Case Report Open Access
Xenograft Bone-Guided Regeneration of the Foot in Case of Metastatic Bladder Carcinoma causing Pathological Fracture
Igor Frangez1*, Tea Nizic Kos1, Marina Mencinger2, Dragica Maja Smrke1 and Matej Cimerman1
1Department of Traumatology, University Medical Centre Ljubljana, Zaloška cesta, Ljubljana, Slovenia
2Institute of Oncology Ljubljana, Zaloska cesta, Ljubljana, Slovenia
- Corresponding Author:
- Igor Frangez
Department of Traumatology
University Medical Centre Ljubljana
Zaloška cesta 2, 1525 Ljubljana, Slovenia
Tel: 00386 41682112
E-mail: ifrangez@gmail.com
Received Date: September 06, 2016; Accepted Date: October 26, 2016; Published Date: October31, 2016
Citation: Frangez I, Kos TN, Mencinger M, Smrke DM, Cimerman M (2016) Xenograft Bone-Guided Regeneration of the Foot in Case of Metastatic Bladder Carcinoma causing Pathological Fracture. Clin Res Foot Ankle 4:213. doi:10.4172/2329-910X.1000213
Copyright: © 2016 Frangez I, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Clinical Research on Foot & Ankle
Abstract
Background: Bladder carcinoma with distal bone metastasis is rare. Treatment should be multidisciplinary, including pain relief, treatment of threatening (or) pathological fractures, and oncologic therapy for bladder cancer.
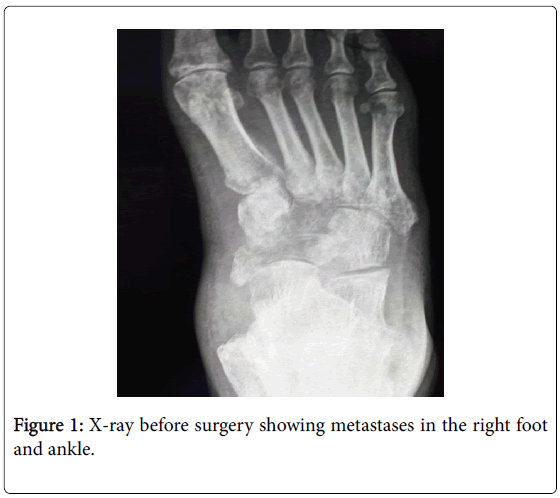
Case report: A 52-year-old male patient with bladder cancer reported having pain in the right foot and ankle. Xray and CT revealed multiple bone metastases of bladder cancer to the right foot and ankle, causing pathological fractures. The patient refused proposed below-knee amputation, therefore, preservative surgery with metastasectomy of larger metastases in the foot and ankle, and distal fibulaectomy were performed. To fulfill the defects in the foot, bone guided regeneration with equine xenograft bone block and collagen membrane was performed and additionally stabilized with osteosynthetic material. Two months after surgery, the bone graft was incorporated into the bone and the patient was capable of weight bearing, pain-free, and able to continue with chemotherapy and radiation therapy. Despite the therapy, the patient died of embolism due to metastasis 6 months following the foot operation.
Discussion: The aim of our case report is to show that amputation is not the only method of treatment for patients with multiple metastases of the foot and ankle. Alternatively, bone-guided regeneration with xenograft can be successfully performed also in such patients. Rehabilitation following bone-guided regeneration is shorter compared to amputation, and also enables a better quality of life.
Keywords
Bone-guided regeneration; Xenograft; Pathological fracture; Osteosynthesis; Bladder carcinomas; Acrometastasis
Introduction
Metastases in patients with spread cancer are often located in the skeleton, mostly in large bones or spine, but are rarely reported in the foot and ankle [1-8]. The treatment of metastatic disease is systemic therapy with additional local therapy if indicated [1]. Metastases in the bone can cause pain due to pathological fractures [1-8]. In cases of threatening fractures, preventive surgical stabilization is recommended [8]. In our case report, we present the case of large metastases in the foot and ankle, treated with metastasectomy and bone-guided regeneration using equine bone xenograft and collagen membrane, and additionally stabilized with an osteosynthetic plate.
Case Report
A 52-year-old Caucasian male patient with an urothelial carcinoma of the bladder and metastases in lungs and the right foot and ankle was presented to a foot and ankle specialist for local treatment of pathological fractures in the right foot and ankle. Two options of operative treatment were discussed: a below-knee amputation and a preserving operation. Since the patient refused an amputation, a preserving operation was performed. The operative procedure included metastasectomy, followed by bone-guided regeneration with xenograft and additional internal fixation with a plate and intramedullary nail. A heterologous collagen membrane was used as a cover over the bone xenograft and the osteosynthetic material to facilitate and accelerate the physiological regeneration process (Figure 1).
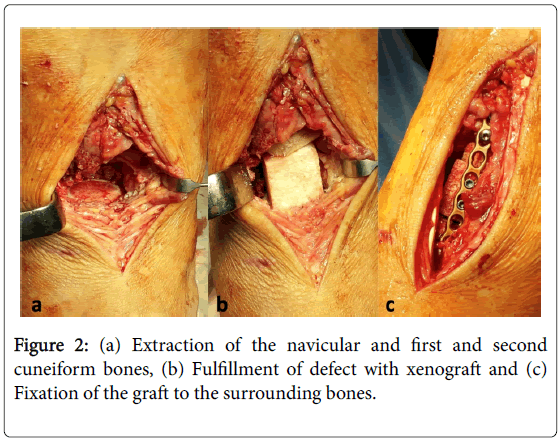
Through dorsomedial incision naviculare, the first and second cuneiform bones were extracted. Bone defect was replaced with equine bone block xenograft and collagen membrane (OsteoBiol -Tecnoss), additionally stabilized using titanium LCP plate 2.7 and an intramedullary nail through the medial column (Synthes). Additionally, distal fibulectomy was performed due to a large metastasis. The remaining distal part of the fibula was fixated to the tibia using a transsyndesmotic screw. A large metastasis in the lateral part of distal tibia was excochleated, with preservation of the articular cartilage. Bone defect was fulfilled with antibiotic cement (Figure 2).
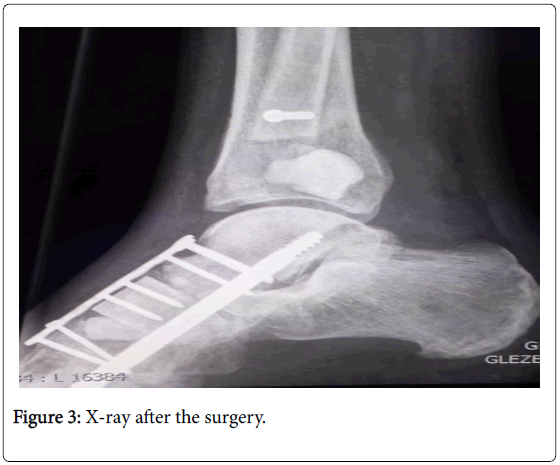
The patient did not require additional immobilization of the operated foot. One day after the surgery, he was mobilized with crutches, offloading the operated foot. Two weeks after the surgery, he started with radiotherapy treatment. He had regular control examinations with the foot and ankle surgeon, including an X-ray every two weeks (Figure 3). After 4 weeks, partial weight bearing was allowed. After 8 weeks the patient was able to fully load the operated foot without pain.
Oncologic treatment continued, but despite two cycles of standard chemotherapy combination, an advance in the growth of the primary tumor and the lungs metastasis were noticed. The patient died 6 months after the surgery (prior planned CT scan) due to pulmonary embolism.
Discussion
According to literature, a third of cancer patients have bone metastasis, while metastases of the foot and ankle are reported quite rarely (in less than 0.02%) [1-8]. Surgical treatment is necessary if they cause or threaten to cause pathological fractures [8].
There were two options presented to our patient. The first was below-knee amputation and the second was a preserving operation. Since the second option allowed a shorter rehabilitation period and a better quality of life, including the psychological benefits of preserving the leg, both the patient and surgeon who already had encouraging results with tissue (bone) guided regeneration opted for preservative treatment [9]. Bone defects, especially in weight-bearing bones, need to be fulfilled with suitable grafts. Bone grafting is usually performed with the autologous bone taken from the iliac crest.
Autologous bone grafts are a gold standard of bone repair and regeneration, but donor site, represents the additional origin of pain and possible complications like bleeding or infection that are avoided in use of other substitute materials. Bone allografts are available in various geometric and shapeable forms, but the material must come from a reputable tissue bank and might not always be available. In our case, a strong graft was needed to enable early weight bearing. Different mineral-based biomaterials are used in clinical practice, such as hydroxyapatite alone or mixed with cancellous bone marrow or ceramic, cell, polymer or factor-based materials [10-12]. To restore the defect after metastasectomy in distal tibia, where distally only the articular cartilage remained, we decided to use antibiotic cement. Since there was no option of performing stabilization of the distal tibia with osteosynthesis, we decided on a material that retains its shape and has the required strength in vertical axis that was needed.
In the foot, where forces are transferred to the horizontal line, we decided for a stronger material that we were able to fixate with osteosynthesis in order to enable early weight bearing. Since we already had a good experience with use of xenograft in fulfillment of bone defects in foot surgery and since xenograft is always available in our institution we prefer to use it compared to other bone substitutes. To achieve optimal results we used the principles of bone-guided regeneration.
Bone guided regeneration, developed in 1976 by Melcher, uses the basic principle of different speed potentials of cellular components, that migrate into the bone defect during the healing process [13]. A mechanical barrier, in our case a collagen resorbable membrane, prevents ingrowth of unwanted cells and allows the passage of desired cells. In the case of bone surgery, osteoprogenitor cells are favorable to the site of the defects.
In our patient bone defects after metastasectomy in the foot were filled with equine xenograft bone block and additionally stabilized with plates. This is, according to our knowledge, a rare case in extant literature—the use of xenograft which (according to the X-ray) incorporated into the bone structure and biomechanically allowed full weight bearing of the leg in 8 weeks, with no other clinical manifestations such as pain, swelling or infection. The patient’s pain due to the metastases was immediately relieved. Moreover, his quality of life in the remaining six months of life was significantly better compared to the option of amputation that requires a longer rehabilitation period. Bone-guided regeneration with xenograft after metastasectomy enabled pain relief, and resulted in far greater independence compared to amputation. It is worthy of note that the patient in our case was relatively young and, despite spread carcinoma, still fully active. This fact justified our treatment approach. Considering that bone-guided regeneration using xenograft and collagen membrane was successful in our case, we believe that this option could be considered in similar cases of preservative bone surgery.
References
- Shinagare AB, Ramaiya NH, Jagannathan JP, Fennessy FM, Taplin ME, et al. (2011) Metastatic pattern of bladder cancer: correlation with the characteristics of the primary tumor. Am J Roentgenol 196:117-122.
- Jacofsky DJ,Frassica DA, Frassica FJ (2004) Metastatic disease to bone. Hospital Physician 39:21-28.
- Petkovi? M, Muhvi? D, Zamolo G, Jonji? N, Musta? E, et al. (2004) Metatarsal metastasis from transitional cell cancer of the urinary bladder. CollAntropol28:337-341.
- Khan S, Win Z, Lloyd CR, Neriman D, Szyszko TA, et al. (2007) Acrometastasis to the foot: an unusual presentation of transitional cell carcinoma of the bladder. Nucl Med Rev Cent East Eur 10:26-28.
- Yadav S, Kumar R (2015) Solitary second metatarsal metastasis as the first site of distant spread in TCC urinary bladder: A case report. Indian J Urol 31:363-365.
- Sedmak B (2003) Malignitumorjimehurja. ZdrVestn 72: 27-31.
- Ryder JH, McGarry SV, Wang J (2013) Calcaneal acrometastasis from urothelial carcinoma of the ureter: a case report and literature review. ClinInterv Aging 8:395-399.
- Hipp JA, Springfield DS, Hayes WC (1995) Predicting pathologic fracture risk in the management of metastatic bone defects. ClinOrthopRel Res. pp: 120–135.
- Frangez I, Kasnik T, Cimerman M, Smrke DM (2016) Guided tissue regeneration with heterologous materials in primary subtalar arthrodesis: a case report. J Med Case Rep 10:108.
- Nandi SK, Roy S, Mukherjee P, Kundu B, De DK, et al. (2010) Orthopaedic applications of bone graft & graft substitutes: a review. Indian J Med Res 132:15-30.
- Parikh SN (2002) Bone graft substitutes: past, present, future. J Postgrad Med48:142-148.
- Finkemeier CG (2002) Bone-grafting and bone-graft substitutes. J Bone Joint Surg Am 84: 454-464.
- Melcher AH (1976) On the repair potential of periodontal tissues. J Periodontol 47:256-260.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 11572
- [From(publication date):
November-2016 - Apr 07, 2025] - Breakdown by view type
- HTML page views : 10686
- PDF downloads : 886