Assessing Work Stressors in the Health Care Sector by Combining External Observation and Health Professionals&rsquo' Self-report in a Cross-sectional Study Design
*Corresponding Author: Peter KA, Division of Applied Research & Development in Nursing, Bern University of Applied Sciences, Bern, Switzerland, Tel: +41 31 848 45 22, Email: karin.peter@bfh.chReceived Date: Jul 20, 2019 / Accepted Date: Feb 25, 2020 / Published Date: Mar 03, 2020
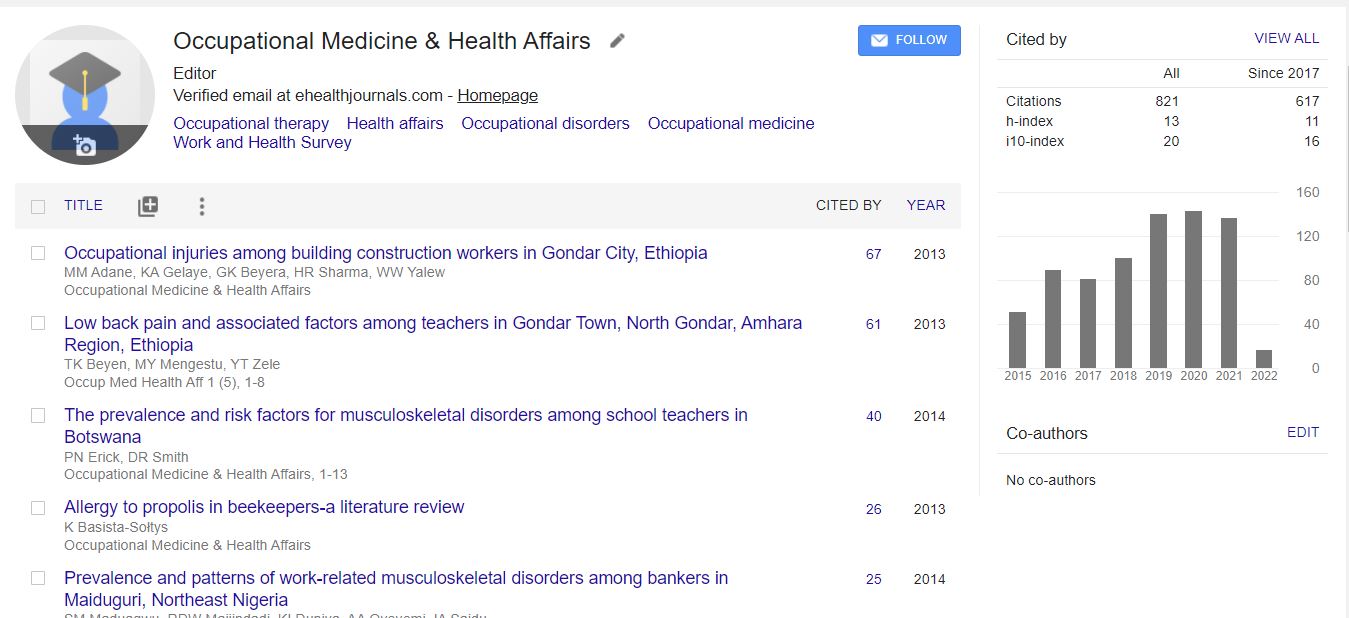
Citation: Peter K, Hahn S, Stadelmann E, Halfens RJG, Schols JMGA (2020) Assessing Work Stressors in the Health Care Sector by Combining External Observation and Health Professionals’ Self-report in a Crosssectional Study Design. Occup Med Health Aff 8: 303.
Copyright: © Peter K. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Objective: Health professionals are particularly affected by work stressors and various methods have already been used to assess them. Linking health professionals’ self-report and external observations can provide a more detailed assessment of stressors, since conclusions for interventions can be derived from their agreement. Since there is a lack of studies in the health sector linking both data sources, the aim of this study is to identify the convergence between health professionals’ self-reports and external observations. Methods: Data were collected in general hospitals, nursing homes, psychiatric institutions and home-care organizations in a cross-sectional study design. 110 health professionals were observed during one entire shift, by one of eight trained external observers. Health professionals and observer separately filled out a questionnaire on work stressors after the observation. For data analysis multiple regression models using bootstrap were calculated considering possible observer effects. Results: Convergent scores for 3 of 9 tested scales on ‘predictability’ of work, ‘social community’ and ‘social relations’ (p>0.05) at work, were identified. However, health professionals rated their ‘quantitative’ (p=0.001), ‘sensorial’ (p=0.001) and ‘physical demands’ (p=0.001) significantly higher than the external observers did. On the contrary, external observers perceived the ‘possibilities for development’ (p=0.007), ‘influence at work’ (p=0.032) and ‘social support at work’ (p=0.002) as lower than did the health professionals. Results also indicate a significant influence of different work settings (p<0.05) on the convergence of self-assessed and observed work stressors. Conclusion: This study results reveal that results on work stressors can be influenced by the chosen method for data collection, which should be considered when using one method only. Moreover, differences between the settings indicate that results on work stressors from one health-care setting cannot be easily transferred to another.

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi