Research Article
Abdominal Stereotactic Body Radiotherapy: Local Control and Correlation to Biologically Equivalent Dose
| Simon Kirste1, Hans Trautsch1, Marc-Benjamin Messmer1, Rolf Wiehle1, Hans-Christian Rischke1, Felix Momm2, Anca-Ligia Grosu1 and Thomas B. Brunner1* | |
| 1Department of Radiation Oncology, University Hospitals Freiburg, Freiburg, Germany | |
| 2Department of Radiation Oncology, Ortenau Hospital Offenburg, Offenburg, Germany | |
| *Corresponding Author : | Thomas B Brunner Department of Radiation Oncology University Hospitals Freiburg, Freiburg, Germany Tel: +49-761-270- 94070 E-mail: thomas.brunner@uniklinik-freiburg.de |
| Received: February 11, 2016; Accepted: March 07, 2016; Published: March 10, 2016 | |
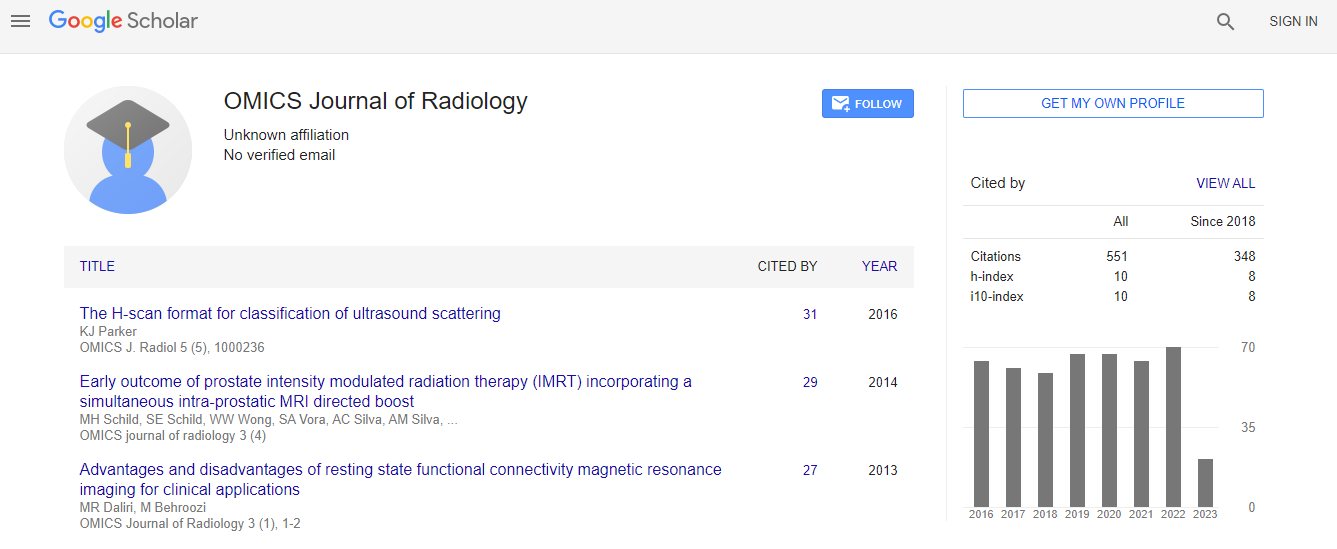
| Citation: Kirste S, Trautsch H, Messmer MB, Wiehle R,Rischke HC, et al. (2016) Abdominal Stereotactic Body Radiotherapy: Local Control and Correlation to Biologically Equivalent Dose. OMICS J Radiol 5:216. doi:10.4172/2167-7964.1000216 | |
| Copyright: © 2016 Brunner TB, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. | |
Abstract
Aim: We conducted a retrospective study to report on the outcome and toxicity of stereotactic body radiotherapy (SBRT) and to analyze the correlation of local control (LC) and biological equivalent dose (BED) of patients treated with SBRT for upper abdominal lesions.
Methods: Patients who completed stereotactic radiotherapy treatment between 05/2007 and 03/2012 were enrolled into the analysis. Different fractionation regimens depending on the dose to organs at risk (OAR) were given. The primary endpoint was LC determined on imaging studies. Toxicities were classified according to CTCAE v4. Physical dose was converted into BED (α / β = 10 Gy) and a tumor control probability model (TCP) was used for dose-response relationship. For outcome analyses the Kaplan-Meier method and log rank tests were used.
Results: Forty-two patients were treated with SBRT. Thirty-three patients with 39 lesions were evaluable for further analysis with a median follow-up of 15.2 months. Lesions were located in liver (n = 28), hepatic hilum (n = 8), nodal (n = 2), adrenal (n = 2) and pancreatic head (n = 1). Local failure was observed in 7 lesions at a mean time of 7.3 months (range, 1.5 - 17.9) resulting in a LC rate of 83% at one year and 63% at two years. No significant difference for intra- vs extrahepatic lesions was observed. Lesions treated with a BED ≥ 59.5 Gy had a better LC vs. lesions treated with a BED < 59.5 Gy (88% vs. 68%, p = 0.027). Median overall survival was 14.5 months (2 - 32.5). Observed toxicities were mild (grade 2 in 4 patients, grade 3 in 1 patient).
Conclusion: Upper abdominal SBRT is well tolerated and results in excellent local control if BED is ≥ 59.5 Gy. We therefore propose to aim for doses at or above this BED.

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi