Case Study: A Precision Medicine Approach to Multifactorial Dementia and Alzheimer’s Disease
*Corresponding Author: Dr. Jared C. Roach MD, PhD, Institute for Systems Biology, 401 Terry Ave N, Seattle WA 98109, USA, Tel: (+1) 206-324-5271, Email: jared.roach@isbscience.orgReceived Date: Aug 04, 2021 / Accepted Date: Aug 18, 2021 / Published Date: Aug 25, 2021
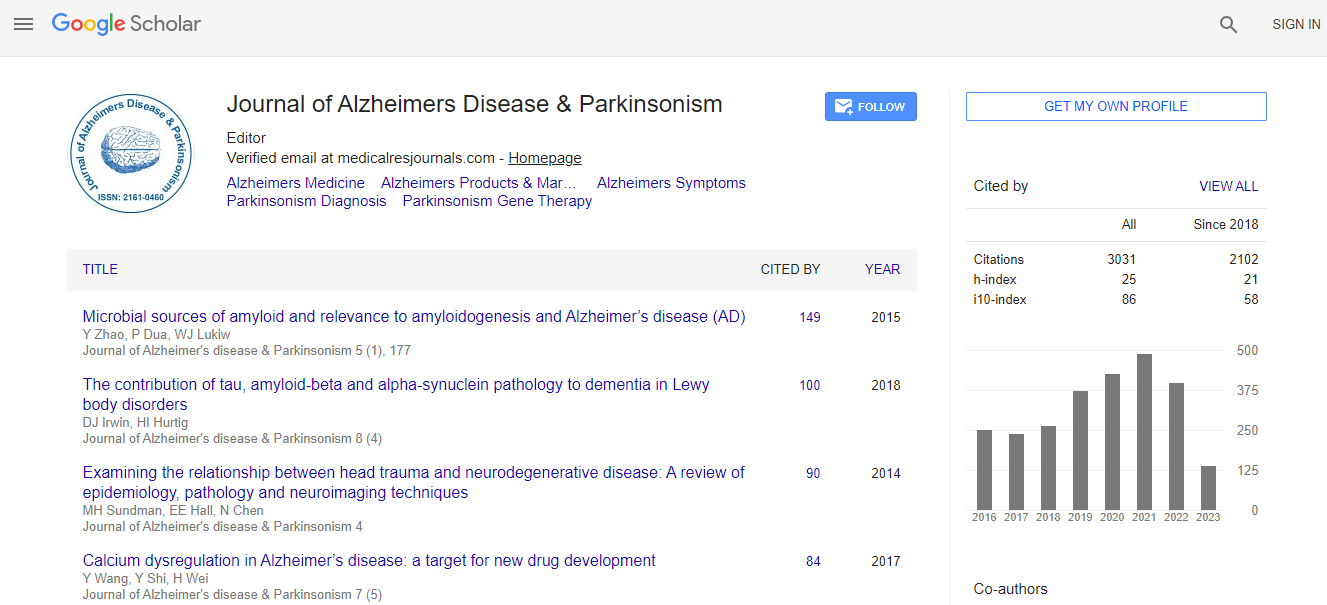
Citation: Ross MK, Raji C, Lokken KL, Bredesen DE, Roach JC, et al. (2021) Case Study: A Precision Medicine Approach to Multifactorial Dementia and Alzheimer’s Disease. J Alzheimers Dis Parkinsonism S5: 018.
Copyright: © 2021 Ross MK. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
We report a case of a patient with mixed dementia successfully treated with a personalized multimodal therapy. Monotherapeutics is inadequate for the treatment of Alzheimer’s disease (AD) and mixed dementia; therefore, we approach treatment through an adaptive personalized multimodal program. Many multimodal programs are pre-determined, and thus may not address the underlying contributors to cognitive decline in each particular individual. The combination of a targeted, personalized, precision medicine approach using a multimodal program promises advantages over monotherapies and untargeted multimodal therapies for multifactorial dementia. In this case study, we describe successful treatment for a patient diagnosed with AD, using a multimodal, programmatic, precision medicine intervention encompassing therapies targeting multiple dementia diastheses. We describe specific interventions used in this case that are derived from a comprehensive protocol for AD precision medicine. After treatment, our patient demonstrated improvements in quantitative neuropsychological testing, volumetric neuroimaging, PET scans, and serum chemistries, accompanied by symptomatic improvement over a 3.5-year period. This case outcome supports the need for rigorous trials of comprehensive, targeted combination therapies to stabilize, restore, and prevent cognitive decline in individuals with potentially many underlying causes of such decline and dementia. Our multimodal therapy included personalized treatments to address each potential perturbation to neuroplasticity. In particular, neuroinflammation and metabolic subsystems influence cognitive function and hippocampal volume. In this patient with a primary biliary cholangitis (PBC) multimorbidity component, we introduced a personalized diet that helped reduce liver inflammation. Together, all these components of multimodal therapy showed a sustained functional and cognitive benefit. Multimodal therapies may have systemwide benefits on all dementias, particularly in the context of multimorbidity. Furthermore, these therapies provide generalized health benefits, as many of the factors-such as inflammation-that impact cognitive functions also impact other systems.

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi