Differences in the Epidemiology, Clinical Characteristics, Distribution of Microorganisms and Outcomes between COVID-19 Patients and Non-COVID-19 Patients with ICU-Associated BSIs: A One-Center Retrospective Study
*Corresponding Author: Cagla Keskin Saritas, Department of Infectious Diseases and Clinical Microbiology, Marmara University Training and Research Hospital, Istanbul, Turkey, Tel: 905413671351, Email: caglakeskinnn@gmail.comReceived Date: Nov 03, 2024 / Published Date: Dec 11, 2024
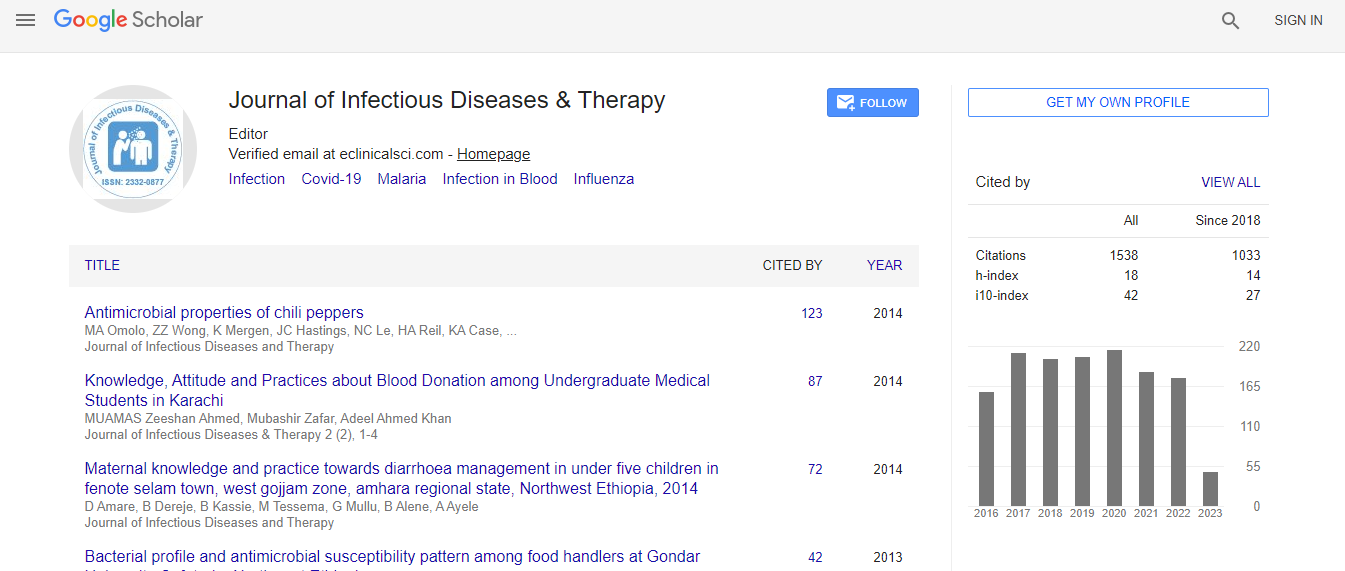
Citation: Saritaş CK, Ozsut H, Benli A, Basaran S (2024) Differences in the Epidemiology, Clinical Characteristics, Distribution of Microorganisms and Outcomes between COVID-19 Patients and Non-COVID-19 Patients with ICU- Associated BSIs: A One-Center Retrospective Study. J Infect Dis Ther S4:005.DOI: 10.4173/2332-0877.24.S4.005
Copyright: © 2024 Saritaş CK, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: We aimed to study the differences between patients with COVID-19 and non-COVID-19 ICU-associated BSIs in terms of epidemiological, clinical, microbiological and outcome data.
Methods: All patients who were followed up in the intensive care unit of a university hospital between 18th March, 2020 and 18th April, 2022 and the ICU-acquired BSI definition according to the study criteria were selected and divided into two groups: COVID-19 and non- COVID-19. In patients with multiple bacteriemia periods, only the initial period was recorded, but the active fungus was also included in the subsequent period. Descriptive statistics were used to analyze differences between patients with COVID-19 and those without COVID-19. Logistic regression analysis was applied to determine mortality risk factors in BSI patients.
Results: 234 patients were treated for ICU-acquired BSI, 127 with COVID-19 and 107 without COVID-19. Respiratory sources were significantly more common in COVID-19 patients compared to non-COVID-19 patients (43.3% vs. 26%, p ≤ 0.01). Among the causative pathogens, Acinetobacter baumannii (24.4% vs. 5.6%, p ≤ 0.01) and gram-negative Multidrug-Resistant (MDR) bacteria (81.7% vs. 61.7%, p=0.020) were detected more frequently in COVID-19 patients than in non-COVID-19 patients. The duration of antibiotic use in the hospital before BSI was longer in COVID-19 patients than in non-COVID-19 patients and this was also associated with BSI in which gram-negative MDR bacteria were active (p ≤ 0.01). Survival times after BSI were shorter in COVID-19 patients than in non-COVID-19 patients (p=0.032).
Conclusion: We showed that MDR microorganisms were prevalent in COVID-19 patients with ICU-acquired BSI and this was partly due to the length of antibiotic use in the hospital prior to BSI. Survival was lower in COVID-19 patients with BSI.

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi