Research Article
Childhood Health and Development in a Cohort of Infants Exposed Prenatally to Methadone or Buprenorphine
Olivia Humbarger1, Daniel Galanto2, Kelley Saia3, Sarah M Bagley4, Elisha M Wachman5* and Susan B Brogly61Boston University School of Medicine, Boston, USA
2Department of Epidemiology, Boston University School of Public Health, Boston, USA
3Department of Obstetrics and Gynaecology, Boston Medical Centre, Boston, USA
4Section of General Internal Medicine, Department of Medicine, Boston University School of Medicine, Boston, USA
5Division of Neonatology, Department of Paediatrics, Boston Medical Centre, Boston, USA
6Departments of Medicine and of Surgery, Queen’s University, Kingston, ON, Canada
- Corresponding Author:
- Elisha Wachman
Division of Neonatology
Department of Paediatrics
Boston Medical Centre, Boston
Tel: 617-414-3690
Fax: 617-414-7297
E-mail: Elisha.Wachman@bmc.org
Received date: date: Nov 26, 2015; Accepted date: date: Jan 22, 2016; Published date: date: Jan 29, 2016
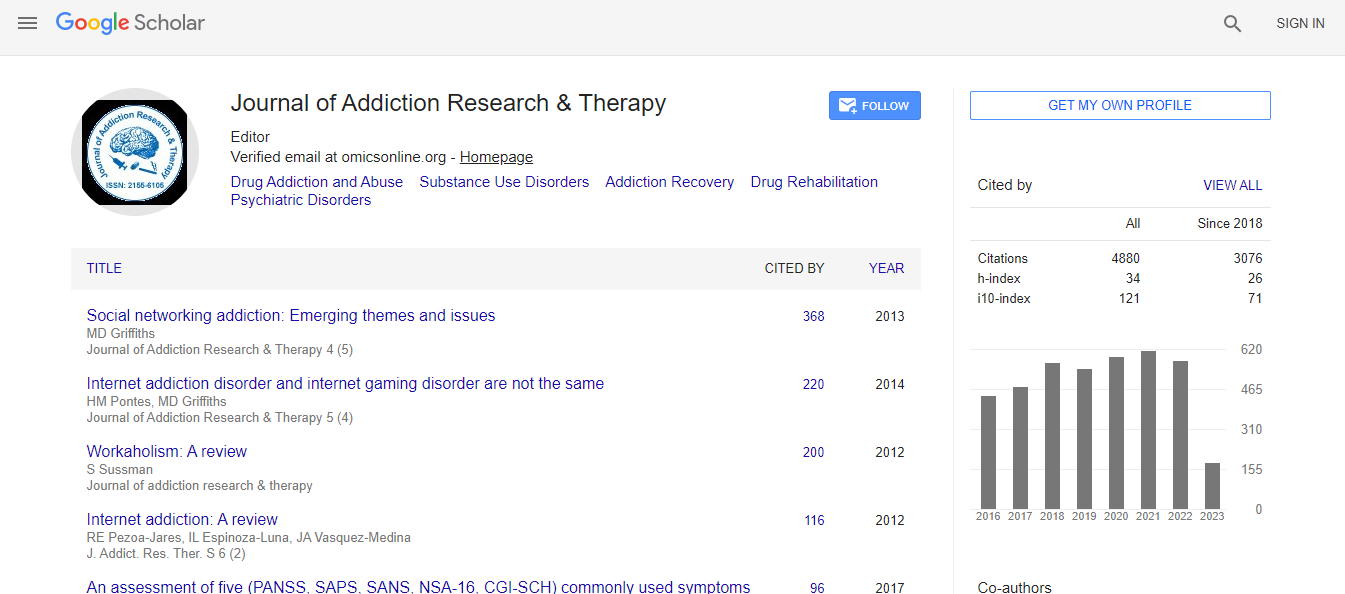
Citation: Humbarger O, Galanto D, Saia K, Bagley SM, Wachman EM, et al. (2016) Childhood Health and Development in a Cohort of Infants Exposed Prenatally to Methadone or Buprenorphine . J Addict Res Ther 7:263. doi:10.4172/2155-6105.1000263
Copyright: © 2016 Humbarger O, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Neonatal Abstinence Syndrome (NAS) due to in-utero opioid exposure is a growing problem with largely unknown long-term childhood outcomes. The objective of this study was to compare long-term outcomes of infants exposed to methadone versus buprenorphine in-utero.
Method: This retrospective cohort study included all pregnant women on buprenorphine or methadone and their infants born between 2006-2010 at our institution. Inpatient data was merged with outpatient data from 2006-2014 for those infants who continued to receive their paediatric care at our institution. We estimated unadjusted risk ratios (RR) of the following outcomes in buprenorphine versus methadone exposed infants: 1) routine healthcare visits, 2) growth and feeding disorders, 3) developmental delay, 4) visual problems, 5) hearing problems, 6) behavioural/attentional problems.
Results: Of 338 infants, 73.1% (N=247) continued to be followed at our hospital. The mean length of follow-up was 25.7 months (95% CI 22.9, 28.9). Infants in the buprenorphine group were less likely to be seen for hepatitis C exposure (19.6 vs. 9.2%, RR=0.60, 95% CI 0.40, 0.91) and more likely to have had a routine weight check (RR=2.14, 95% CI 1.05, 4.34). There were no differences in the incidence of developmental delay, ophthalmologic abnormalities, hearing deficits, or behavioural diagnoses between the groups. Results are limited by small sample size and lack of adjustment for confounders.
Conclusion: No significant differences in paediatric outcomes at 2 years of age after in-utero methadone or buprenorphine exposure were found, but the evidence is affected by study limitations. Further studies in a large patient population are warranted.

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi