Zoonotic Sporotrichosis: Series of Cases from Non-Endemic Region
Received: 31-May-2017 / Accepted Date: 21-Mar-2018 / Published Date: 27-Mar-2018
Abstract
Sporotrichosis is a mycosis caused by the fungus of the Sporothrix schenckii complex, saprophytes in nature, common in thorns and vegetables that can affect both humans and animals. An increase in the number of cases of zoonotic transmission of sporotrichosis in the state of Minas Gerais-Brazil, where the disease was previously associated only with professional or accidental transmission, (such as gardeners), who warns of a possible change in the epidemiological profile, in which the cat is a vector. We described the cases of three patients from related areas. They all had contact with domestic cat affected by cutaneous involvement disease.
Keywords: Dermatosis; Infectious dermatosis; Sporotrichosis; Sporothrix schenckii; Itraconazole
Introduction
Sporotrichosis is a mycosis caused by the fungus of the Sporothrix schenckii complex, saprophytes in nature, common in thorns and vegetables that can affect both humans and animals.
The main clinical manifestations of the disease are cutaneouslymphatic and localized cutaneous forms, and can evolve with systemic dissemination.
The cutaneous-lymphatic is the most common form, which occurs in about 70-90% of the cases. Transmission may occur through the traumatic inoculation of contaminated material through the skin, in addition to scratches or bites of felines infected with Sporothrix schenckii [1].
We described the cases of three patients from related areas. They all had contact with domestic cat affected by cutaneous involvement disease.
Communication Reports
Case 1
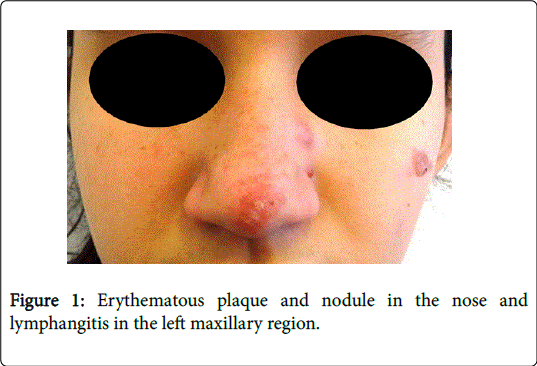
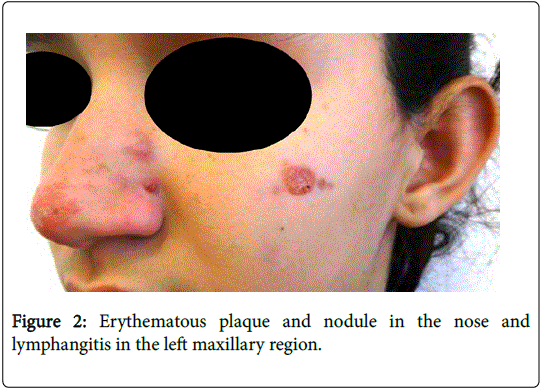
An 11-year-old female patient from Zona da Mata region, Minas Gerais, Brazil, was referred to the department of dermatology with an erythematous plaque and nodule in the nose, likewise lymphangitis in the left maxillary region with one month of evolution (Figures 1 and 2). She denied systemic symptoms and comorbidities.
She reported that two months ago her domestic cat had ulcers on the skin and evolved to death. She refused to perform biopsy of the lesions. Initiated the treatment with oral potassium iodide, but she presented intolerance (iodine allergy) being replaced by itraconazole 200 mg/day. She obtained a progressive improvement of the clinical picture.
Case 2
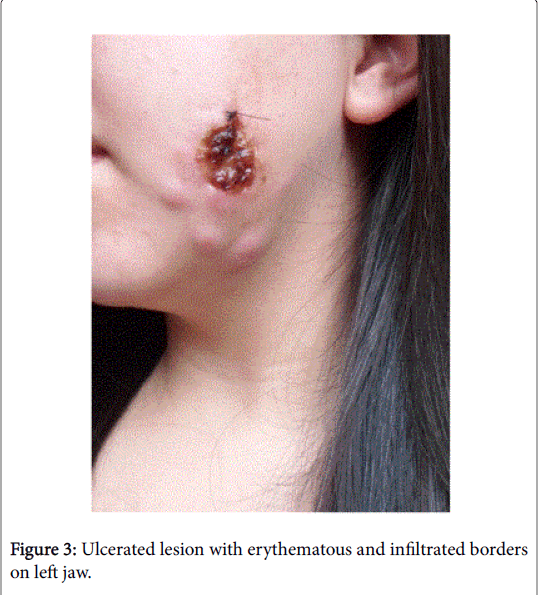
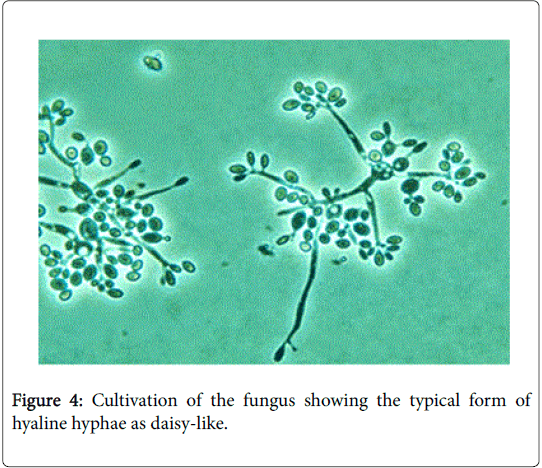
A 23-year-old female patient from Zona da Mata region, Minas Gerais, Brazil, attended the dermatology service with a report of a nodule in the submandibular region for a month that evolved with central ulceration and exudation in the last 15 days. She denied comorbidities and use of medications. She reported contact with a domestic cat that presented cutaneous involvement disease, treated with ketoconazole, with complete improvement of the lesions. On examination, the patient presented ulcerated lesion with erythematous and infiltrated borders, with a moist crust and purulent exudate in the ramus region of the left mandible with submandibular lymph node enlargement (Figure 3). In the fungal culture, the fungus Sporothrix schenckii (Figures 4 and 5) was isolated. Treatment with itraconazole 200 mg/day was started, with progressive improvement of the lesion.
Case 3
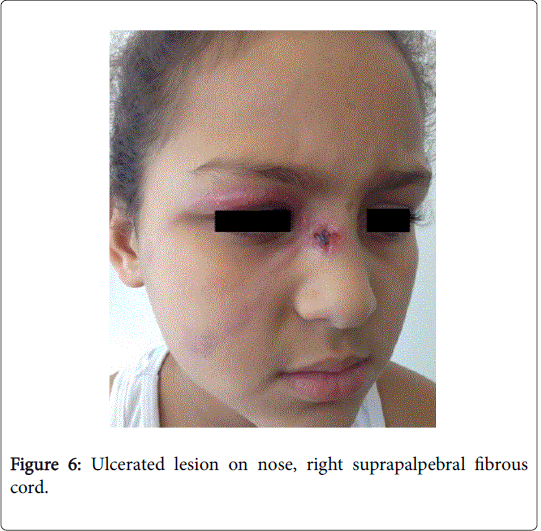
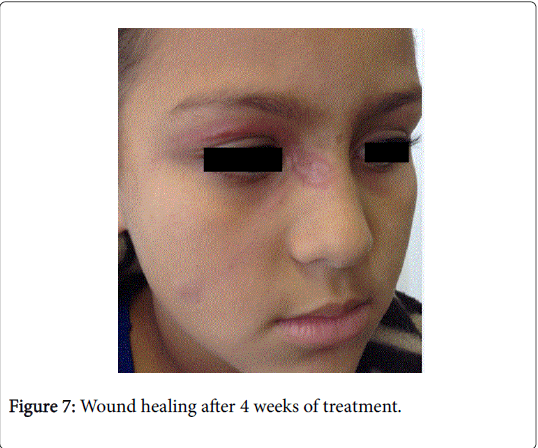
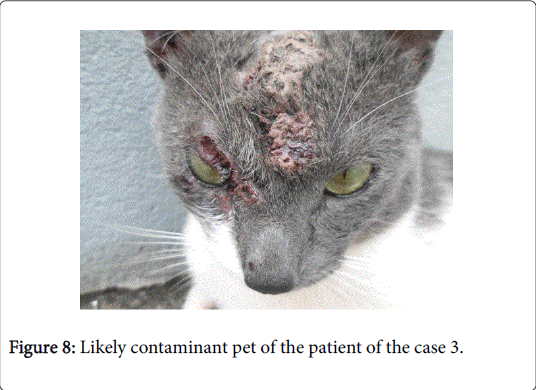
An 8-year-old female patient, born and resident in Zona da Mata, Minas Gerais, Brazil, presented nodule formation in the right nasal region in November 2015, which evolved with local edema, drainage of purulent secretion and, later, with the formation of ulcerated lesion. One month later, the patient was treated by a dermatologist and at the time had an ulcerated lesion in the right nasal region, with a fibrous cord in the upper eyelid and maxillary region and lymph nodes in the submental region (Figure 6). She denied systemic signs and previous pathologies. She reported that she had a cat and it had an ulcerated lesion on its face. Before 15 days of the onset of the injury, the patient was scratched by the cat. Scraping of the lesion and culture of the collected material was performed, where Sporothrix schenckii was isolated. The treatment was initiated with itraconazole 100 mg/day. The patient remained in outpatient follow-up, presenting involution of the lesion (Figure 8). The feline evolved to death 10 days after this incident (Figure 8).
Discussion
Sporothrix schenckii is a pathogenic, dimorphic, cosmopolitan fungus found in soil and in decaying organic matter. It infects felines, dogs, wild animals and humans. Cats are among the main vectors of the zoonotic form of the disease and when infected they present a high fungal load [2]. The zoonotic transmission of sporotrichosis has been shown to be highly incident in the state of Rio de Janeiro (RJ-Brazil) [1].
A family outbreak of zoonotic sporotrichosis in the state of Espirito Santo (ES-Brazil) has been reported in which we can see similarities with cases in RJ: in the two regions the affected patients presented contact with felines [3].
An increase in the number of cases of zoonotic transmission of sporotrichosis in the state of Minas Gerais-Brazil, where the disease was previously associated only with professional or accidental transmission, (Such as gardeners), who warns of a possible change in the epidemiological profile, in which the cat is a vector.
The characteristics of the lesions depend on factors such as: the host's immune status, the size of the inoculum and the pathogenicity of the fungus. The cutaneous-lymphatic form presents as an ulcerated, crusty, infiltrated lesion that evolves into ascending regional lymphadenomegaly.
Localized cutaneous form is the second most common clinical form (20% of the cases), it occurs frequently in children and individuals with good immune response. The Disseminated form occurs in immunocompromised patients such as diabetics, transplanted patients and chronic alcoholics. It occurs hematogenously and courses with subcutaneous lesions that ulcer after weeks.
Extra-cutaneous forms correspond to less than 5% of the cases and relate to the affected organs, such as lungs and bones. In the reported cases, whose clinical form was cutaneous-lymphatic, erythematous plaque, ulcerated nodules and satellite lymphangitis were observed [4]. Lesions with such aspects, added to the positive clinical history for contact with contaminated felines, should always have sporotrichosis as a diagnostic hypothesis.
The diagnosis of sporotrichosis is based on the clinical history, epidemiology and culture of secretion/scraping of the positive lesion for Sporothrix schenckii in the medium of Sabouraud-dextrose agar, which presents growth of 3-5 days, but can take up to 1 month.
Initially it looks white or cream and wrinkled, brown or black. Under culture microscopy appear hyaline, septate and conidia hyphae as daisy-like (Figure 5). Even the histopathological examination is not specific, it is useful to the diagnosis and evidences the presence of pseudoepitheliomatous hyperplasia and granulomatous reaction [5].
Conclusion
The literature recommends the use of itraconazole or potassium iodide for the cutaneous-localized and cutaneous-lymphatic clinical forms. For patients who are allergic to azole and/or potassium iodide, terbinafine is the therapeutic option. The physician should be alert to immunosuppressed patients and to cases that do not respond well to initial treatment, which may develop with disseminated or extracutaneous lesions. The prognosis in these cases varies according to the clinical form presented. It is important to treat contaminated animals, wear gloves and boots when coming into contact with plants [6].
References
- Freitas DF, do Valle AC, Almeida-Paes R, Bastos FI, Galhardo MC (2010). Zoonotic sporotrichosis in Rio de Janeiro, Brazil: A protracted epidemic yet to be curbed. Clin Infect Dis 50: 453-454.
- Barros MB, Schubach Ade O, do Valle AC, Gutierrez Galhardo MC, Conceicao-Silva F, et al. (2004) Cat-transmitted sporotrichosis epidemic in Rio de Janeiro, Brazil: description of a series of cases. Clin Infect Dis. 38: 529-535.
- Oliveira MME, Maifrede SB, Ribeiro MA, Oliveira RMZ (2013) Molecular identification of Sporothrix species involved in the first familial outbreak of sporotrichosis in the state of Espirito Santo, southeastern Brazil 108: 936-938.
- Kauffman CA, Bustamante B, Chapman SW, Pappas PG (2007). Clinical practice guidelines for the management of sporotrichosis: 2007 update by the Infectious Diseases Society of America. Clin Infect Dis 45:1255-1265.
- Barros MBL, de Almeida P, Schubach AO (2011) Sporothrix schenckii and Sporotrichosis. Clin Microbiol Rev 24: 633-654.
- Rosa ACM, Scroferneker ML, Vettorato R, Gervini RL, Vettorato G, et al. (2005) Epidemiology of sporotrichosis: A study of 304 cases in Brazil. J Am Acad Dermatol 52: 451-459.
Citation: Neto MPM, Rocha GP, de Oliveira WLG, Freire ES, Bastos BF, et al. (2018) Zoonotic Sporotrichosis: Series of Cases from Non-Endemic Region. Cosmetol & Oro Facial Surg 4: 129.
Copyright: © 2018 Neto MPM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Open Access Journals
Article Usage
- Total views: 5352
- [From(publication date): 0-2018 - Mar 12, 2025]
- Breakdown by view type
- HTML page views: 4655
- PDF downloads: 697