Research Article Open Access
Work-related and Dietary Factors Associated with Weight Gain over the Period of Employment in Paramedics
Sandrine Hegg-Deloye1-3, Philippe Corbeil1,4*,Patrice Brassard1,2, Jérôme Prairie1,4, Dominique Larouche1,4, Nathalie Jauvin3, Pierre-Hugues Carmichael4, Paul Poirier2 and Angelo Tremblay1,21Department of Kinesiology, Laval University, Quebec City, QC, Canada
2University Institute of Cardiology and Pneumology, Laval Hospital, Laval University, Quebec City, QC, Canada
3Research Team RIPOST, CSSS De la Vieille Capitale (CAU), Quebec City, QC, Canada
4Center of Excellence on Aging Quebec Research Centre of the University Hospital of Quebec, Quebec City, QC, Canada
- *Corresponding Author:
- Philippe Corbeil
Faculty of Medicine
Department of Kinesiology
Laval University, Quebec, QC
G1V 0A6, Canada
Tel: 418-656-5604
E-mail: philippe.corbeil@kin.ulaval.ca
Received date: June 04, 2014; Accepted date: August 01, 2014; Published date: August 07, 2014
Citation: Hegg-Deloye S, Corbeil P, Brassard P, Prairie J, Larouche D et al. (2014) Work-related and Dietary Factors Associated with Weight Gain over the Period of Employment in Paramedics. Occup Med Health Aff 2:173. doi: 10.4172/2329-6879.1000173
Copyright: © 2014 Hegg-Deloye et al.This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Occupational Medicine & Health Affairs
Abstract
Background: Recent studies reported high body mass index values in paramedic, with a high percentage of workers being considered overweight or obese. However, little evidence exists regarding which factors explained weight gain over time in paramedics. Objective: This study evaluated whether occupational stress, tobacco consumption, sleeping problems or emotional food disinhibition were associated with weight gain over time in paramedics compared to a control group. Method: A retrospective study was performed. The study consisted in a self-report questionnaire composed of 84 questions related to sleeping problems, emotional food disinhibition, tobacco consumption and occupational stress. Occupational stress was evaluated through lack of social support and effort-reward imbalance. A repeated measures regression model was used to explore relationships between body mass index (BMI) and characteristics related to employment. Results: Questionnaires from 283 controls and 295 paramedics were analyzed. Paramedics, but not controls, gained BMI over the period of employment, as shown by a significant interaction between Time and Occupation (F(2, 568)=6.28; p=.002). Men were more likely to gain BMI over the period of employment (F(1,568)=42.95; p<. 0001). Among all covariates tested, tobacco consumption (F(1,568)=5.68; p=.02), supervisor support (F(1,568)=5.25; p=.02) and emotional disinhibition of eating (F(3,568)=7.51; p<.0001) had a significant effect on BMI for both groups. Conclusion: Paramedics experienced a greater increase in BMI over their years of employment than controls, often leading to obesity. These findings suggest that both work environment and organizational factors influence weight gain among paramedics and other workers.
Keywords
Occupational stress; Obesity; Emergency worker; Eating behaviors; Work-related factors
Introduction
Background
The prevalence of obesity is constantly growing, leading to an increase in the prevalence of obesity-related work disabilities [1]. Several factors are known to contribute to overweight or obesity, including factors related to eating behavior (e.g., dietary restraint and disinhibition), psychological factors, occupational stress, working conditions (e.g., long working hours and physically demanding jobs), sociocultural factors and sleeping problems [2,3]. Disinhibition eating behavior, defined as the tendency to overeat in response to a stimulus (e.g., occupational stress) [4], is strongly associated with weight gain over time and with obesity in adult life [5]. Occupational stress is caused by psychosocial conditions such as high job strain (i.e., high psychological demands and low decision latitude), which has been identified as a risk factor for higher body mass index (BMI) [2]. Lack of social support and effort-reward imbalance have also been proposed to contribute to weight gain; however, no consistent evidence has been reported [6,7]. Stressful working conditions (i.e., time pressure) can influence food choices, eating patterns, tobacco consumption and result in low levels of leisure-time physical activity [2,8]. In particular, emotional eaters who consume food when they are under stress consume more sweet and fatty foods or sugary drinks than unstressed and non-emotional eaters [9,10]. In addition, acute psychological stress has been associated with eating in the absence of hunger, especially in vulnerable individuals who display disinhibited eating behavior and sensitivity to chronic stress [11].
Paramedics constitute a group of workers who are required to rescue people as quickly and efficiently as possible. To achieve this goal, paramedics may put their own lives at risk. Their everyday occupational stress is characterized by organizational and psychosocial challenges that may represent stressors. These organizational challenges include, for example, workload, shift work, pressure to achieve rapid response times, economic efficiency and variable waiting periods between calls [12]. Moreover, their mealtimes depend on their workload and vary depending on the number of calls in a day and their timing [12]. In accordance with Selye’s theory [13], persistent exposure to stressors may progressively lead to maladaptive outcomes such as the development of mental health impairments, metabolic syndrome, obesity and cardiovascular disease [14].
A recent study reported high BMI values in paramedic recruits and office workers, with a high percentage of workers being considered overweight or obese [15,16]. Another study reported high perceived stress, lack of leisure time and increased prevalence of obesity among pre-hospital emergency professionals [17]. Further, several studies have reported that a high percentage of paramedics – 62% in Sweden, 100% in the USA and 93% in Germany – experienced acute stress during their shifts, especially in situations involving management of their own emotions [18-21]. The overall prevalence of post-traumatic stress disorder in emergency ambulance personnel is higher than in the general population (20% versus 5%) [22,23]. Among office workers, it has been suggested that chronic work stress predicts general and central obesity [16]. To our knowledge, no study has established an association between work-related factors and weight gain among paramedics, if any.
The aim of this study was therefore to assess whether work-related occupational stress, tobacco consumption, dietary behavior at work and sleeping problems are associated with increased BMI among paramedics in comparison with a control group of general workers.
Subjects and Methods
Subject
A retrospective study was conducted during the fall and winter of 2011 among paramedics and a control group in the province of Quebec. Participants were recruited via an electronic mailing list and word of mouth. All paramedics and control group individuals were required to work at least 20 h/week and they were over 18 years old. The control group represented the general population, including office workers, university staff, self-employed people, marketers, salespeople and research center staff. In the province of Quebec, the paramedic population totals approximately 3000 workers. Three hundred respondents were desired in each group. The final sample included 283 controls and 295 paramedics. Ethical approval for the study was obtained from the institutional ethics committee and informed consent was obtained from all participants.
Method
The study consisted in a self-report questionnaire composed of 84 items. The first portion of the questionnaire contained 18 items that identified age, height, body weight, during the first year in employment and current age, current height, current body weight, current tobacco consumption and current date. The body mass index was calculated for the first year in employment and for the current date. Body mass index (BMI), defined as weight in kilograms divided by the square of the height in meters (kg/m2). Subjects were considered overweight when the BMI was greater than 25 kg/m2.
Sleeping problems were evaluated using the Pittsburgh Sleep Quality Index [24]. This questionnaire is designed to assess sleep quality across seven dimensions: subjective sleep quality (representing the overall quality of sleep), sleep latency (amount of time taken to fall asleep), sleep duration (number of hours of actual sleep per night), habitual sleep efficiency (number of hours of sleep divided by number of hours spent in bed), daytime dysfunction (trouble staying awake or decreased energy during the day), sleep medication and sleep disturbance (trouble during sleep). In this study, we excluded two dimensions (sleep medication and sleep disturbance), as they are typically evaluated by the participant’s spouse. Participants indicated their usual bedtime, how long it usually takes them to fall asleep, their usual waking time and the usual hours of sleep obtained per night. They answered questions on a 4-point Likert-type scale (0=not during the past month, 3=three or more times a week). The Pittsburgh Sleep Quality Index has internal consistency and a reliability coefficient (Cronbach’s alpha) of 0.83 for its seven components. A global score of more than 3 out of 15 indicated sleeping problems associated with health consequences [24].
Organizational and psychosocial factors at work were evaluated with the French version of the Job Content Questionnaire and effort-reward model [25-27]. The Job Content Questionnaire measures psychological demands and decision latitude. Psychological demands refer to the quantity of work, intellectual requirements, and time constraints. Participants with a combination of high psychological demands and low job decision latitude composed the high-job-strain group. Social support evaluates support from co-workers and supervisors, as social support is considered a moderator of tensions felt at work [26]. The Job Content Questionnaire has internal consistency and a reliability coefficient (Cronbach’s alpha) of 0.65. The effort-reward model was used to measure the imbalance between efforts at work and rewards [27]. Effort refers to the psychological and physical constraints at work and also to behaviors associated with excessive involvement in work. Reward refers to salary, esteem and control over the participant’s own professional status (e.g., opportunities for promotion, job security). For each question, there are four levels to choose from, ranging from strongly disagree to strongly agree. A ratio of greater than 1 indicated an imbalance between effort and reward, which is harmful to health [27]. The effort-reward model has internal consistency and a reliability (Cronbach’s alpha) of 0.75 for effort dimensions and 0.86 for reward. Disinhibition and hunger were evaluated with the Eating Inventory Three Factor Eating Questionnaire (TFEQ), also known as the [28,29]. Disinhibition (habitual, emotional and situational disinhibition) reflects loss of control over eating in response to the presence of palatable food or other disinhibiting stimuli, such as emotional distress. Hunger refers to the appetite for a meal induced by internal and external loci [28,29]. Responses are scored as 0 or 1 and summed. Higher scores on the respective scales are indicative of disinhibited eating and predisposition to hunger [28]. The TFEQ has internal consistency and a reliability coefficient (Cronbach’s alpha) of 0.91 for disinhibition and 0.85 for hunger [28]. Eating habits were also evaluated with the following question: “What do you eat most often for lunch when you are working?” Participants were asked to select one of three possible responses: homemade meal, meal at a restaurant, or food delivery or pickup from a local restaurant.
Statistical analyses
Of the 295 paramedics and 283 controls who responded, none had missing data and all subjects were included in the statistical analysis. For each part of the questionnaire, a coding system was used to generate specific scores for each item and a percentage for each item was calculated. Then, a repeated measures regression model based on a mixed model approach was used to explore the relationships between BMI (first year of employment, date of maximum BMI, and current date), occupational categories, sleeping problems, psychological demand, decision latitude, social support, effort-reward imbalance, emotional food disinhibition, restaurant meals and hunger (Proc MIXED, SAS software, SAS Institute Inc., Cary, NC) [30]. A first model was constructed using occupation, age, gender, time at current job and possible interactions with other workers to create the adjustment model. Then each additional occupation-by-covariate interaction was individually added to the adjustment model and tested at a 20% alpha level to eliminate truly unremarkable interactions. Finally, a backward selection procedure was used to select a final model from the full model that included the adjustment model, each covariate and all interactions identified in the second step. Exclusion from the one-way ANOVA and model was at the 5% level.
Results
Characteristics of study subjects
Two hundred and eighty three questionnaires from the control group including 73% women and 27% men, and 295 from the paramedics, including 26.4% women and 73.6% men, were analyzed. The control group was a group of office and other workers with a standard day shift and no time pressure (Table 1). At the beginning of employment, the mean BMI was 26.1 ± 4.8 (± standard deviation) for the paramedics and 23.7 ± 4.5 kg/m2 for the control group (Table 2). In 2011, the BMI for each group was 28.0 ± 5.6 and 26.6 ± 4.3 kg/m2, respectively. The percentages of workers in each profession with sleeping problems, organizational and psychosocial contributors, tobacco use, disinhibited eating, predisposition to hunger, and frequent consumption of restaurant meals are presented in Table 3.
| Percent by employment type | Age | BMI | |
| (%) | Mean (95% CI) | Mean (95% CI) | |
| University employees | 33 | 35.9 (33.3–38.4) | 24.7 (23.9–25.6) |
| Government employees | 18 | 32.2 (29.3–35.1) | 24.4 (23.0–25.8) |
| Salespeople | 15 | 28.6 (26.0–31.5) | 25.1 (23.6–26.6) |
| Research center staff | 8 | 26.6 (23.6–29.5) | 25.8 (23.7–27.9) |
| Others | 7 | 31.5 (23.9–38.2) | 24.8 (23.3–26.5) |
| Bank employees | 6 | 39.7 (33.2–46.2) | 25.3 (23.6–27.0) |
| Hospital employees | 6 | 28.7 (24.6–32.8) | 24.7 (22.7–26.7) |
| Servers | 4 | 27.9 (21.2–34.6) | 24.0 (21.9–26.0) |
| Self-employed | 3 | 41.6 (27.9–55.3) | 25.4 (21.3–29.5) |
| BMI: Body mass index (kg/m2) | |||
Table 1: Control group composition (n=283)
| Variables | Control group | Paramedics | ||||||
| 1st year of employment | Max – 1st year | Current – 1st year | 1st year of employment | Max – 1st year | Current – 1st year | |||
| Age | 25.8 (24.8 –26.8) | – | – | 24.2 (23.6–25.0) | – | – | ||
| Body mass index (kg/m2) | 23.7 (23.2–24.2) | 2.7 (2.3–3.1) | .9 (.6–1.3) | 26.1 (25.5–26.6) | 3.8 (3.4–4.2) | 1.9 (1.5–2.3) | ||
| Years of employment | – | 2.6 (1.5–3.5) | 6.9 (6.1–7.7) | – | 7.3 (6.3–8.2) | 11.6 (10.6–12.5) | ||
| Values: mean (95% confidence interval). Max: maximum body mass index. | ||||||||
Table 2: Descriptive statistics: Age, BMI and years of employment for paramedics and controls
| Control group | Paramedics | P value | |
| Daily smokers | 7 (4–10) | 15 (10–19) | 0.001 |
| High psychological demand | 54 (48–60) | 62 (56–68) | 0.091 |
| Low decision latitude | 34 (28–40) | 34 (29–39) | 0.851 |
| Low supervisor support | 21 (16–26) | 53 (47–59) | <.001 |
| Low co-worker support | 20 (15–25) | 31 (26–36) | 0.003 |
| Effort-reward imbalance | 38 (32–44) | 89 (85–93) | < .001 |
| Sleeping problem | 78 (73–83) | 84 (80–88) | 0.066 |
| High disinhibition | 16 (12–20) | 8 (5–11) | 0.001 |
| Predisposition to hunger (internal) | 22 (17–27) | 31 (26–36) | 0.12 |
| Predisposition to hunger (external) | 16 (12–20) | 19 (14–24) | 0.456 |
| Restaurant meals | 13 (9–17) | 30 (25–35) | < .001 |
| P-value obtained from the Z-test (p-values adjusted with Bonferroni method) used to compare proportions between the two independent groups.Daily smokers ≥ 1 cigarette/day; High psychological demand score >7; High decision latitude score ≥72; High hierarchical support score >15; High peer support score >18; Effort-reward imbalance ratio >1; Sleeping problem score ≥ 3; High disinhibition (disinhibited eating >2); Predisposition to hunger (internal or external) >3; Restaurant meals include meals at a restaurant, food delivery or pickup from local restaurants. | |||
Table 3: Percentages with 95% confidence interval of controls and paramedics with tobacco consumption, occupational stress indicators, sleeping problems and dietary behavior
Main results
A significant interaction between Time and Occupation was found (F(2, 568)=6.28; p=.002; Table 4). On average, the paramedics had a higher BMI at each time point than the controls and reached a higher maximum weight (ps<.04). Paramedics had a higher BMI currently than when they were hired for their job (p<.0001). No such significant increase was observed for controls (p=.08). No other interaction was found between occupation and covariates.
| Time | Controls | Paramedics | P-value | ||
| BMI estimate | Standard error | BMI estimate | Standard error | Controls vs. Paramedics | |
| 1st year of employment | 25.72 | 0.4 | 26.62 | 0.39 | 0.04 |
| Maximum body mass index | 27.47† | 0.42 | 29.31† | 0.4 | < .001 |
| Current date | 26.09 | 0.39 | 27.71‡ | 0.38 | < .001 |
| † Significant difference between 1st year of employment and time of maximum body mass index (p < .0001); ‡ Significant difference between 1st year of employment and current date (p < .0001). | |||||
Table 4: Results of the significant interaction between occupation and time: Least squares means for BMI
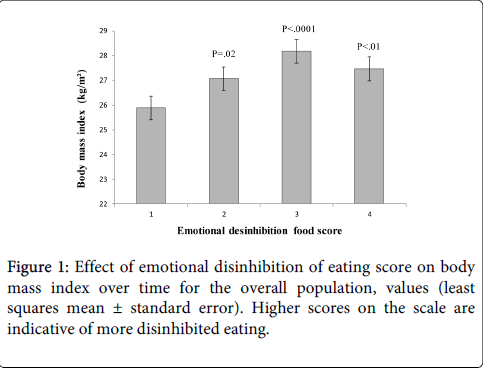
Men were more likely to gain BMI over the period of employment (F(1,568)=42.95; p<.0001). The final model showed also that tobacco consumption (F(1,568)=5.68; p=.02), social support from supervisors (F(1,568)=5.25; p=.02) and emotional disinhibition of eating (F(3,568)=7.51; p<.0001) had a significant effect on BMI. Workers who smoked fewer cigarettes during the day had a lower risk of gaining weight over the period of their employment. As for supervisor support and emotional eating, workers with higher supervisor support and lower emotional food disinhibition had a lower risk of weight gain over the period of employment (Figure 1). Workers who had the habit of eating homemade meals had an average BMI 1 point lower than those who ate mainly restaurant meals. This difference is nearly significant (F(2,568)=2.87; p=.06). Co-worker support, decision latitude, effort/reward ratio, sleeping problems and predisposition to hunger had no significant effect on BMI.
Discussion
This study identified a greater association between occupational stress and dietary behavior at work, with an increase in BMI over the term of their employment among paramedics in the province of Quebec in comparison with a control group of general workers. Paramedics experienced a greater increase in BMI over their years of employment than controls, often leading to obesity. The increase in BMI during employment, more prevalent in men, was associated with higher tobacco consumption, high emotional food disinhibition and low supervisor support at work in both groups.
In this study, tobacco consumption was associated with an increase in BMI over time. Both controls and paramedics reported several occupational and psychosocial factors at work, including high psychological demand and effort-reward imbalance, which may be representative of occupational stress [31,32]. Occupational stress may lead to higher tobacco consumption and maladaptive changes in eating behavior, with a preference for sweet and fatty foods or sugary drinks [10,33]. It has been reported that smokers are more likely than non-smokers to report work-related stress [8]. As well, tobacco consumption is a risk factor for abdominal obesity, glucose intolerance and insulin resistance when smokers consume high levels of dietary fat [34]. This may help explain the positive association that was observed between tobacco consumption and BMI and suggest that occupational stress has a negative impact on individual eating behavior.
In this study, 53% of controls and 33% of paramedics showed a low to high degree of emotional food disinhibition. Although the percentage of paramedics with low to high emotional food disinhibition was lower than in the control group, the final model showed a positive association between disinhibited eating and higher BMI in both groups. Emotional distress and disinhibited eating result in an increase in body weight in children, adolescents and adults [35,36]. Emotional food disinhibition reflects a tendency towards overeating, for example in response to a negative stressor [29]. It has been reported that paramedics are exposed to stressful events in the line of duty and elevated cortisol levels have been observed in on-duty compared to off-duty paramedics [37]. High cortisol levels have been claimed to lead to insulin and glucagon dysregulation, which in turn promotes an increase in body weight [38]. In addition, Torres and Nowson [39] reported that chronic stress seems to be associated with a greater preference for sugary and fatty foods. In the case of paramedics, work that involves unpredictable emergency call-outs and variable waiting periods between calls is associated with irregular meal timing [12], which influences satiety and thus the propensity for weight gain [40]. This study revealed a trend towards an influence of meal type (i.e., home-cooked vs. meal from restaurant) on BMI in both groups. Independent, small- and large-chain restaurants have been criticized for contributing to the obesity epidemic by providing meals with excess dietary energy, in other words, more energy than is required for weight maintenance [41,42]. Meal energy data was not collected in this study, limiting the capacity to establish a clear relationship between meal type and weight gain during years of employment. Eating habits at work and their consequences for health should be further investigated. Efforts should be made to improve workers’ ability to make informed choices about their diet by analyzing the dietary energy content provided by restaurant meals vs. homemade meals.
In addition, the results of this study showed an inverse association between BMI and supervisor support at work in both groups. In the control group and among paramedics, over 50% of respondents reported high psychological demand and 34% reported low decision latitude; however, no association was observed between job strain and increases in BMI over time. These results are in accordance with several studies that found no significant associations between job strain and BMI [16]. In their literature review, Brunner et al. [16] found that only 3 out of 13 studies reported an association between job strain and BMI. Also, Karasek and Theorell [31] postulated that active jobs (high psychological demand and high decision latitude) permitted workers to adequately control their work and health. In the same model, Johnson et al. [26] included social support as a moderating dimension enabling workers to alleviate strain. Therefore, workers without adequate supervisor and co-worker support are more likely to develop negative health outcomes [26]. It has been suggested that eating disorders may be related to inadequate social support [43]. Recently, Raspopow et al. [44] showed that inadequate social interactions were associated with emotional eating. Our results showing an association between increased BMI and low supervisor support corroborate this hypothesis.
Finally, there was no association between sleeping problems and increases in BMI. This result is surprising and it is possible that this questionnaire was unsuitable as it evaluated subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, and daytime dysfunction, but not the circadian misalignment that is caused by working the night shift. In this study, both night and day shift workers were included in the same sample, which may have introduced confounds and may partially explain the absence of a positive association between sleeping problems and BMI.
Limitations
The present study has a number of limitations. The questionnaire was self-administered and sent by Internet and therefore the results depend on the respondents’ accuracy and self-awareness. It is also possible that BMI values and tobacco consumption were underestimated [45]. This kind of study is prone to contain volunteer bias. It is possible that unfit or inactive paramedics who exhibit a higher BMI, higher tobacco consumption and occupational stress factors may have refused to participate. A longitudinal study would be a good means of complementing these results.
This study did not identify specific factors related to each occupation that would explain the weight gain over the years of employment. It is possible that the questionnaires used were not sensitive enough to identify pathogenic characteristics specific to each occupation. Further investigations are needed that may require different measures, such as the characteristics of work settings, energy intake/expenditure, physiological biomarkers related to energetic metabolism, and stress/anxiety.
Conclusion
These findings suggest that both work environment and organizational factors influence behavior among paramedics and a control group of other workers. The influences are slightly different since most controls showed higher emotional food disinhibition than the paramedics, while most paramedics reported more occupational and psychosocial stress factors as well as higher tobacco consumption. Whatever the influence of the work environment on the individual may be, attempts to prevent maladaptive eating behavior at work that address both occupational and individual factors are warranted.
Acknowledgements
This study was partly supported by a grant from the Institut de recherche Robert-Sauvé en santé et en sécurité du travail (IRSST) to PC. PP is a senior clinical scientist of the Fonds de recherche du Québec – Santé (FRQS). PB is a Junior 1 Research Scholar of the Fonds de recherche du Québec – Santé (FRQS).
References
- Nevanperä NJ, Hopsu L, Kuosma E, Ukkola O, Uitti J, et al. (2012) Occupational burnout, eating behavior, and weight among working women. See comment in PubMed Commons below Am J Clin Nutr 95: 934-943.
- Champagne N, Abreu M, Nobrega S (2012)Obesity-Overweight and the role of working conditions: a qualitative, participatory investigation. Center for the Promotion for Health in the New England Workplace: Lowell, MA.
- Foss B, Dyrstad SM (2011) Stress in obesity: cause or consequence? See comment in PubMed Commons below Med Hypotheses 77: 7-10.
- Hays NP, Roberts SB (2008) Aspects of eating behaviors "disinhibition" and "restraint" are related to weight gain and BMI in women. See comment in PubMed Commons below Obesity (Silver Spring) 16: 52-58.
- Hays NP, Bathalon GP, McCrory MA, Roubenoff R, Lipman R, et al. (2002) Eating behavior correlates of adult weight gain and obesity in healthy women aged 55-65 y. See comment in PubMed Commons below Am J Clin Nutr 75: 476-483.
- Ishizaki M, Nakagawa H, Morikawa Y, Honda R, Yamada Y, et al. (2008) Influence of job strain on changes in body mass index and waist circumference--6-year longitudinal study. See comment in PubMed Commons below Scand J Work Environ Health 34: 288-296.
- Hellerstedt WL, Jeffery RW (1997) The association of job strain and health behaviours in men and women. See comment in PubMed Commons below Int J Epidemiol 26: 575-583.
- Heikkilä K, Nyberg ST, Fransson EI, Alfredsson L, De Bacquer D, et al. (2012) Job strain and tobacco smoking: an individual-participant data meta-analysis of 166,130 adults in 15 European studies. See comment in PubMed Commons below PLoS One 7: e35463.
- de Assis MA, Nahas MV, Bellisle F, Kupek E (2003) Meals, snacks and food choices in Brazilian shift workers with high energy expenditure. See comment in PubMed Commons below J Hum Nutr Diet 16: 283-289.
- Kouvonen A, Kivimäki M, Virtanen M, Pentti J, Vahtera J (2005) Work stress, smoking status, and smoking intensity: an observational study of 46,190 employees. See comment in PubMed Commons below J Epidemiol Community Health 59: 63-69.
- Rutters F, Nieuwenhuizen AG, Lemmens SG, Born JM, Westerterp-Plantenga MS (2009) Acute stress-related changes in eating in the absence of hunger. See comment in PubMed Commons below Obesity (Silver Spring) 17: 72-77.
- Arial M, Pichonnaz L, Benoît D (2009) Rapport court: Facteurs et stratégies favorisant la préservation de la santé chez les ambulanciers. Institut universtaire romand de Santé au Travail: Lausanne.
- Brunner EJ, Chandola T, Marmot MG (2007) Prospective effect of job strain on general and central obesity in the Whitehall II Study. See comment in PubMed Commons below Am J Epidemiol 165: 828-837.
- Selye H (1978) The Stress of Life. McGraw-Hill: New York.
- Sluiter JK, van der Beek AJ, Frings-Dresen MH (2003) Medical staff in emergency situations: severity of patient status predicts stress hormone reactivity and recovery. See comment in PubMed Commons below Occup Environ Med 60: 373-374.
- Tsismenakis AJ, Christophi CA, Burress JW, Kinney AM, Kim M, et al. (2009) The obesity epidemic and future emergency responders. See comment in PubMed Commons below Obesity (Silver Spring) 17: 1648-1650.
- Betlehem J, Horváth A, Göndöcs Z, Jeges S, Boncz I, et al. (2010) [Major contributing factors of self perceived health in Hungarian ambulance personnel]. See comment in PubMed Commons below Orv Hetil 151: 2089-2098.
- Cydulka RK, Lyons J, Moy A, Shay K, Hammer J, et al. (1989) A follow-up report of occupational stress in urban EMT-paramedics. See comment in PubMed Commons below Ann Emerg Med 18: 1151-1156.
- Jonsson A, Segesten K (2004) Daily stress and concept of self in Swedish ambulance personnel. See comment in PubMed Commons below Prehosp Disaster Med 19: 226-234.
- Alexander DA, Klein S (2001) Ambulance personnel and critical incidents: impact of accident and emergency work on mental health and emotional well-being. See comment in PubMed Commons below Br J Psychiatry 178: 76-81.
- Declercq F, Meganck R, Deheegher J, Van Hoorde H (2011) Frequency of and subjective response to critical incidents in the prediction of PTSD in emergency personnel. See comment in PubMed Commons below J Trauma Stress 24: 133-136.
- Bennett P, Williams Y, Page N, Hood K, Woollard M (2004) Levels of mental health problems among UK emergency ambulance workers. See comment in PubMed Commons below Emerg Med J 21: 235-236.
- Sterud T, Ekeberg Ø, Hem E (2006) Health status in the ambulance services: a systematic review. See comment in PubMed Commons below BMC Health Serv Res 6: 82.
- Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ (1989) The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. See comment in PubMed Commons below Psychiatry Res 28: 193-213.
- Karasek R (1985) Job Content Questionnaire and user’s guide. University of Southern California: Los Angeles.
- Johnson JV, Hall EM, Theorell T (1989) Combined effects of job strain and social isolation on cardiovascular disease morbidity and mortality in a random sample of the Swedish male working population. See comment in PubMed Commons below Scand J Work Environ Health 15: 271-279.
- Siegrist J (1996) Adverse health effects of high-effort/low-reward conditions. See comment in PubMed Commons below J Occup Health Psychol 1: 27-41.
- Stunkard AJ, Messick S (1985) The three-factor eating questionnaire to measure dietary restraint, disinhibition and hunger. See comment in PubMed Commons below J Psychosom Res 29: 71-83.
- Bond MJ, McDowell AJ, Wilkinson JY (2001) The measurement of dietary restraint, disinhibition and hunger: an examination of the factor structure of the Three Factor Eating Questionnaire (TFEQ). See comment in PubMed Commons below Int J Obes Relat Metab Disord 25: 900-906.
- Jennrich RI, Schluchter MD (1986) Unbalanced repeated-measures models with structured covariance matrices. See comment in PubMed Commons below Biometrics 42: 805-820.
- Karasek R, Theorell T (1990) Healthy Work: Stress, Productivity and the Reconstruction of Working Life, (1st edn). Basic Books: New York.
- Siegrist J (2012) Effort-reward imbalance at work – theory, measurement and evidence. Düsseldorf University, Germany.
- Oliver G, Wardle J, Gibson EL (2000) Stress and food choice: a laboratory study. See comment in PubMed Commons below Psychosom Med 62: 853-865.
- Chen H, Hansen MJ, Jones JE, Vlahos R, Anderson GP, et al. (2007) Detrimental metabolic effects of combining long-term cigarette smoke exposure and high-fat diet in mice. See comment in PubMed Commons below Am J Physiol Endocrinol Metab 293: E1564-1571.
- Bryant EJ, King NA, Blundell JE (2008) Disinhibition: its effects on appetite and weight regulation. See comment in PubMed Commons below Obes Rev 9: 409-419.
- Chaput JP, Tremblay A (2007) Acute effects of knowledge-based work on feeding behavior and energy intake. See comment in PubMed Commons below Physiol Behav 90: 66-72.
- Backé E, Kaul G, Klubmann A (2009) Assessment of salivary cortisol as stress marker in ambulance service personnel: comparison between shifts working on mobile intensive care unit and patient transport ambulance. Int Arch Occup Environ Health82: 1057–1064.
- Laugero KD, Falcon LM, Tucker KL (2011) Relationship between perceived stress and dietary and activity patterns in older adults participating in the Boston Puerto Rican Health Study. Appetite 56: 194–204.
- Torres SJ, Nowson CA (2007) Relationship between stress, eating behavior, and obesity. See comment in PubMed Commons below Nutrition 23: 887-894.
- Jakubowicz D, Froy O, Wainstein J, Boaz M (2012) Meal timing and composition influence ghrelin levels, appetite scores and weight loss maintenance in overweight and obese adults. See comment in PubMed Commons below Steroids 77: 323-331.
- Dumanovsky T1, Nonas CA, Huang CY, Silver LD, Bassett MT (2009) What people buy from fast-food restaurants: caloric content and menu item selection, New York City 2007. See comment in PubMed Commons below Obesity (Silver Spring) 17: 1369-1374.
- Urban LE, Lichtenstein AH, Gary CE, Fierstein JL, Equi A, et al. (2013) The energy content of restaurant foods without stated calorie information. See comment in PubMed Commons below JAMA Intern Med 173: 1292-1299.
- Wonderlich-Tierney AL, Vander Wal JS (2010) The effects of social support and coping on the relationship between social anxiety and eating disorders. See comment in PubMed Commons below Eat Behav 11: 85-91.
- Raspopow K, Matheson K, Abizaid A, Anisman H (2013) Unsupportive social interactions influence emotional eating behaviors. The role of coping styles as mediators. See comment in PubMed Commons below Appetite 62: 143-149.
- Shields M, Connor Gorber S, Janssen I, Tremblay MS (2011) Bias in self-reported estimates of obesity in Canadian health surveys: an update on correction equations for adults. See comment in PubMed Commons below Health Rep 22: 35-45.
Relevant Topics
- Child Health Education
- Construction Safety
- Dental Health Education
- Holistic Health Education
- Industrial Hygiene
- Nursing Health Education
- Occupational and Environmental Medicine
- Occupational Dermatitis
- Occupational Disorders
- Occupational Exposures
- Occupational Medicine
- Occupational Physical Therapy
- Occupational Rehabilitation
- Occupational Standards
- Occupational Therapist Practice
- Occupational Therapy
- Occupational Therapy Devices & Market Analysis
- Occupational Toxicology
- Oral Health Education
- Paediatric Occupational Therapy
- Perinatal Mental Health
- Pleural Mesothelioma
- Recreation Therapy
- Sensory Integration Therapy
- Workplace Safety & Stress
- Workplace Safety Culture
Recommended Journals
Article Tools
Article Usage
- Total views: 17228
- [From(publication date):
October-2014 - Apr 04, 2025] - Breakdown by view type
- HTML page views : 12524
- PDF downloads : 4704