Research Article Open Access
Pathways of Breast Cancer Screening Among Chinese American Women
Grace X Ma1*, Carolyn Fang2, Min Qi Wang3, Steven E Shive4 and Xiang S Ma5
1Professor of Public Health, Department of Public Health, Director of Center for Asian Health, College of Health Professions, Temple University, Philadelphia, USA
2Fox Chase Cancer Center, Cancer Prevention and Control Program, 333 Cottman Ave, Philadelphia, PA 19111 USA
3Professor, Department of Public and Community Health, University of Maryland, College Park, Maryland, USA
4Research Associate, Center for Asian Health, Temple University, USA, and Department of Health, East Stroudsburg University, East Stroudsburg, PA
5Center for Asian Health, College of Health Professions and School of Medicine, Temple University, Philadelphia, USA
- *Corresponding Author:
- Grace X Ma, PhD
Professor of Public Health, Department of Public Health
Director of Center for Asian Health, College of Health Professions
Temple University, 1301 Cecil B. Moore Ave.
913 Ritter Annex, Philadelphia, PA, 19122-0843, USA
Tel: 215-204-5108, 215-787-5434
Fax: 215-787-5436
E-mail: grace.ma@temple.edu
Received date April 02, 2013; Accepted date: April 16, 2013; Published date: April 19, 2013
Citation: Ma GX, Fang C, Wang MQ, Shive SE, Ma XS (2013) Pathways of Breast Cancer Screening Among Chinese American Women. J Community Med Health Educ 3:209. doi: 10.4172/2161-0711.1000209.
Copyright: © 2013 Ma GX, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Community Medicine & Health Education
Abstract
Objective: The purpose of this community-based study was to develop a structural equation model for factors contributing to breast cancer screening among Chinese American women.
Methods: A cross-sectional design included a sample of 440 Chinese American women aged 40 years and older. The initial step involved use of confirmatory factor analysis, which included the following variables: access/satisfaction with health care, enabling, predisposing, and cultural and health belief factors. Structural equation model analyses were conducted to evaluate factors related to breast cancer screening in Chinese American women.
Results: Initial univariate analyses indicated that women without health insurance were significantly more likely to report being never-screened compared to women with health insurance. Structural equation modeling techniques were used to evaluate the utility of the Socio cultural Health Behavior model in understanding breast cancer screening among Chinese American women. Results indicated that enabling and predisposing factors were significantly and positively related to breast cancer screening. Cultural factors were significantly associated with enabling factors and satisfaction with healthcare. Overall, the proposed model explained 34% of the variance in breast cancer screening
among Chinese American women.
Conclusions: The model highlights the significance of enabling and predisposing factors in understanding breast cancer screening behaviors among Chinese American women. In addition, cultural factors were associated with enabling factors, reinforcing the importance of providing translation assistance to Chinese women with poor English fluency and increasing awareness of the critical role of breast cancer screening. Partnering with community organizations may help to facilitate and enhance the screening rates.
Keywords
Mammograms; Breast cancer screening; Chinese women
Introduction
Cancer is the number one cause of death among Asian American women [1-3]. Asian American women also have the lowest cancer screening rates of all ethnic groups in the United States [4,5]. Asian Americans overall report: a breast cancer incidence rate of 88.6/100,000 and a mortality rate of 12.6/100,000 women [6]. Mammogram screening rates are lower for Asian Americans at 57.0%, compared with Whites 72.1% [7,8]. There are, however, Asian subgroup differences in incidence of cancer and in cancer screening rates [9]. For Chinese American women in particular, breast cancer is the most frequently diagnosed cancer [3,10]. Chinese American women who have lived in the United States for a longer duration are at higher risk for breast cancer than are new immigrants [11].
Despite recommendations from the American Cancer Society, the Michigan Cancer Consortium, the American Medical Association, and other professional organizations that all women aged 40 years and older have an annual mammogram, Chinese American women have relatively low rates of breast cancer screening. Previous studies have indicated that mammogram rates among Chinese American women range from 71.1% to 74.0% [12,13]. Lee-Lin et al. reported that while 86% of Chinese American women reported ever having had a mammograms, only 48.5% had had one in the past year [14]. Rates of breast self-examination and clinical breast exams are similarly low among Chinese American women at 53.2% and 53.6%, respectively [12].
Various factors have been associated with poor adherence to breast cancer screening recommendations among Chinese American women, including education level, language difficulties, cultural and acculturation factors, economic barriers, and health insurance coverage, satisfaction with health care, and fear of having cancer [8,15,16]. Factors that enhance a woman’s likelihood of getting a mammogram include having health insurance and having seen a physician in the past year [13,17,18].
Many previous studies have examined the relationship between various independent variables and screening outcome using co relational analyses. However, socio cultural and ecological models stress the interrelationships among individual, interpersonal, and environmental factors. Specifically, these models examine the relationship between an individual’s behavior and the manner in which a given behavior interacts with the immediate environment and how aspects of the contextual settings influence the individual and his or her immediate environment. Furthermore, distal factors such as family influences cannot be differentiated at the same time in analysis models such as logistic regression or linear regression. As a result, the interactions and multiple levels of influence of individual, interpersonal, and environmental factors underlying the behavioral ecological model make these interrelations difficult to study.
Structural Equation Modeling has been used to study a variety of diverse outcomes, such as substance use among minority youth, factors for academic performance, HIV risk reduction intervention for injection drug users in treatment, marital conflict and children’s adjustment, stress among policy officers, and racial/ethnic disparities in knowledge of HIV of testing and treatment [19-22]. Few studies have used Structural Equation Modeling to examine cancer-related behaviors or outcomes in domains such as cancer survivorship and physician-patient communication [23,24]. This is especially true in relation to breast cancer screening behaviors among Chinese American women. Structural Equation Modeling offers some advantages in the examination of factors in the cultural and ecological approaches [25]. The structure of relationships among set factors can be tested [26], there is increased statistical control over random measurement error and measurement biases [25], and examination of interrelated constructs can occur without the disadvantages of a multivariate analysis of covariance approach [27]. Because screening behavior is influenced by multiple factors, there is a need to identify and characterize the interrelationships among these factors. Too often, the role of cultural factors is seldom included in analyses of health behavior outcomes.
Socio cultural Health Behavior Model is used to explain health behavior [28]. In addition to common theoretical components, this model includes cultural factors as a primary component. The model incorporates the interdependence of predisposing, enabling, need, family/social support, environmental health system, and cultural factors which contribute to a particular health behavior or outcome. A number of variables can be included under cultural factors, including notions of fatalism, birth in the United States, years lived in the United States, level of English fluency, use of native language at home, native food eaten and at what frequency, use of media sources in native language, and attendance of native social events.
The analysis of this community-based study was guided by the Sociocultural Health Behavior Model [28], using a structural equation analysis to determine the direction and magnitude of the interdependence of the proposed components of the model in relation to the health behavior of breast cancer screening among Chinese American women.
Methods
Sample
Participants in this study were recruited as part of a larger study that included a sample of Chinese, Korean, Vietnamese, and Cambodian Asian Americans. In the larger study, 111 Asian American community organizations in the greater Philadelphia area, New Jersey, and New York City were identified by the Asian Community Cancer Coalition and staff of ATECAR-Asian Community Cancer Network. These organizations are located in geographic areas that helped to maximize the coverage of Asian Americans across ethnic groups, ages, and socioeconomic status. Asian American community organizations (N=52) were randomly selected as clusters from the list of 111 organizations. The selected community organizations were stratified based on the four racial/ethnic or language groups. A proportional allocation procedure of assigning the sample size proportionally to the subgroups’ size was used [29]. In the larger parent study, 2,098 participants agreed to participate; of these, 2,011 completed the study for a response rate of 95.9%. The overall sample (N=2,011) was comprised of: 45.9% Chinese (N=923); 19.1% Korean (N=384); 18.1% Vietnamese (N=364); and 16.9% Cambodian (N=340) participants. For the purpose of the present study, Chinese women aged 40 years and older were selected, resulting in a final sample of 440 Chinese American women.
Design and data collection procedures
A cross-sectional research design was used for this study because of the common advantages provided by this method, such as collecting information from numerous, diversified participants in a short time. All data were collected at the facilities of Asian American community organizations. Data collection and survey administration training was provided to all survey administrators as well as to onsite bilingual translators. The survey was administrated in person. When necessary, language assistance was provided during survey administration. Participants had the option of responding to the questionnaire in English or in their native language (Chinese, Korean, or Vietnamese). Translators were provided when needed for individuals or group translations. The average time for completion of the questionnaire was 25 minutes.
Measurements
A 95-item questionnaire, developed by the Principal Investigator and research team, was back-translated, and pilot-tested for reliability, validity, and cultural appropriateness with community partners.
The full questionnaire included the following groups of variables: (1) predisposing factors (age, gender, marital status, education level, ethnic background, and employment status); (2) cultural factors (fatalism, importance of screening, birth in the United States, years lived in the United States, ability to speak English, use of native language at home, preparation of native food at home, and use of media sources in native language); (3) health beliefs (feeling well so there were no perceived health problems, susceptibility, fear of getting a bad test result, embarrassment/shame of undergoing screening, and fear of having a health problem); (4) enabling factors (annual household income, having health insurance, coverage of screening by insurance provider, having a primary care physician, and barriers to screening such as language, transportation, lack of knowledge about disease or location of services, having routine health exams, and self-efficacy); (5) access factors/satisfaction with health care (having a physician who speaks the native language, having insurance that covers the cost of screening, receiving physician advice to get screened, needing assistance in transportation, having access to medical services when needed, needing assistance in making arrangements for appointments, length of time waiting to see physician, ability to contact physician after hours or weekends, convenience of location of physician, and quality of care by physician); (6) family/social support (family support of screening, acting on physician’s advice, and family or friends having breast cancer).
In the initial step, a confirmatory factor analysis of the full questionnaire was conducted and led to the final list of survey questionnaire items that were then used in the SEM analysis. The alpha reliability coefficients of the final items are presented in table 1 and are described below:
Access/satisfaction with health care: Seven items assessed a respondent’s perceptions of their health care and doctors’ services. The response categories were on a 5-choice scale: “poor,” “fair,” “good,” “very good,” and “excellent”.
Enabling factor
The enabling factor was measured using three questions: Do you currently have health insurance? Do you have a primary health care provider to go to when you are sick? How many times did you visit your current primary physician in the last 12 months? The response categories were a binary choice (no/yes) for the first two questions. The third question’s potential responses were on an ordinal scale with four choices: “never,” “1-2 times,” “3-4 times,” and “5 or more times.”
Predisposing factor
The predisposing factor measured the education level of the participants, including their highest grade of school completed and their years of education completed.
Cultural factor
The cultural factor included participants’ English proficiency and their level of information seeking (Internet use). The response categories were “not at all” to “very well” for English speaking and a binary choice (no/yes) for Internet use.
Health belief factor
The cancer fear factor reflects the fear of knowing a bad cancer test result and whether the participants felt embarrassment about getting the cancer screening test. The response categories were a binary choice (no/yes).
Statistical Analysis
Model description
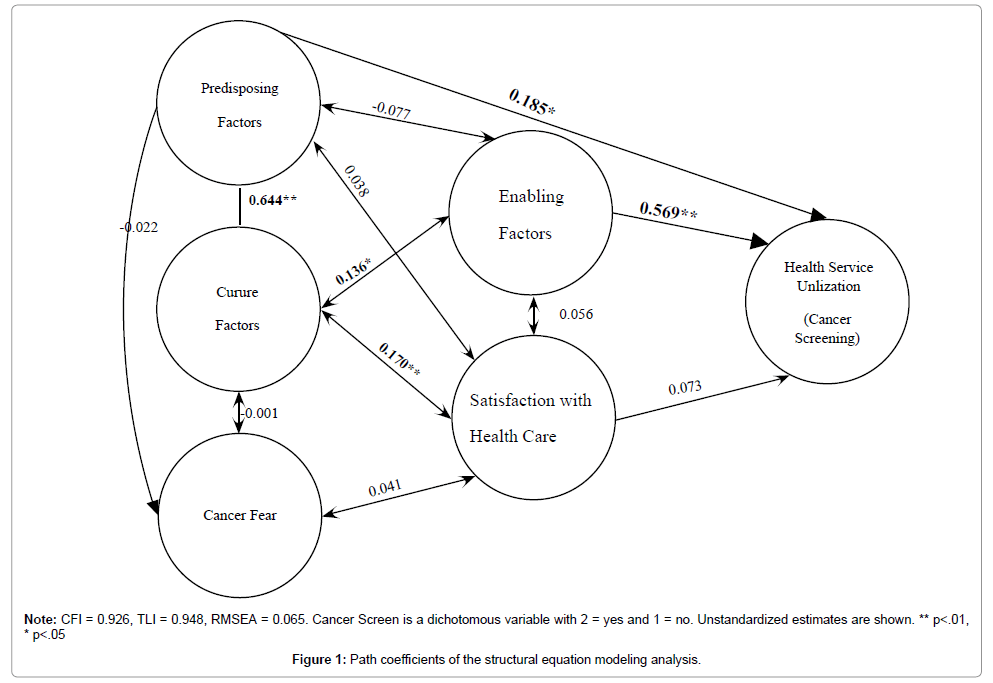
Structural equation model analyses were conducted using Mplus software. The models were covariance structural models with multiple indicators for all latent constructs. The analysis employed a twostep procedure using maximum likelihood estimation. The first step was confirmatory factor analysis to test the measurement model. A measurement model describes the nature of the relationship between a number of latent variables and the observed variables corresponding to each of the constructs. The second step tested the structural model, depicted in figure 1 in the Results section. This step represents the theoretically-based model in which the relationships among exogenous variables (those variables with both emanating paths and receiving paths) and endogenous variables (those variables with mostly receiving paths) can be seen. The dependent factor is a binary variable: never screened vs. screened. Using ordinal and dichotomous indicators is a very common practice in SEM literature. This practice is based on the assumption that the underlying construct represented by the dichotomous variables are continuous. A tetra choric correlation was created instead of Pearson correlations for the SEM analysis [30].
Model fit tests. Multiple indices were used to test the model fit including: the comparative fit index (CFI), where a value of 0.90 or higher is considered acceptable [26]; Tucker-Lewis Index (TLI), where a value of 0.90 or higher is considered acceptable [26]; and the root mean square error of approximation (RMSEA), with a value below 0.08 indicating good model fit.
Results
Sample characteristics
Demographic characteristics of study participants are presented by screening status in table 1. Only health insurance status significantly differed across the three groups, χ2 (2)=42.13, p<0.01. The percentage of women without health insurance reporting never-screened was three times greater than that of women with health insurance (43.2% vs. 14.2%). The groups did not differ on any of the other demographic variables. More women with annual household incomes below $10,000 (25.8%) reported never-screened than women with annual household incomes of more than $30,000 (11.6%). A greater percentage (24.2%) of those with below high school education reported never-screened compared with those with high school or more education (18.7%). A greater percentage (22.6%) of those unemployed reported neverscreened compared with those employed (18.6%). Married and unmarried were not related to screening with 23.8% of unmarried women reporting never-screened vs. 19.5% of married women reporting never screened.
| N=440 | Never Screened | Non Compliance | Compliance |
|---|---|---|---|
| Age Category | |||
| 40-64 | 20.6 | 21.8 | 57.5 |
| 65+ | 19.0 | 23.8 | 57.1 |
| Current Marital Status | |||
| Unmarried | 23.8 | 18.8 | 57.5 |
| Married | 19.5 | 23.1 | 57.4 |
| Highest Degree | |||
| <High School | 24.2 | 19.2 | 56.7 |
| >High School | 18.7 | 24.3 | 56.9 |
| Employment Status | |||
| Employed | 18.6 | 22.1 | 59.3 |
| Unemployed | 22.6 | 22.6 | 54.8 |
| Annual Income | |||
| <$10,000 | 25.8 | 19.2 | 55.0 |
| $10,000-$30,000 | 17.1 | 21.9 | 61.0 |
| >$30,000 | 11.6 | 27.5 | 60.9 |
| Current Health Insurance** | |||
| No | 43.2 | 27.2 | 29.6 |
| Yes | 14.2 | 21.2 | 64.5 |
Table 1: Demographics and mammogram screening status for chinese women.
Model fit index
The CFI for the SEM model was 0.926, which meets the acceptable model fit criterion. The TLI yielded a value of 0.948. The RMSEA compares the observed variances and co variances with those resulting from the model’s parameter estimates and is not sensitive to sample size. The RMSEA of 0.065 indicated an acceptable fit of the measurement model.
Measurement model
The factor loadings for the indicator variables associated with the constructs are presented in table 2. The factor loadings are equivalent to standardized regression weights for predicting observed variables from latent constructs. The t-scores obtained for the coefficients in table 2 were all significant except for one variable (embarrassment/ shame). The magnitude of the factor loadings and their significance provided evidence to support the convergent validity of the indicators. Overall, the model fit indices and the factor loadings supported the reliability and validity of the constructs for their indicator variables. It was concluded that the theoretical constructs hypothesized to exist at the level of latent factors were assessed with an acceptable degree of precision and that the observed variables were adequate indicators of these factors.
| Construct & indictors | Factor Loading |
|---|---|
| Access Factors/Satisfaction with Health Care | |
| Arrangements for making appointments for medical care | 1.000 |
| Length of time waiting to see doctor at the office | 0.981 |
| Length of time between making an appointment for care and visit | 0.971 |
| Rating of care for medical group | 0.873 |
| Convenience of location of the doctor's office | 0.955 |
| Access to medical care whenever needed | 0.955 |
| Quality of care from your physician | 0.812 |
| Enabling factor | |
| Currently have health insurance | 1.00 |
| Have a primary health care provider | 0.945 |
| Number of visits to current primary physician in the last 12 months | 0.565 |
| Predisposing factor | |
| Highest grade of school completed | 1.00 |
| Years of education completed | 3.966 |
| Cultural factor | |
| Internet as source of information | 1.00 |
| Perception of English fluency | 0.806 |
| Use of native Asian language at home | 0.268 |
| Health Belief | |
| Fear of a getting a bad test result | 1.00 |
| Embarrassment/shame | 1.937 |
Table 2: Parameter Estimates for the Measurement Model.
Structural model
The hypothesized model and the standardized maximum likelihood estimates for the parameters of the model are presented in figure 1. For all figures presented in this section, the constructs were coded in the same direction: a positive path coefficient indicates that it is more likely to be associated with cancer screening.
The path coefficients indicate the direction and magnitude of the associations. To summarize the findings of the structural equation findings, the following equation can be derived:
Breast Cancer Screening=0.569(enabling factor) + 0.185(predisposing factor)
The enabling factor was positively and significantly associated with screening (coefficient=0.569, t=7.325, p<0.001). Predisposing factors were also positively related to screening (coefficient=0.185, t=2.424; p<0.05). These two significant path coefficients indicate that: (1) women with health insurance, a primary health care provider, and frequent primary physician visits were more likely to have had breast cancer screening; and (2) more educated women were more likely to be screened for breast cancer. Cultural factors were not directly related to breast cancer screening. However, it was significantly associated with the enabling factor as well as satisfaction with health care. Though satisfaction with health care was positively related to cancer screening, this pathway was not found to be statistically significant (p>0.05). The R2 value provides explained variance among construct variables. Overall, 34% of the cancer screening was explained by the model.
Discussion
The present study evaluated the relationship of breast cancer screening with factors in the Socio cultural Health Behavior model among Chinese American women. This study adopted a structural equation model analysis to determine the structural relationship and multiple levels of influence of predisposing, enabling, cultural, health system access, and health belief factors underlying breast cancer screening among Chinese American women. The study found some significant pathways of the original model proposed and some additional factors.
Univariate analyses indicated that health insurance status was significantly related to breast cancer screening. Women with health insurance were significantly more likely to get screened and to be compliant with screening than were women who did not have health insurance. Studies consistently show that lack of health insurance coverage leads to reduced screening [8,10,16,31,32].
Structural equation modeling
Overall, our results offer support for a multilevel socio cultural approach to understanding the relationship between access/satisfaction with health care, predisposing, enabling and cultural factors, and health beliefs and breast cancer screening. Factor loadings which were significant for the enabling and predisposing factors showed a positive and significant relationship with screening for breast cancer. Chinese American women with health insurance, a primary care provider whom they see frequently, and a higher education level were more likely to be screened for breast cancer than were women in whom these factors were not present.
There has been some inconsistency in the literature regarding the role of education level and breast cancer screening. The role of education has not been examined systematically in previously published studies. Some studies show support for the direct and indirect influences of education level on cancer screening, while analyses in other studies did not show a significant correlation between education and socioeconomic status in cancer screening [15,33-35]. A possible explanation is that the constructs of education and income are multidimensional. Researchers may need to explore the various dimensions of education and income level/socioeconomic status separately to assess whether these dimensions are significantly related to breast cancer screening. There may be more dimensions to education level or income than having more education than high school or annual income that may be influential on a Chinese American woman’s decision to get a mammogram. Further, low income may not be as important to breast cancer screening because some Chinese American women who have Medicaid/Medicare may be likely to obtain breast cancer screening, if they chose to obtain one.
The path analysis findings also lend support for components of the Socio cultural Model and indicated that there was a positive and significant relationship between breast cancer screening and the predisposing and enabling factors, between cultural factors and predisposing, enabling, and access/satisfaction with health care factors, and between enabling factors and access/satisfaction with health care [28]. In general, if Chinese American women were able to access and were satisfied with health care, they were more likely to get a mammogram. There were a number of factors that loaded heavily under access/satisfaction with health care. These factors included ability to make an appointment, not having to wait long, the providers were in a convenient location, and higher provider ratings by the women. The cultural factor was significantly related to the predisposing and enabling factors and satisfaction with health care. Those Chinese American women who perceived they were fluent in English and who used the Internet as a source of information were more likely to get a mammogram. A health belief, that of fearing that one will get a bad test result, also was determined to be a factor in whether women went for a mammogram. The model accounted for 34% of the variance in breast cancer screening.
The model highlights the significance that socio cultural factors play in relation to breast cancer screening. Consistent with previous studies, being more acculturated in general and the ability to speak English in particular, is associated with higher breast cancer screening rates than those who were less fluent in English [16,34,36]. These findings reinforce the necessity to assist Chinese American women who have poor English language skills with translation and awareness of the importance of breast cancer screening.
In conclusion, this study analyzed and illustrated a model of the pathways among constructs leading to breast cancer screening among Chinese American women. By using structural equation modeling, the most likely linkages among constructs and the mediating factors can be examined. This model investigated how cultural, predisposing, enabling, access/satisfaction with health care, and health belief factors with breast cancer screening. To our knowledge, our present study is one of the first studies to have performed a path analysis to assess factors that may be associated with breast cancer screening among Chinese American women.
Limitations
There are several limitations to this study. First, since the study was cross-sectional, the causality of relationships among the constructs cannot be determined. Second, these findings are based on self-report questionnaires and as a result may include participant response bias. Third, since the sample was drawn from Chinese American women who participate in community organizations, the findings may not be generalizable to all Chinese American women.
Prevention efforts must focus on groups who have the lowest rates of screening for breast cancer. To be successful, breast cancer screening programs must include activities that take into account the multiple factors that interact which lead to lower rates of screening among Chinese American women compared to other groups. Sensitivity to ethnic and cultural factors, such as the use of the English language and other family or community contexts and dynamics, should be present throughout all secondary prevention activities, especially with the provision of translation services and education materials in one’s native language, to enhance interventions which target improved breast cancer screening rates among Chinese American women.
Furthermore, the significant relationship that cultural factors had to more proximal constructs suggests that the use of culturally appropriate materials be explored. The use of community organizations, which served as the basis for the study, can play a role in assisting Chinese American women in identifying, planning, and adopting effective evidence-based screening programs. Such community organizations may work in collaboration with representatives from local government, the local health department, and other related partners to be more successful than the work of a single agency in implementing prevention programs.
Acknowledgements
The authors wish to thank Asian Community Health Coalition partners, volunteers, community coordinators, and research team at the Center for Asian Health, Temple University, who facilitated and supported the completion of the study. This research was supported by National Institutes of Health, National Cancer Institute’s Community Networks Program (CNP), grant U01 CA114582 ATECAR-Asian Community Cancer Network (Grace X. Ma, Ph.D., Principal Investigator) and U54 CA153513 Asian Community Cancer Health Disparities Center (PI: Dr. Grace Ma).
Author Disclosure Statement: No competing financial interests exist.
References
- Chen MS Jr, Koh HK (1997) The Need for Cancer Prevention and Control among Asian Americans and Pacific Islanders. Asian Am Pac Isl J Health 5: 3-6.
- Leading causes of death by race/ethnicity, All females- United States (2009). Department of Health and Human Services. Centers for Disease Control and Prevention.
- Wu TY, West B, Chen YW, Hergert C (2006) Health beliefs and practices related to breast cancer screening in Filipino, Chinese and Asian-Indian women. Cancer Detect Prev 30: 58-66.
- American Cancer Society (1998) Cancer facts and figures for minority Americans. Atlanta, GA: American Cancer Society.
- Department of Health and Human Services (2012) Study finds racial and ethnic disparities in US cancer screening rates. Centers for Disease Control and Prevention
- Ries LAG, Harkins D, Krapcho M, Mariotto A, Miller BA, et al (2006). SEER Cancer Statistics Review, 1975-2003. National Cancer Institute.
- Miller BA, Kolonel LN, Bernstein L, Young JL, Swanson GM, et al. (1996) Racial/Ethnic patterns of cancer in the United States 1988-1992. National Cancer Institute. NIH Pub: 96-4104.
- Ward E, Jemal A, Cokkinides V, Singh GK, Cardinez C, et al. (2004) Cancer disparities by race/ethnicity and socioeconomic status. CA Cancer J Clin 54: 78-93.
- McCracken M, Olsen M, Chen MS Jr, Jemal A, Thun M, et al. (2007) Cancer incidence, mortality, and associated risk factors among Asian Americans of Chinese, Filipino, Vietnamese, Korean, and Japanese ethnicities. CA Cancer J Clin 57: 190-205.
- Coughlin SS, Uhler RJ (2000) Breast and cervical cancer screening practices among Asian and Pacific Islander women in the United States, 1994-1997. Cancer Epidemiol Biomarkers Prev 9: 597-603.
- Saphir A (1997) Asian Americans and cancer: discarding the myth of the "model minority". J Natl Cancer Inst 89: 1572-1574.
- Su X, Ma GX, Seals B, Tan Y, Hausman A (2006) Breast cancer early detection among Chinese women in the Philadelphia area. J Womens Health (Larchmt) 15: 507-519.
- Tu SP, Yasui Y, Kuniyuki AA, Schwartz SM, Jackson JC, et al. (2003) Mammography screening among Chinese-American women. Cancer 97: 1293-1302.
- Lee-Lin F, Menon U, Pett M, Nail L, Lee S, et al. (2007) Breast cancer beliefs and mammography screening practices among Chinese American immigrants. J Obstet Gynecol Neonatal Nurs 36: 212-221.
- Lovejoy NC, Jenkins C, Wu T, Shankland S, Wilson C (1989) Developing a breast cancer screening program for Chinese-American women. Oncol Nurs Forum 16: 181-187.
- Tang TS, Solomon LJ, McCracken LM (2000) Cultural barriers to mammography, clinical breast exam, and breast self-exam among Chinese-American women 60 and older. Prev Med 31: 575-583.
- Wu TY, Guthrie BJ, Bancroft JM (2005) An integrative review on breast cancer screening practice and correlates among Chinese, Korean, Filipino, and Asian Indian American women. Health Care Women Int 26: 225-246.
- Liang W, Yuan E, Mandelblatt JS, Pasick RJ (2004) How do older Chinese women view health and cancer screening? Results from focus groups and implications for interventions. Ethn Health 9: 283-304.
- Copenhaver MM, Lee IC (2006) Optimizing a community-friendly HIV risk reduction intervention for injection drug users in treatment: a structural equation modeling approach. J Urban Health 83: 1132-1142.
- Ebrahim SH, Anderson JE, Weidle P, Purcell DW (2004) Race/ethnic disparities in HIV testing and knowledge about treatment for HIV/AIDS: United States, 2001. AIDS Patient Care STDS 18: 27-33.
- Van GB, Van HE, Veldhoven M, Zeelenberg M, Croon M (2007) Psychological strain and emotional labor among police-officers: A diary study. J Vocat Behav 71: 446-459.
- Wang MQ, Matthew RF, Bellamy N, James S (2005) A structural model of the substance use pathways among minority youth. Am J Health Behav 29: 531-541.
- Loitman J, Leeman JM (2005) Testing a mediational model of communication among medical staff and families of cancer patients. Struct Equ Modeling 12: 454-470.
- Recklitis CJ, Parsons SK, Shih MC, Mertens A, Robison LL, et al. (2006) Factor structure of the brief symptom inventory--18 in adult survivors of childhood cancer: results from the childhood cancer survivor study. Psychol Assess 18: 22-32.
- Bentler PM (1995) EQS Structural Equations Program Manual. Encino: Multivariate Software, Inc 1-422.
- Joreskog, K. G. (1993). Testing structural equation models. In K. A. Bollen & J. S. Long Eds. 294-316.
- Spoth R, Redmond C, Shin C (1998) Direct And Indirect Latent-Variable Parenting Outcomes Of Two Universal Family-Focused Preventive Interventions: Extending A Public Health-Oriented Research Base. J Consult Clin Psych 66: 385-399.
- Ma GX, Shive SE, Gao W, Tan Y, Wang MQ (2012) Prostate cancer screening among chinese american men: a structural model. Am J Health Behav 36: 495-504.
- Sudman S, Bradburn NM. (1986) Asking questions. San Francisco, CA: Jossey pub.
- Muthén B, Muthén L (2000) Mplus User’s Guide.
- Juon HS, Kim M, Shankar S, Han W (2004) Predictors of adherence to screening mammography among Korean American women. Prev Med 39: 474-481.
- Secginli S, Nahcivan NO (2006) Factors associated with breast cancer screening behaviours in a sample of Turkish women: a questionnaire survey. Int J Nurs Stud 43: 161-171.
- Yi JK, Prows SL (1996) Breast cancer screening practices among Cambodian women in Houston, Texas. J Cancer Educ 11: 221-225.
- Yu ES, Kim KK, Chen EH, Brintnall RA (2001) Breast and cervical cancer screening among Chinese American women. Cancer Pract 9: 81-91.
- Juon HS, Seo YJ, Kim MT (2002) Breast and cervical cancer screening among Korean American elderly women. Eur J Oncol Nurs 6: 228-235.
- Maxwell AE, Bastani R, Warda US (1998) Mammography utilization and related attitudes among Korean-American women. Women Health 27: 89-107.
Relevant Topics
- Addiction
- Adolescence
- Children Care
- Communicable Diseases
- Community Occupational Medicine
- Disorders and Treatments
- Education
- Infections
- Mental Health Education
- Mortality Rate
- Nutrition Education
- Occupational Therapy Education
- Population Health
- Prevalence
- Sexual Violence
- Social & Preventive Medicine
- Women's Healthcare
Recommended Journals
Article Tools
Article Usage
- Total views: 15412
- [From(publication date):
May-2013 - Nov 28, 2025] - Breakdown by view type
- HTML page views : 10623
- PDF downloads : 4789