C, Enojo R, Viets-Upchurch J (2017) Emergency Department Intervention Program for Enhancing Choice at the End of Life: A Quality Improvement Project at a Comprehensive Cancer Center. J Palliat Care Med 7:298. doi:10.4172/2165-7386.1000298
Copyright: © 2017 Maria, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Advance care planning (ACP) for end-of-life care is especially important for individuals with terminal illnesses such as advanced cancer. It ensures that patients’ wishes are honored and alleviates the decisionmaking burden on family members and medical providers. It reduces unnecessary medical costs, and prevents waste of valuable resources. We proposed a quality improvement project to improve documentation of advanced care directives in the Emergency Department (ED) of a tertiary cancer center.
Methods: We developed a pocket card to help emergency physicians screen patients in need of ACP. The goal was to assist ED staff in initiating conversations about end-of-life issues, and encourage patients and their caregivers to get involved in decisions about their medical treatment.
Intervention: The project was implemented in a Plan-Do-Study-Act design. Baseline data was collected from the medical records of all patients visiting the ED on seven consecutive days prior to the distribution of the pocket card tool. After the launch of the intervention, the charts of all patients visiting the emergency center were reviewed for documentation of advanced care planning. Metrics polled included presence of a health care power of attorney and determination of code status, specifically the do-not-resuscitate (DNR) status.
Results: 429 patients who visited the ED seven consecutive days prior to institution of the screening tool. Of these, we found that 66 (15.4%) had indicated their do-not-resuscitate (DNR) status in their charts, and 82 (19.1%) had a health care power of attorney. Post launch of the intervention, 391 patients visited the ED over seven consecutive days. Of these, 125 (32.0%) indicated their DNR status in their charts before leaving the ED, and 95 (24.3%) had a health care power of attorney. After implementation of our screening tool, there was a 107.8% increase in documentation of DNR status and a 76% increase in patients with a health care power of attorney.
Conclusions: In this quality improvement project, a straightforward, low cost intervention was successfully implemented to improve documentation of patients’ ACP goals.

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi