Research Article
Contributions of Procalcitonin in the Treatment of Neonatal Late Onset Sepsis: A Prospective Observational Study
Aude du Mesniladelee1, Valérie Champion1, François Kieffer1, Mohamed Ali Lachtar1, Inès de Montgolfier1, Laurence Foix l’Hélias1,2 and Delphine Mitanchez1,2*
1Division of Neonatology, Department of Perinatology, Armand Trousseau Hospital, Paris
2Sorbonne University, UPMC Univ Paris, Paris, France
- *Corresponding Author:
- Delphine Mitanchez
Sorbonne University, UPMC Univ Paris, Paris, France
Tel: 331 44736191
Fax: 33144736892
E-mail: delphine.mitanchez@aphp.fr
Received date: May 26, 2016; Accepted date: May 31, 2016; Published date: June 05, 2016
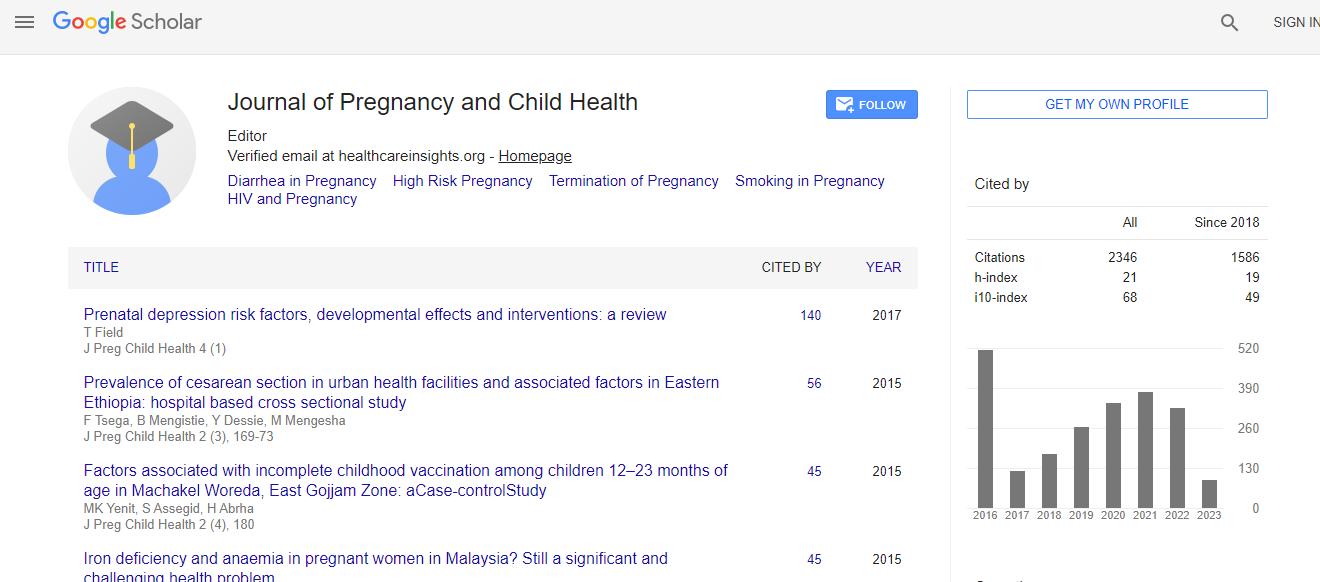
Citation: du Mesniladelee A, Champion V, Kieffer F, Lachtar MA, de Montgolfier I, et al. (2016) Contributions of Procalcitonin in the Treatment of Neonatal Late Onset Sepsis: A Prospective Observational Study. J Preg Child Health 3:256. doi:10.4172/2376-127X.1000256
Copyright: © 2016 du Mesniladelee A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Duration of antibiotic treatment in neonatal late onset sepsis is empirical. Objectives: a) To study the evolution of procalcitonin during treatment of secondary sepsis in new-borns, b) To evaluate the reduction of antibiotic exposure using its serial measurements. Methods: This single-center prospective observational study was conducted in a level II neonatology unit in the Armand Trousseau Hospital in Paris, France. All neonates hospitalized in the unit between December 2011 and January 2013 with suspected infection after 5 days of life and serum procalcitonin concentration >0.6 μg/L were included. Serial procalcitonine, C-reactive protein and blood culture survey was performed during antimicrobial therapy. Antimicrobial therapy was administered for 10 days after the last positive blood culture. Results: 54 infective episodes were observed in 46 neonates, born at a mean term of 32 weeks (range: 26-40) and infected at mean age of 19 days (7-40). Staphylococci was found in 31 infective episodes (57.4%), other microorganisms in 12 (22.2%), and none bacteria in 11 episodes (20.4%). The main cause was central line infection (85.2%). On day 5, 80% of procalcitonin measurements were <0.6 μg/L compared to 60% of C-reactive protein <5 mg/L measurements. If antimicrobial therapy had been discontinued when serum procalcitonine level was <0.6 μg/L, or the decrease from the maximal procalcitonin level was at least 80%, the duration would have been 5 days shorter. Conclusion: The use of procalcitonine in neonatal late onset sepsis as a guide to duration of treatment may limit the prescription of antibiotics. This should be further examined in a controlled study

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi