Research Article
Calpain-Mediated Hsp70.1 Cleavage in Monkey CA1 after Ischemia Induces Similar ‘Lysosomal Vesiculosis’ to Alzheimer Neurons
Tetsumori Yamashima1*, Arumugam Mathivanan1, Maryia Y. Dazortsava1, Shota Sakai2, Shota Kurimoto1, Hong Zhu1, Nozomi Funaki1, Hanbai Liang1, Françoise Hullin-Matsuda2, Toshihide Kobayashi2, Hiroyasu Akatsu3, Hitoshi Takahashi4 and Yoshio Minabe1
1 Departments of Restorative Neurosurgery and Psychiatry, Kanazawa University Graduate School of Medical Science, Kanazawa, Japan
2 Lipid Biology Laboratory, RIKEN (Institute of Physical and Chemical Research), Wako, Japan
3 Choju Medical and Neuropathological Institute, Fukushimura Hospital, Aichi, Toyohashi, Japan
4 Department of Pathology, Brain Research Institute, University of Niigata, Niigata, Japan
- Corresponding Author:
- Tetsumori Yamashima
Departments of Restorative Neurosurgery and Psychiatry
Kanazawa University Graduate School of Medical Science
Takara-machi 13-1, Kanazawa, 920-8641, Japan
Tel: +81762652381
Fax: +81762344264
E-mail: yamashima215@gmail.com
Received date: December 25, 2013; Accepted date: February 27, 2014; Published date: March 15, 2014
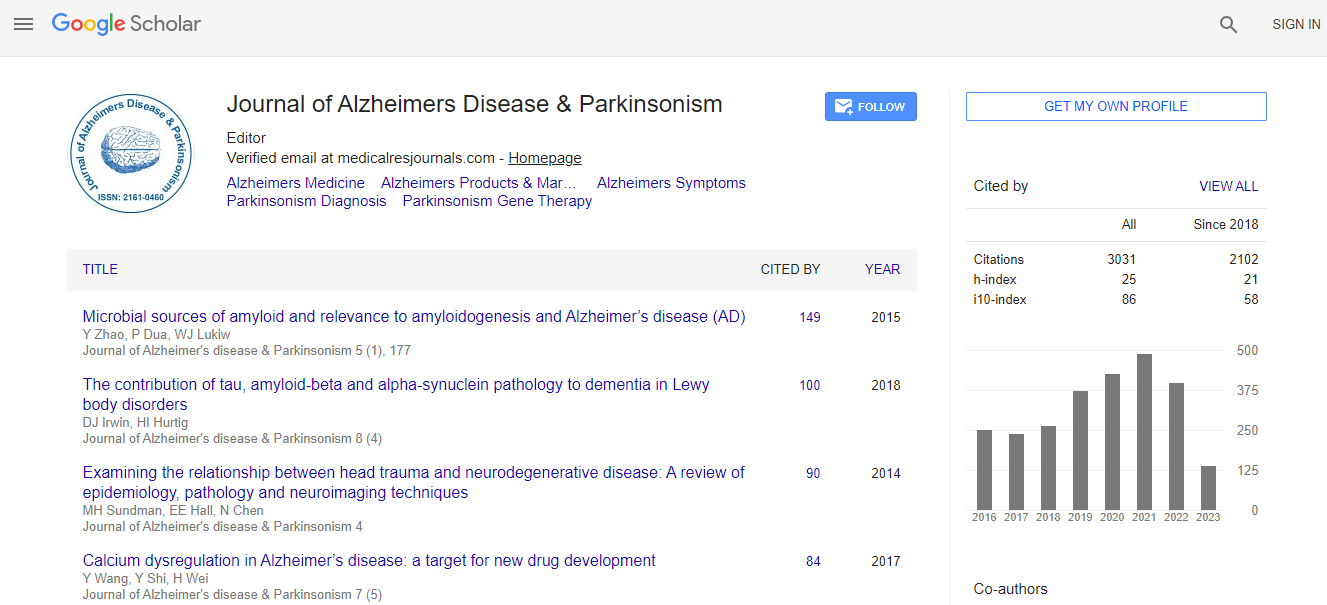
Citation: Yamashima T, Mathivanan A, Dazortsava MY, Sakai S, Kurimoto S, et al. (2014) Calpain-Mediated Hsp70.1 Cleavage in Monkey CA1 after Ischemia Induces Similar –Lysosomal Vesiculosis’ to Alzheimer Neurons. J Alzheimers Dis Parkinsonism 4:139.doi: 10.4172/2161-0460.1000139
Copyright: © 2014 Yamashima T, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
For the past decade evidence has gathered for the implication of lysosomes in the development of programmed cell death. Recent data advocate for dual roles of heat-shock protein 70.1 (Hsp70.1) not only as a molecular chaperone for damaged/aged proteins but also as a guardian of lysosomal integrity. Hsp70.1-mediated lysosomal stabilization is tightly regulated, but its disorder under extreme conditions results in lysosomal rupture to cause cell death. Comparing with the pathological hallmark ‘granulo-vacuolar degenerations’ in Alzheimer’s disease, the postischemic monkey neurons were carefully observed with microscope. Intriguingly, we found very similar change, and identified it as ‘lysosomal vesiculosis’ by electron microscopy. However, the exact molecular and structural impacts of the Hsp70.1 disorder upon the lysosomal membrane are hardly elucidated in the human brain because of the practical and ethical problems. Accordingly, using the monkey brain tissues after in-vivo and in-vitro oxidative stresses, we studied molecular modifications of Hsp70.1 and its counterpart bis(monoacylglycero) phosphate (BMP), because these molecules are closely related to the lysosomal membrane stability by regulating acid sphingomyelinase. It still remains unelucidated whether ischemia/reperfusion can alter composition or amount of BMP in the brain. Regardless of the brain regions studied, the normal monkey brain tissues showed calpain-mediated cleavage of Hsp70.1 after in-vitro oxidative stress. In the CA1 after in-vivo ischemia/reperfusion, we first found that docosahexaenoic and oleic acids in BMP showed a significant decrease on days 1 and 3, compared to non-ischemic controls. Since Hsp70.1- BMP binding is indispensable for activating acid sphingomyelinase and producing ceramide to stabilize lysosomal membrane, dysfunction of Hsp70.1 and BMP presumably causes storage of sphingomyelin and deficiency of ceramide at the lysosomal membrane, leading to its destabilization in the postischemic CA1 neurons. These data, combined together, suggest that lysosomal destabilization induced by calpain-mediated cleavage of carbonylated Hsp70.1 and the concomitant BMP breakdown causes ‘lysosomal vesiculosis’.

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi