Thesis
Clinical Analysis of 65 Patients with Pancreatic Fistula and Wound Infection after Pancreatoduodenectomy (PD) with Duct-to-Mucosa Pancreaticojejunostomy: A Single-Center Report
Mohammad Abdul Mazid, Zheng Hui Ye, Xiao-Ping Geng, Fu-Bao Liu, Yi-Jun Zhao, Fan Huang, Kun Xie and Hong-Chuan Zhao*
Department of Hepatobiliary, Pancreatic Surgery and Liver Transplantation, Anhui Medical University, China
- *Corresponding Author:
- Hong-Chuan Zhao
MD, Department of Hepatobiliary
Pancreatic Surgery and Liver Transplantation
The First Affiliated Hospital of Anhui medical University
Anhui Medical University, 81 Meishan Road, Sushan District
Hefei, 230032, Anhui
China
Tel: +8613856085670
E-mail: zhc0117@sina.com
Received date: November 28, 2016; Accepted date: December 06, 2016; Published date: December 14, 2016
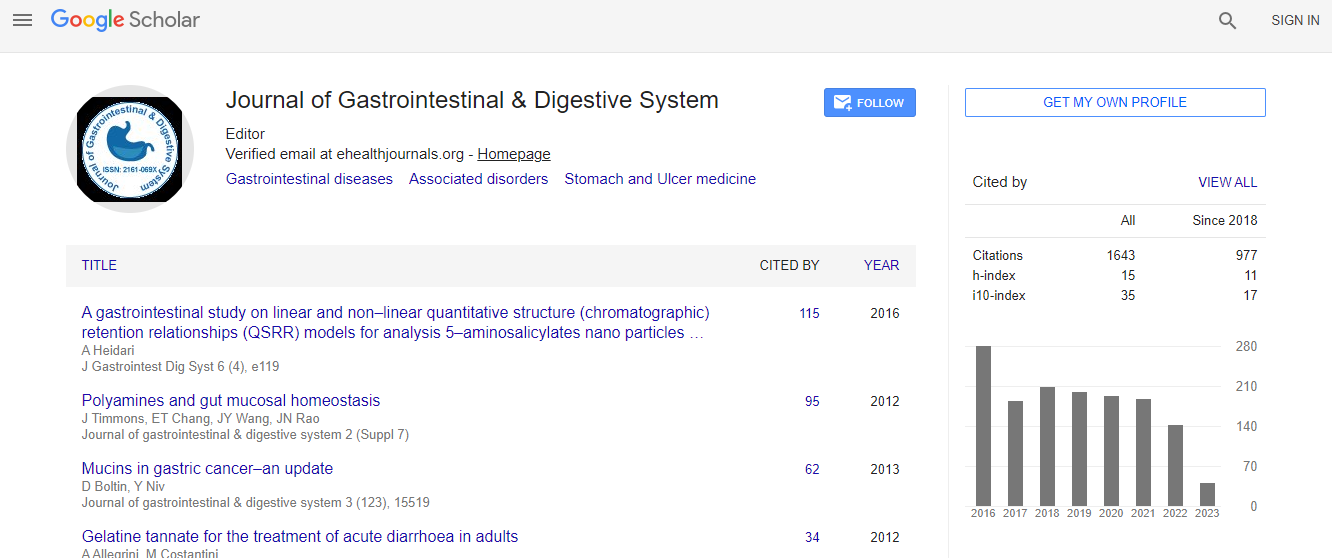
Citation: Mazid MA, Ye ZH, Geng XP, Liu FB, Zhao YJ, et al. (2016) Clinical Analysis of 65 Patients with Pancreatic Fistula Wound Infection after Pancreatoduodenectomy (PD) with Duct-to-Mucosa Pancreaticojejunostomy: A Single-Center Report. J Gastrointest Dig Syst 6: 481. doi:10.4172/2161-069X.1000481
Copyright: © 2016 Mazid MA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Objective:The study sought to analyze Whipple procedure in 65 patients’ in-hospital evaluation of morbidity and mortality rate after pancreatoduodenectomy (PD) with adjusted duct-to mucosa pancreaticojejunostomy. Methods: A retrospective study of 65 consecutive patients that underwent (PD) at ‘The First Affiliated Hospital of Anhui Medical University teaching Hospital during the period of December 2008 to December 2015 was done. A two-layered duct-to-mucosa pancreaticojejunostomy over an internal transanastomotic stent was performed in all 65 patients. Results: The in-hospital morbidity and mortality rate in the study was 47.6% and 1.5%, respectively. One patient died as a consequence of mesenteric ischemia. Pancreatic fistula occurred in one patient (1.5%) and was treated conservatively with good results. The wound infection was the most common surgical complication (13/65; 20%) and occurred more often in patients who had a biliary stent inserted endoscopicallyprior to surgery (10/24; 41.7%), as compared to those without the stent (3/41; 7.3%; P<0.0001). Conclusions: The consequences of the present study recommend that a two-layered conduit to-mucosa pancreaticojejunostomy with inside trananastomotic stent is a sheltered anastomosis, connected with an okay of pancreatic fistula. The nearness of a biliary stent at the season of surgery speaks to a danger element for the improvement of postoperative injury contamination. In our information we have an aggregate number of 65 patients some of them we did endoscopy and some of them didn't. 24 patients were done endoscopy and in these cases 10 patients get wound contamination while 41 of our patients did not get endoscopy but rather 3 patients get wound disease. The summery of information is that the rate of wound contamination is high with patients is who get the endoscopy.

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi