Research Article
Antenatal Care Utilization and It’s Associated Factors in East Wollega Zone, Ethiopia
Tilaye Gudina Terfasa1, Mesganaw Fantahun Afework2 and Frew Tadesse Berhe3*1Federal Ministry of Health of Ethiopia, Maternal and Child Health Directorate, Ethiopia
2Department of Reproductive Health, School of Public Health, College of Health Sciences, Addis Ababa University, Ethiopia
3School of Public Health, College of Health Sciences and Medicine, Jigjiga University, Jigjiga, Ethiopia
- *Corresponding Author:
- Berhe FT
School of Public Health, College of Health Sciences and Medicine
Jigjiga University, Jigjiga, Ethiopia
Tel: 251913782429
E-mail: fretaabrish@gmail.com
Received date: April 07, 2016; Accepted date: April 17, 2017; Published date: April 24, 2017
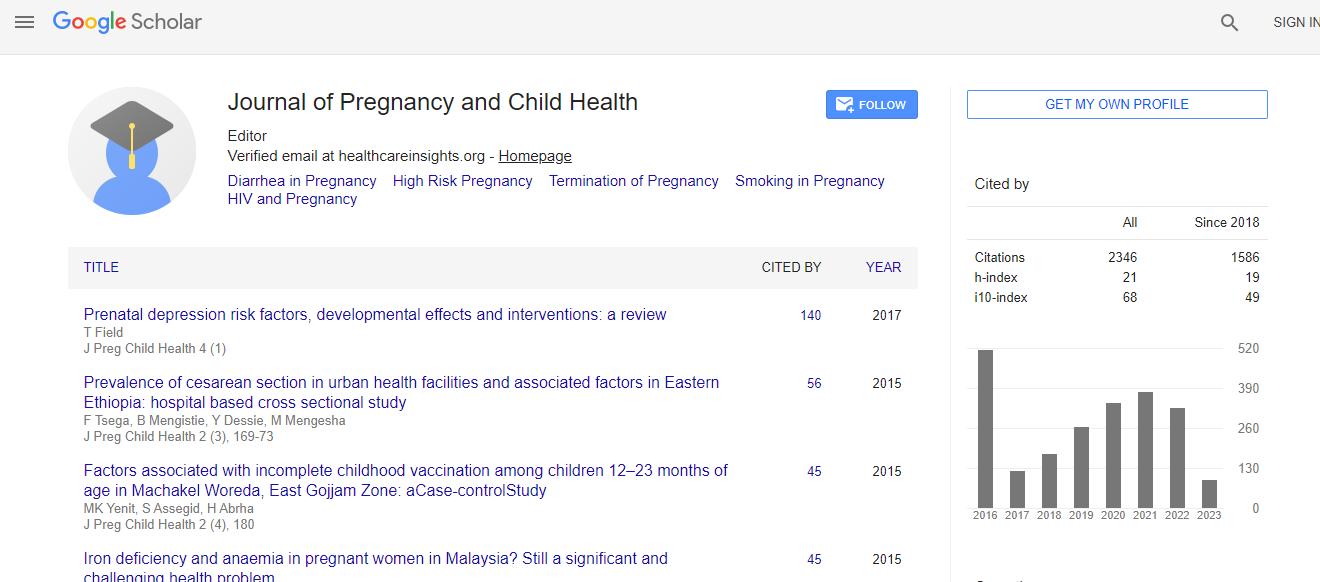
Citation: Terfasa TG, Afework MF, Berhe FT (2017) Antenatal Care Utilization and It’s Associated Factors in East Wollega Zone, Ethiopia. J Preg Child Health 4:316. doi:10.4172/2376-127X.1000316
Copyright: © 2017 Terfasa TG, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Antenatal care, is one of the most effective health interventions that can play a significant role in preventing maternal morbidity and mortality especially in under developed world. Information regarding its utilization is crucial to encourage mothers to get Antenatal care and institutional delivery service. Methods: A community-based cross-sectional study was carried out from October to November 2013 in East Wollega Zone of Oromia Regional State. Women aged 15-49 who gave birth in the 12 months prior to the beginning of the study in the selected kebeles/clusters were included in the study. Bivariate and multiple logistic regression models were used to examine the effect of each independent variable on ANC use. Results: Among the 770 women included in the study, 443 (57.5%) had at least one antenatal visit. Out of whom 58 (13.1%) had only one, 141 (31.8%) had two antenatal contacts 178 (40.2 %) had three visits, and only 66 (14.9%) had the recommended four or more antenatal visits. Among the potential determinants explored, having taken health education on maternal health [Adjusted OR (aOR)=5.5; 95% CI (3.2, 9.5)]; being above grade eight [aOR=2,8; 95% CI (1.4, 5.5)], grade one to four [aOR=2.3; 95% CI (1.5, 3.5)], grade five to eight [aOR =2.1; 95% CI (1.2, 3.6)]; being husband’s occupation “other than farming” [aOR=1.8; 95% CI (1.2, 2.9)]; and perceived walking time to the nearest health facility being <30 min [aOR=1.7; 95% CI (1.1, 2.5)] were the factors that encourage pregnant mothers to use ANC. Conclusion: This study has witnessed that there was low utilization of ANC services in the study area when compared to the recommended four visits during pregnancy. Hence, health education programs intended to enhance community use of ANC service should be strengthened.

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi