Research Article
3D-CT Mammary Lymphography Can Help Selective Axillary Dissection of Breast Lymph Flow Differed from the Arm
| Koji Yamashita* and Kazuo Shimizu | |
| Department of Breast Surgery, Nippon Medical School, Japan | |
| Corresponding Author : | Koji Yamashita Department of Breast Surgery, Nippon Medical School 1-5, Sendagi-1, Bunkyo-ku, Tokyo, 113-8602, Japan Tel: +81-3-5814-6219 Fax: +81-3-5685-0985 E-mail: yamasita@nms.ac.jp |
| Received December 19, 2013; Accepted January 25, 2014; Published January 27, 2014 | |
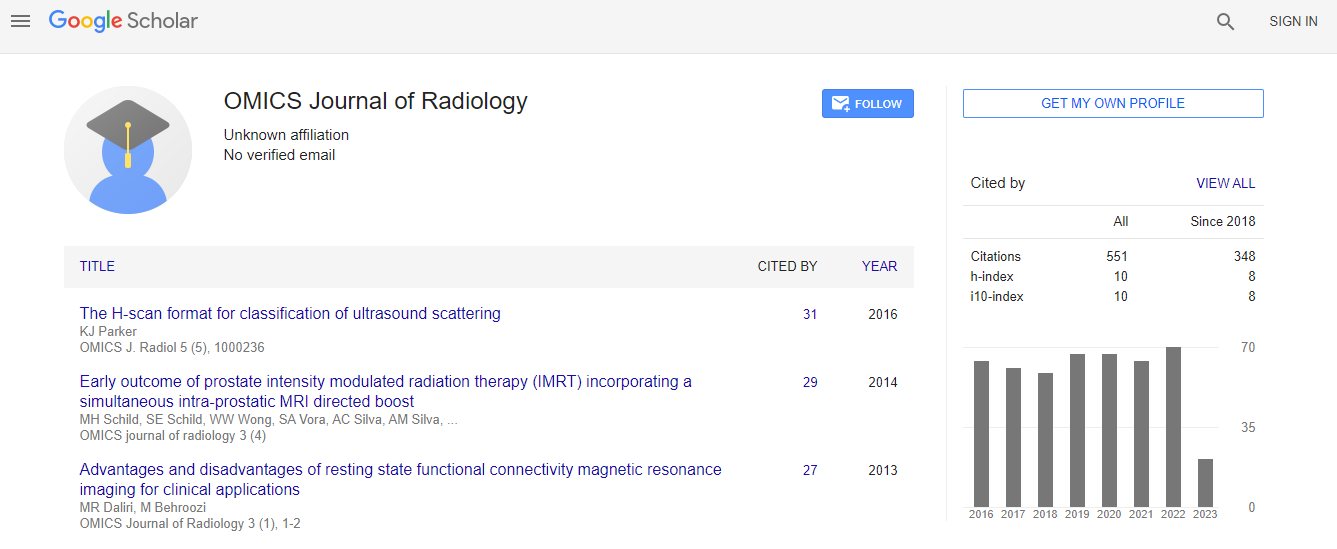
| Citation: Yamashita K, Shimizu K (2014) 3D-CT Mammary Lymphography Can Help Selective Axillary Dissection of Breast Lymph Flow Differed from the Arm. OMICS J Radiol 3:158. doi:10.4172/2167-7964.1000158 | |
| Copyright: © 2014 Yamashita K, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. | |
Abstract
Background: Axillary Nodes (AN) dissection causes many complications such as lymphedema. Three Dimensional Computed Tomographic (3D-CT) Lymphography (LG) can show the precise individual lymphatic flow from the breast tumor to Sentinel Node (SN), and through AN to venous angle, which means breast lymphatic channel. We applied 3DCT LG to distinguish them from the arm channel to avoid any arm complications.
Methods: 3D-CT LG used contrast medium injected subcutaneously above the tumor, near the areola and the inner upper arm. CT images were taken 1, 3 and 5 minutes after injection. SN biopsy and AN dissection were performed by dye-method using endoscopy.
Results: We performed SN biopsy with 3D-CT LG on 160 patients. 3D-CT LG clearly showed the precise lymphatic flow from the tumor to SN one minute after injection and five axillary node groups into venous angle 5 minutes after injection. Detection rate of SN, the second, the third, and the fifth group was 100%, 88%, 80%, and 30% respectively. The arm lymph flow was distinguished by the connecting ducts between the breast and the arm channel, observed 39% and 71% in the fourth and the fifth group. Five patients (3.1%) had the common SN from the breast and the arm channel, and suffered arm lymphedema only after SN biopsy. We dissected AN from the breast by endoscopic surgery on the SN-positive patients.
Conclusions: 3D-CT LG can helps us easily to distinguish between the breast and the arm channel by finding the connecting ducts.

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi