Research Article Open Access
Women Promiscuity and Reproductive Health Matters: Findings and Policy Implications
Paul Andrew Bourne1*, Charlene Sharpe-Pryce2, Cynthia Francis3, Angela Hudson-Davis4, Ikhalfani Solan5, Dadria Lewis2, Olive Watson-Coleman6, Jodi-Ann Blake1
1Socio-Medical Research Institute, Jamaica
2Northern Caribbean University, Mandeville, Jamaica
3University of Technology, Jamaica
5South Carolina State University, USA
6Southern Connecticut State University, USA
Visit for more related articles at International Journal of Emergency Mental Health and Human Resilience
Abstract
Background: For millennia, women with multiple sexual partners have been labeled and stigmatized as whores, prostitutes, promiscuous and commercial sex workers. However, there is little literature comprehensively addressing factors related to reproductive health in this group. Aim: The aim of the current study is to elucidate the reproductive health matters of women who have multiple sexual partners. Setting and design: The data use for this research is taken from the Jamaica Reproductive Health Survey, 2007. Stratified random sampling is used to design the sampling frame. Materials and Methods: The current study extracts a sample of 225 respondents (from 7,168 women ages 15-49 years) who indicate having had multiple sex partners. Statistical analysis used: Data are analyzed using the Statistical Packages for the Social Sciences for Windows, Version 21.0. Multiple logistic regressions were used to analyze factors that explained current method of contraception. Results: Women with multiple sex partners on average are involved with men at least 9.5 years their senior, and 72% of them have become pregnant. Currently, contraception use can be explained by social class (middle class, Odds ratio (OR) = 0.08, 95% CI= 0.01 – 0.59); age at first sexual intercourse (OR = 0.90, 95% CI = 0.68 – 1.21); employment status (employed, OR = 5.07, 95% CI = 1.06 – 24.36); and marital status (married or common-law, OR = 0.09, 95% CI = 0.02 – 0.38). Conclusion: The early sexual initiation among young women is a public health problem because of the increased incidence of teenage pregnancy and increased incidence of sexually transmitted diseases, which must be addressed with the same intensity and resource allocation used to fight against Human Immunodeficiency Virus / Acquired Immunodeficiency Syndrome (HIV/AIDS)
Keywords
Women with multiple sex partners, reproductive health matters, contraceptive methods, Jamaica
Introduction
It is well documented in the literature that sexualpromiscuity, low condom usage and early sexual initiation have accounted for an increase in HIV/AIDS, teenage pregnancies and abortions in the developing world (Norman, 2003; Hernandez-Giron et al., 1999; Kaestle et al., 2005; Andersson-Ellstrom et al., 1996). The reality is promiscuous sexual behaviour and infrequent use of condoms (Coker et al., 1994; George et al., 2007) are highly likely to result in sexually transmitted infections, in particular HIV/AIDS and the human papillomavirus (HPV) (Davis et al., 1999; Bain, 2005) as well as the increased risk of cervical cancer (Cooper, Hoffman, Carrara et al., 2007). Using statistics for Jamaica, Bain (Bain, 2005) stated that the prevalence rate of sexually transmitted infections (STIs) among Jamaicans was greater for sex workers than for the population, 6% and 10-20% respectively. Cooper, Hoffman, Carrara et al. (Cooper, Hoffman, Carrara et al., 2007) found that womenwho have multiple sexual partners (≥ 4) were 2 times more likely to have cervical cancers; women who have 2 sexual partners were 1.1 times more likely to have cervical cancers and women who reported having 3 sexual partners were 1.4 times more likely to have cervical cancers compared to women who reported having one sexual partner. There is no doubt, that sexual relationships are a public health matter and that elaborate health intervention programs cannot be developed and implemented without first addressing the reproductive health concerns of women with multiple sexual relationships and risky behavioral practices (Duncan et al., 2010; Kishore & Joshi, 2001).
There are studies that have examined the behavior of commercial sex workers (Duncan et al., 2010; Kishore & Joshi, 2001; Elmore- Meegan et al., 2004) to determine their health status, health-care seeking behaviour and reproductive health matters of those with multiple sex partners. In 2007-2008, using a sample of 2,848 randomly selected Jamaicans aged 15-74 years, Wilks and colleagues (Wilks, Younger, Tulloch-Reid et al., 2008) discovered that 24.4% had at least 2 sexual partners (women, 8.4%; men, 41.0%) in the study period. It should be noted here that the number of Jamaicans using a condom in their last sexual relation was about 53.1%, indicating the higher level of risk among this population. Furthermore, in 2008 Wilks et al. (Wilks, Younger, Tulloch-Reid et al., 2008) found that only 43.1% of Jamaicans used a condom with their main partner in the last sexual relation, which is a decline of 35.2% since 2000 (in 2000, 78.3%). This further demonstrates the increase in risky behaviour among those that are sexually active. The sexual behaviour of some Jamaicans can also be captured in the prevalence of sexually transmitted infections (STIs) between the sexes. Wilks and colleagues found that over the last twelve months, women reported having had a STI 2.6 times more than their male counterparts, which highlights the exposure rate of this group. This observation was not related to commercial sex workers, but ordinary citizens. The sexual exposure to STIs must be taken within the context of the rise in sexual promiscuityamong Jamaicans, as Wilks et al. (Wilks, Younger, Tulloch-Reid et al., 2008) noted that 24.4% of Jamaicans indicated having at least two sexual partners in 2008, which is a 2% increase over 2000. Sexual promiscuity is not limited to Jamaica as studies have established the practice in other developing nations (Elmore-Meegan, Conroy, & Agala, 2004).
Using statistics from the ReproductiveHealth Survey for 2002 it found that 2.2% of Jamaican women aged 15-49 years were involved in the commercial sex trade (National Family Planning Board, 2005), suggesting that promiscuity is higher than the sex trade. Studies which have examined commercial sex workers have researched reproductive health matters, in particular condom usage, STIs, HIV/AIDS, unwanted pregnancies (Duncan et al., 2005; Elmore-Meegan, 2004; Jayasree, 2004), and violenceagainst these individuals (Elmore-Meegan, 2004; Jayasree, 2004]. Wilks et al. (Wilks, Younger, Tulloch-Reid et al., 2008) found that more Jamaican women of ages 15-24 years had multiple sexual partners (15.2%) compared to women ages 25-34 years (11.1%); 35-44 years (6.6%); 45-54 years (2.6%); 55-64 years (1.0%) and 65-74 years (0.2%) and that 41% of young women (ages 15-24 years) were reporting having sex once per week, whereas only 25% indicated that they never had sexual relations. The literature showed that studies on women with multiple sexual partners are limited in scope and primarily focus on age; gender; risk factors; frequency of sexual intercourse; factors associated with the odds of having multiple sexual partners; the rationale for multiple sexual partners, and the increased risk of contracting human papillomavirus (HPV) (Wilks et al., 2008; Yan et al., 2009; Shelton, 2009; Van Doornum et al., 1994; Santelli et al., 1998). Like the sexual promiscuity that occurs in India (Jayasree, 2004) and China (Yan, Chen, Wu et al., 2009), Jamaica is showing signs of increased sexual promiscuity at a much younger age of first sexual initiation and infrequent use of reliable protection, among those that are sexually promiscuous, to prevent STIs.
The empirical evidence on women with multiple sexual partners is omitted in the literature, of which this research aims to fill this gap. This research aims to add to our understanding of reproductive health in women who have numerous sexual partners, as this is not well covered in the current literature. The following three questions will guide the research and analyses: What are the reproductive health matters of women who have multiple sexual partners? What is the prevalence of those who were sexually assaulted? And what are factors that explain current contraceptive usage among this population? The goal of this study is to obtain empirical findings that will be used to guide policy formulationand effective intervention programs.
Materials and Methods
Sample Design
The current study uses a sample of 225 respondents who indicate having had multiple sex partners from an initial survey sample of 7,168 women ages 15-49 years old. The only entry criterion for this study is having two or more sexual partners. A woman whose first husband dies and she re-marries would have had 2 sexual partners; but this is not considered as having more than one partner. Hence, sexual promiscuity is simultaneously having more than one sexual partner. We used data from the JamaicaReproductive Health Survey, 2007 which is a survey conducted by the National Family Planning Board (NFPB) of Jamaica. Since 1997, the NFPB has been collecting information on women (ages 15-49 years) in Jamaica regarding contraception usage and/or other reproductive health matters. The Jamaica Reproductive Health Survey is a national stratified probability cross-sectional survey which is conducted to provide policy makers with pertinent information on reproductive health matters among women in the reproductive years of 15 to 49 years.
The Statistical Institute of Jamaica (STATIN) provided the interviewers and supervisors for the survey. The interviewers administered a thirty-five (35) page questionnaire to the research participants. The participants gave verbal consent to the interviewers before they completed the instrument, and an Institutional Review Board approved the study’s proposal. Stratified random sample was used to draw a sample which reflected the population of Jamaica. Firstly, Jamaica was sub-divided in fourteen sample units, with each representing a parish. Within each parish, communities were divided into enumeration districts (EDs) with each ED comprised of 100 households. Each ED is a geographic region that borders another and this categorization was done to all communities in each parish. The final sample was selected based on a fraction of the EDs in each parish, which then finally constitute Jamaicans. The data are weighted in order to represent the population of women ages 15 to 49 years in the nation (National Family Planning Board, 2002). A detailed account of the sample design is present in the Reproductive Health Survey of Jamaica (National Family Planning Board, 2002). A detailed description of the sampling design has previously been published and can be examined by readers seeking additional information (Bourne & Charles, 2010).
Statistical Tools
The Statistical Packages for the Social Sciences (SPSS) for Windows, Version 21.0 (SPSS Inc; Chicago, IL, USA) was used for this study. Frequencies and means are computed on the basis of sociodemographic characteristics, and other variables. We also performed Pearson’s chi-squared (χ2) tests to compare associations in non-metric variables and Pearson’s Product Moment Correlation for metric variables. Multiple logistic regressions were used to analyze factors that explained current method of contraception. Where collinearity existed (r>0.7), variables were entered independently into the model to determine those that should be retained during the final model construction. To derive accurate tests of statistical significance, the SUDAAN statistical software (Research Triangle Institute (RTI), Research Triangle Park (RTP)) was used to adjust for the survey’s complex sampling design. The rationale behind the chosen method is solely based on the data. Multiple logistic regressions were selected primarily because the dependent variable is a binary one and the researchers wanted to establish likely factors that influence this variable.
Operational Definitions
Data for contraceptive method comes from the question “Are you and your partner currently using a method of contraception? …”, and if the answer is yes “Which method of contraception do you use?” Age at which the person began using contraception was taken from “How old were you when you first used contraception? Currently having sex was measured by the question “Have you had sexual intercourse in the last 30 days?” Education was measured by the question “How many years did you attend school?” Coitarche was measured by “At what age did you have your first intercourse?” Gynaecological examination was taken from “Have you ever had a gynaecological examination?”
Employing logistic regression analysis, this study will examine factors associated with the method of contraception use among women with multiple sexual partners in Jamaica. Grossman’s model (Grossman, 1972) has established the use of econometric analysis to determine the use of health demand. Grossman’s model is forwarded below, where health status is a function of particular determinants and these are given as:
Ht = ƒ (Ht-1, Go, Bt, MCt, ED) (1)
Where Ht-– current health in time period t, stock of health (Ht-1) in previous period, Bt – smoking and excessive drinking, and good personal health behaviours (including exercise – Go), MCt,- use of medical care, education of each family member (ED), and all sources of household income (including current income).
Grossman’s model has been modified and used by many scholars to examine health, health outcome and other health-related issues. Contraceptive usage is a health matter, which means that Grossman’s theoretical framework can be modified and employed thereby. In this case the dependent variable is a dichotomous one (currently using a contraceptive method or not), which means that logistic regression can be applied to examine the factors that influence the dichotomous dependent variable. For this study, four factors determine contraceptive usage among women with multiple sexual partners:
C = ƒ(MS, A, E, S) (2)
Where MS denotes marital status, A means age at first sexual encounter, E represents employment status and S indicates social class
Results
Almost 33% of the study population was 15-24 years of age, compared to 16.4% ages 25-29 years, 20.9% ages 30-34 years, 14.2% ages 35-39 years, 10.7% aged 40-44 years and 4.9% aged 45-49 years.
The socio-demographic characteristics of the study population are presented in Table 1. On average women’ first sexual encounter was with men at least 9.5 years their senior. Almost 29% of the respondents indicated that they had been sexually assaulted during their lifetime, while 51% of those who were sexually assaulted indicated that they were sexually assaulted on their first sexual encounter.
| Characteristic | n | % |
|---|---|---|
| Religiosity | ||
| At least once a week | 56 | 24.9 |
| At least once a month | 49 | 21.8 |
| Less than once a month | 30 | 13.3 |
| Only on special occasions (weddings, funerals, christening) | 62 | 27.6 |
| Does not attend at all | 25 | 11.1 |
| No response | 3 | 1.3 |
| Marital status | ||
| Legally married | 18 | 8.0 |
| Common-law | 44 | 19.6 |
| Visiting | 107 | 47.5 |
| Divorced, separated, widowed | 44 | 19.6 |
| Single | 12 | 5.3 |
| Ever been forced to have sex | ||
| Yes | 65 | 29.1 |
| No | 157 | 70.4 |
| Not sure | 1 | 0.5 |
| Currently having sex (in the last 30 days) | ||
| Yes | 120 | 53.6 |
| No | 104 | 46.4 |
| Currently using a method of contraception | ||
| Yes | 175 | 77.8 |
| No | 50 | 22.2 |
| Employment status | ||
| Unemployed | 143 | 63.6 |
| Employed | 82 | 36.4 |
| Are of residence | ||
| Urban | 34 | 15.1 |
| Semi-urban | 65 | 28.9 |
| Rural | 126 | 56.0 |
| Socioeconomic class | ||
| Lower | 56 | 24.9 |
| Middle | 95 | 42.2 |
| Upper | 74 | 32.9 |
| Years of schooling mean (SD) | 13.5 years (8.3 years) | |
| Age mean (SD) | 29.6 years (8.7 years) | |
| Coitarchemean (SD) | 16.0 years (2.7 years) | |
| Age of person had first sexual intercourse with mean (SD) | 25.7 years (19 years) | |
Table 1. Sociodemographic Characteristic of Sample, n = 225
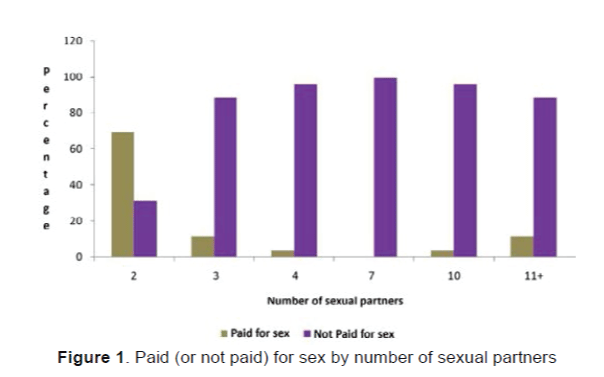
A significant statistical association existed between the number of sexual partners and commercial sexual encounter (χ2=39.4, P<0.0001, Figure 1). Figure 1 show that 69.2% of women with 2 sexual partners were paid for the sexual encounter compared to 11.5% of those with 3 sexual partners, 3.8% of those with 4 sexual partners, and 11.5% of those with 11+ sexual partners.
Half of the commercial sex workers indicated that they had been sexually assaulted, and 19.2% stated they were sexually assaulted on their first sexual encounter. Of those who had indicated being commercial sex workers, 32% had intercourse 2-5 times (per week), 16% between 6-10 times, and 52% at least 11 times per week. When the commercial sex workers were asked when they began this activity, 31% indicated during high school (i.e., post-secondary level including preliminary University and college), 46% reported after leaving high school and 23% noted both.
Of the 54% of the respondents who indicated being currently sexually active (i.e., in the last 30 days), 8.5% reside in urban zones, 25.8% in semi-urban areas, and 65.8% were from rural areas (χ2=13.09, P=0.001). Furthermore, 48.3% of the currently sexually active women indicated that a condom was used during the last contact (χ2 = 34.76, P < 0.0001).
Table 2 presents information on the number of sexual partners, condom usage and frequency of condom usage with steady and casual partners. Fifty-seven (57%) percent of the study population did not state the number of sexual partners, and condom usage was relatively inconsistent.
| Characteristic | n | % |
|---|---|---|
| Number of sexual partners | ||
| 2 | 84 | 37.3 |
| 3 | 5 | 2.2 |
| 4 | 3 | 1.4 |
| 7 | 3 | 1.4 |
| 8+ | 1 | 0.4 |
| Unstated | 129 | 57.3 |
| Currently using a condom | ||
| Yes | 148 | 65.8 |
| No | 77 | 34.2 |
| Frequency of condom usage with steady partner | ||
| Always | 60 | 44.1 |
| Most times | 66 | 48.5 |
| Seldom | 8 | 5.9 |
| Never | 2 | 1.5 |
| Frequency of condom usage with casual partner | ||
| Always | 44 | 54.3 |
| Most times | 30 | 37.0 |
| Seldom | 1 | 1.3 |
| Never | 6 | 7.4 |
Table 2. Number of Sexual Partners, Condom Usage and Frequency of Condom Usage by Study Population, n = 225
There was no significant statistical association between age cohort of study population and those who reported being forced (or not forced) to have sexual intercourse (χ2=16.3, P<0.177). However, information can be provided on those who indicated being sexually assaulted by age cohort: 15-19 years, 12.1%; 20-24 years, 27.3%; 25-29 years, 12.1%; 30-34 years, 12.1%; 35-39 years, 21.2%; 40-44 years, 12.1%; and 44-49 years, 3.0%.
Almost 17% of the sample shared sanitary conveniences (i.e., bathroom and toilet), with 11.6% reported having a pelvic or urinary tract infection, 23.4% had done a Pap smear.
Table 3 presents information on age of respondent, years of schooling, age of menarche, coitarche, age when the person began using contraception and age of person with whom they had their first sexual intercourse. A positive statistical correlation existed between age of respondent and age of person with whom the individual had their first sexual intercourse (r=0.28, P=0.015), as illustrated in Table 3.
| Characteristics | Age | Years of schooling | Age of menarche | Age at first intercourse | Age began using contraception | Age of whom you had sexual intercourse |
|---|---|---|---|---|---|---|
| Age of respondent | 1 | |||||
| Years of schooling | -.097 | 1 | ||||
| 0.147 | ||||||
| Age of menarche | -0.052 | -0.009 | 1 | |||
| 0.441 | 0.898 | |||||
| Age at coitarche | 0.169(*) | 0.291(**) | 0.056 | 1 | ||
| 0.023 | <0.0001 | 0.450 | ||||
| Age began using contraception | 0.500(**) | 0.033 | 0.017 | 0.563(**) | 1 | |
| <0.0001 | 0.643 | 0.814 | <0.0001 | |||
| Age of whom you had sexual intercourse | 0.282(*) | -0.111 | -0.039 | -0.031 | 0.029 | 1 |
| 0.015 | 0.345 | 0.741 | 0.798 | 0.813 | ||
| 74 |
* Correlation is significant at the 0.05 level (2-tailed).
** Correlation is significant at the 0.01 level (2-tailed).
Table 3. Age of Respondent, Years of Schooling, Age of Menarche, Age of Coitarche, Age Began Using Contraception and Age of Person Whom You Had First Sexual Intercourse with
Multivariate Analyses
Table 4 presents information on possible factors, which account for the use of a contraceptive method. Using logistic regression analyses, four variables emerged as statistically significant factors of method of contraception. The model had statistically significant predictive power (model Chi-square (17))=30.79, P<0.021); Hosmer and Leme show goodness of fit test, χ2=4.01, P=0.80), correctly classified 97.3% of the sample. Method of contraception can be accounted for by social class (middle class, Odds ratio (OR)=0.08, 95% CI=0.01–0.59); age at first sexual intercourse (OR=0.90, 95% CI=0.68–1.21); employment status (employed, OR= 5.07, 95% CI=1.06–24.36); and marital status (married or common-law, OR=0.09, 95% CI= 0.02–0.38).
| Variable | β Coefficient | Std Error | Wald statistic | Odds ratio | 95% CI |
|---|---|---|---|---|---|
| Forced into sexual encounter (1=yes) | -1.18 | 0.73 | 2.58 | 0.31 | 0.07 - 1.30 |
| Semi-urban | -1.38 | 1.50 | 0.85 | 0.25 | 0.01 - 4.74 |
| Rural | -1.86 | 1.47 | 1.60 | 0.16 | 0.01 - 2.78 |
| Urban (reference group) | 1.00 | ||||
| Lower class | -1.13 | 1.18 | 0.90 | 0.32 | 0.03 - 3.30 |
| Middle class | -2.56 | 1.04 | 6.14 | 0.08* | 0.01 - 0.59 |
| Upper class (reference group) | 1.00 | ||||
| Pelvic or urinary tract infection | 0.56 | 0.92 | 0.36 | 1.74 | 0.29 - 10.62 |
| Age at first sexual encounter | -0.10 | 0.15 | 0.45 | 0.90* | 0.68 - 1.21 |
| Shared sanitary convenience (1=yes) | 0.58 | 0.89 | 0.43 | 1.79 | 0.32 - 10.15 |
| Frequent church attendance (1=at least one per week) | 2.10 | 1.19 | 3.13 | 8.16 | 0.80 - 83.42 |
| Employed (1=yes) | 1.62 | 0.80 | 4.12 | 5.07* | 1.06 - 24.36 |
| Age of respondents | -0.07 | 0.05 | 1.51 | 0.94 | 0.85 - 1.04 |
| Years of schooling | -0.04 | 0.11 | 0.11 | 0.96 | 0.78 - 1.20 |
| Age at menarche | 0.02 | 0.07 | 0.10 | 1.02 | 0.89 - 1.17 |
| Age began using contraceptive method | 0.07 | 0.12 | 0.33 | 1.07 | 0.85 - 1.35 |
| Crowding | 1.25 | 0.79 | 2.53 | 3.50 | 0.75 - 16.35 |
| Pap Smear (1=yes) | -0.85 | 0.70 | 1.45 | 0.43 | 0.11 - 1.70 |
| Married or common-law union (1=yes) | -2.44 | 0.75 | 10.52 | 0.09** | 0.02 - 0.38 |
1Model chi-square (17) = 30.79, P < 0.021
-2 Log likelihood = 82.93
Nagelkerke r-squared = 0.342
Hosmer and Lemeshow test, χ2 = 4.61, P = 0.80
Overall correct classification = 88.5%
Correct classification of cases of condom usage at first sexual intercourse = 97.3%
Correct classification of cases of not using condom at first sexual intercourse = 16.7%
*P < 0.05, **P < 0.01, ***P < 0.001
Table 4. Logistic Regression Analyses: Variables of Currently Using a Method of Contraception
Discussion
Young women in Jamaica, as well as other developing nations, like China, are engaged in risky sexual behaviour that puts them at risk of contracting a STIs, cervical cancers and pregnancies. Simply put, risky sexual behaviour is directly linked to reduced health status, STIs, and cervical cancers, which make sexual practices among these women a public health matter. This study is on reproductive health practices of women with multiple sexual partners and we found that 65.8% of them currently used a condom; 44.1% consistently used a condom with their steady sexual partner; 54.3% consistently used a condom with their casual sexual partner, and the mean age of coitarche was 16.0 years ± 2.7 years. There were clear dissimilarities between the survey of female undergraduate students in China and the study population. Inconsistent condom usage among female undergraduate Chinese students with multiple sexual partners was 38.6% compared to 56% in this study among women with steady partners and 46% among those with casual partners (Yan, Chen, Wu et al., 2009). Emerging from both studies is the risky sexual behaviour of young women in Jamaica and China.
Using Wilks et al.’s work, we computed that the prevalence rate of STIs among men with multiple sexual partners (≥ 2) was 10.2% compared to 8.0% for those with one sexual partner (Wilks, Younger, Tulloch-Reid et al., 2008). Comparatively, the prevalence rate for women with multiple sexual partners (≥ 2) 7.0% and 4.4% for those with one sexual partner (Wilks, Younger, Tulloch-Reid et al., 2008). A study by Eversley and Newstetter (Eversley & Newstetter, 1989) found that “…women who are exposed to multiple partners do have a significantly higher chance of encountering a male in a high risk category, which results in more serious health concern on a broader scale.” Within the context of Eversley and Newstetter and those which emerged in this research; 72 out of every 100 women have been pregnant; 54 out of every 100 were ‘currently having sexual intercourse’; 78 out of every 100 presently use contraception; 66 out of every 100 use a condom the last time they had sexual relations; 44 out of every 100 frequently used a condom with their steady partner, and 54 out of every 100 frequently utilized a condom with a casual sexual partner. In Wilks and colleagues study (Wilks, Younger, Tulloch-Reid et al., 2008), they found an increase in sexual activities among Jamaicans 15-24 years. They also found an increase in sexual transmitted infections (STIs) among those with multiple sexual partners, indicating the increasing risk factors associated with sexual promiscuity.
Within the context of this study, that found an inverse association between age at first sexual encounter and method of contraception use. It demonstrates that many adolescent women would be ten (10%) percent less likely to use protection against STIs as this may be rejected by the male partner, their inexperience, and most importantly the economics associated with promiscuity. In this study, men who initiate sexual intercourse with adolescent women were about 10 years older. Although these males are older and more sexually experienced, they also have more material resources compared to the young women. This places the women at a disadvantage of being exposed to various STIs, in particular HIV/AIDS, and the human papillomavirus (HPV) (Norman, 2003; Cooper, Hoffman, Carrara et al., 2007; Van Doornum, Prins, Juffermans et al., 1994). It can be extrapolated from this finding that promiscuity is a feature of the individual’s economic situation, social realities and culture.
The socio-economic challenges faced by many Jamaicans, in particular those who are poor; include how to avoid the temptations of being lured by sexual predators, who offer material resources to alleviate the economic plight of vulnerable individuals. The costs of STIs are enormous, but not limited to the individual, and this extends to the wider society (Santelli & Brener, 1998). Early sexual initiation among young Jamaicans accounts for the number of multiple sexual relationships as the first relation may be an experiment. Although marriage and common-law union indicate some stability in a social union, 28% of those individuals may be actively engaged in multiple sexual relations. This means that the cost of STIs such as HIV/AIDs and HPV is not weighed deeply on the minds of sexually promiscuous women because in this work, inconsistent condom usage is high between couples in sexual relations, particularly among those with steady partners fifty-six (56%) percent. When the aforementioned issues are taken within the context of Wilks and colleagues work; that only 52% of young women (ages 15-24 years old) indicated having used a condom, the incidence of STIs has increased greater among women than men in 2008, and the rate of inconsistent condom usage among those in multiple relationships, especially with a casual partner (46%) as found by this work, multiple sexual relationships is more than an individual matter, it is a national public health matter in Jamaica. Hence, it should come as no surprise that in the Caribbean, of the 7 million births in 2013, 2 million were from young women 14 years and younger (Jamaica, 2013). This indicates that teenage pregnancy is on the rise in the Caribbean region, and means more high school dropout among young females. Cromer and Brown (Cromer & Brown, 1992) found that about 50% of adolescents used a condom, teenage pregnancies are high and consequences of sexual practices are sources of morbidity in the United States, which are similar to the findings in Jamaica. These are the national public health matters which we contend are unfolding in Jamaica as a result of sexual promiscuity.
One of the findings which emerged from this work is the percentage of women who commenced commercial sex work during their secondary schooling. Embedded in this finding is how sexual promiscuity is a gateway to commercial sex work. Based on the findings, 3 in every 10 commercial sex workers in Jamaica admitted that this began during their school years and the average age of first sexual debut is during secondary school (16 years). In fact, the behavior is associated with the social pressure of peer groups in regard to sexual initiation, sex traders recruiting school girls, social decay in the general society, and economic challenges faced by many families. Early sexual initiation, multiple sexual partners and sexual promiscuity are, therefore, by-products of socio-economic ills of the Jamaican society, and commercial sex work is a response to the economic challenges.
Previous studies have established a direct association between education and health status, and other factors and health (Hutchinson, 2004; Bourne, 2009a; Bourne, 2009b; Bourne, 2009c; Bourne, 2009d; Bourne, 2009e; Bourne, 2008a; Bourne, 2008b; Smith & Kington, 1997; Wilkinson & Marmot, 2003). Even though education opens numerous opportunities for the recipient, the economic hardship of women in Jamaica is eroding this reality as many of them become engaged in illegal sex work and multiple sexual relationships in order to provide for themselves and their children. Whether due to illicit drug use or any other factors (Santelli, Brener, & Lowry, 1998), the reality in Jamaica is that 33 out of every 100 women who indicated having multiple sexual partners were between 15 and 24 years, 16 out of every 100 aged 15-19 years, and most of the individuals resided in rural areas, and had post-secondary education. Poverty hampers economic freedom and choice, and so despite one’s willingness to avoid these practices, many realities are circumvented. The poor are held in a vicious cycle of continuous poverty, and on the onset of health conditions poverty could extend to the family. With the reality that the prevalence rate of poverty, since 1990, is at least twice as high in rural as in urban areas, (Planning Institute of Jamaica & Statistical Institute of Jamaica, 1990-2008), the economic difficulty is accounting for rural women having many sexual partners, as this is in keeping with the needed assistance. Still, some of these women, although they receive gifts, money, material items and other articles, by being with men in a sexual relationship, it is not construed as commercial sex work.
In 2007, inflation in Jamaica rose to 16.8% that was the highest in a decade (1998-2007) and the exchange rate of one US dollar was Jamaican $69.06 being the highest in two decades (1989-2007), which translates into high cost of living and by extension increased socio-economic hardship. This time was also the precursor to a threeyear economic recession which was from 2008-2010 and it was 2007 that the data for study was collected by the Family Planning Board. Clearly the middle-to-upper class women were adversely affected by the high cost of living and economic hardship more than poor women. The rationale for the previously mentioned perspective is enveloped in the sexual practices of women in the various social classes. Wilks et al.’s work that a conducted in 2007 revealed that 20.7% of poor Jamaican women ages 15-74 years had multiple sexual partners (2+ partners) compared to 26.2% of those in the middle class and 26.7% in the upper class.
Economic deprivation is, therefore, creating sexual promiscuity as can be demonstrated by the current findings. This research found that employed women with multiple sexual partners were 5.1 times more likely to use a method of contraception than unemployed women and that 16 in every 25 women who have many sexual partners were unemployed. These unemployed women are mostly educated at the post-secondary level in the middle-to-upper class who are in need of employment opportunities. It is a desire for socio-economic opportunities that is driving sexual promiscuity among educated-middle to upper class women and this account for their willing to have multiple relationships with economically stable men. Thus, unemployed women give men vetoing power over reproductive health, because they do not want the men to withdraw the needed financial and other forms of support. We can deduce from Wilks et al.’s study that there is vetoing power of expressed in sexual practices of women as 44.2% of Jamaican women ages 15-74 years used a condom compared to 35.1% of unemployed women. Embedded in economics of sexuality as well as sexual practice is the psychological state of unemployed women and how they surrender to the demands of the male because of the economics of survivability. The male, on the other hand, is able to play a psychological game with the female because of the economics of survivability, through which he is able to lure the female to acquiesce his demands.
Statistics showed that unemployment among women is greater than that for men (Planning Institute of Jamaica, 1991-2009), and with the context that poverty is greater for the former group than the latter and among rural residents (Planning Institute of Jamaica & Statistical Institute of Jamaica, 1990-2008), a part of the survivability strategy of women is to rely on men for financial support. It should not be surprising that poverty, which along with unemployment is higher in rural Jamaica, results in some residents engaging in more risky behaviour. Furthermore, men who have economic power, are more likely to be employed and receive greater emoluments, are still able to wield this power, even over their spouses. In this survey, married women or women in common-law unions were 91% less likely to use a method of contraception which means decisions on contraceptive usage is a male economic issue. This is the opportunity cost of his economic provision for the household.
Previous studies have established that there is a statistical association between poverty and illness (Wagstaff, 2001; Marmot, 2002; Pan American Health Organization, 2001a; Pan American Health Organization, 2001b; Alleyne, 2001; Van Agt, Stronks, & Mackenbach, 2000). Poverty does not only have an impact on illness, it causes pre-mature deaths, lower quality of life, lower life (and unhealthy life) expectancy, low development, high rates of pregnancy and social degradation of the community (World Health Organization, 2005), including the commercial sex trade. The World Health Organization (WHO) (World Health Organization, 2005) opined that 80% of chronic illnesses were in low and middle income countries, suggesting that illness interfaces with poverty and other socio-economic challenges. The WHO captures this aptly by noting the following “...People who are already poor are the most likely to suffer financially from chronic diseases, which often deepen poverty and damage long term economic prospects” (World Health Organization, 2005). Another by-product of poverty is multiple partner relationships, as women use these relationships to bridge the unemployment and poverty gap, and material deprivation (Bourne, 2009f). The notion that poverty, material deprivation and unemployment are related to increase multiple sexual relationships is a reality. In 2008, the Jamaican economy was in a significant economic downtown and Wilks et al. (Wilks, Younger, Tulloch- Reid et al., 2008) showed that more women reported having multiple sexual partners (2008, 24.4%), compared to 2000 (22.6%), when the economy grew by a mere (0.2%) percent.
Promiscuity is clearly a product of experimentation among youths and there is an obvious social stigma of this issue in many cultures. Jamaica is a highly sexed culture as Wilks and co-authors found that 3 out of every 4 people had sexual relations at least once per month and 33 out of every 100 women aged 15-74 years had never had sex in the last 12 months, and among women aged 15-24 years only 32 out of every 100 had not have sex in the last year. While poverty is frequently cited as rationale for the commercial sex trade, promiscuity is not a product of inconvenience as emerged from the current work. This work found that 75 out of every 100 female Jamaicans aged 15-49 years were of the middle-to-upper class – including 33 out of every 100 from the wealthy class. The argument of poverty should not be used in a discourse on multiple sexual relations among female Jamaica as the evidence refutes this common sense (or traditional) notion. They also revealed that 8.4% of female Jamaicans aged 15-74 years had at least two sexual relationships compared to 17% among those 15-24 years old. The highly sex culture is having an influence on young people, and older men are initiating sexual relations on young women, particularly those among the middle-to-upper class who are unemployed.
There are mental health issues in Jamaica, which emerged from this study that have never been discussed prior, related to the psychology of multiple sex partners. Studies from Ramrakha et al. (Ramrakha, Paul, Bell et al., 2013) and Searle (Searle, 2009) revealed that substance dependence, depression, low self-esteem, and those with low economic status were more likely to engaged into multiple sexual relationship. The present study is unable to refute the issue of substance dependence among people with multiple sexual partners, but national probability study in 2007 revealed that 64.3% of Jamaicans aged 15-74 years currently consume alcoholic beverages compared to 13.5% used marijuana, 14.5% are current cigarette smokers (Wilks, Younger, Tulloch-Reid et al., 2008). Males aged 15-74 years old were at least two times more like to consume alcoholic beverages, use marijuana and smoke cigarettes compared to females of the same cohorts (Wilks, Younger, Tulloch-Reid et al., 2008). We can therefore deduce and extrapolate using Wilks et al.’s study (Wilks, Younger, Tulloch-Reid et al., 2008) on the current one that women with multiple sexual partners rely on substance such as alcoholic beverages. We surmise that the substance dependence of sexual promiscuous women is an indicator of poor psychological state and this may not go as far as depression as is found by Searle (Searle, 2009), but is equally refuted by Ramrakha et al. (Ramrakha, Paul, Bell et al., 2013).
In contemporary western societies, education is sold as a means of social mobility and success. It follows, therefore, that when education is attained by western women, if they are unemployed, particularly among the middle-to-upper class for long periods, they are likely to internalize their situation as failure and this results in psychological disorders. Clearly, there is a negative mood which is embedded in multiple sexual relationships. Jamaican women who are engaged in multiple sexual relations are mostly unemployed (64%), have at least secondary level education and rural residents which means lower socio-economic resources, and these would translate into negative moods as they are unable to material certain demands because of these constraints. Burleson et al. (Burleson, Trevathan, & Todd, 2007) reiterated the argument of negative moods among sexual promiscuous people, and this offers an explanation of what obtains among this sampled women in Jamaica. The reality among sexual promiscuous women in Jamaica is that they are unable to assist themselves economically and this must be having a negative impact on their psyche, and there the expression of substance use including alcoholic beverages is an indicator of the stressors, mental health issues among the women. Jamaican women are experiencing sexually induced psychological disorders created by the economic environment.
In Jamaica reproductive health matters have not caught onto the inclusion of psychiatric morbidity or mental health matters arising from sexual behaviours induced by the economy. A careful perusal of data collected by the Family Planning Board, which is the agency responsible for the collection of data on reproductive health matters, have not shown a single item on psychiatric morbidity in the sexual practices of women ages 15-49 years old. This study has highlighted the importance of the mental health issues surrounding sexual practices and as such psychiatric morbidity must be included as items on the questionnaire of the Family Planning Board. With the primary agency not caught onto the inclusion of psychiatric morbidity in reproductive health matters, many sub-agencies have followed suit and this explains the shortfall in data collection on the matter.
With no obvious statistical association between psychiatric morbidity and sexual practices of women ages 15-to-49 years, it is difficult to definitely state what obtains in this situation. However, Wilks and colleagues work (Wilks, Younger, Tulloch-Reid et al., 2008) comes as close as possible and we will use this study to deduce and argue a case for the relationship between mental health conditions and sexual practices. In Wilks et al.’s work, 72.3% of women ages 15-74 years indicated that they were experiencing some mental health conditions – feeling down/depressed/hopeless, 40.9%; little interest in pleasure 31.5% compared to 46.3% of men. Our study, on the other hand, showed that many of the women are educated, unemployed and from the middle-to-upper class. Hence, sexual promiscuity could be an expression of their depressive state or their depressive state an indicator of sexual promiscuity. It is highly difficult to categorically and definitively prove which comes first; but the reality is, sexual promiscuity is associated with psychiatric morbidity. In order to understand this obvious linkage between the two aforementioned variables, we will examine some findings from Wilks et al.’s study. Wilks and colleagues (Wilks, Younger, Tulloch-Reid et al., 2008) found that 34.5% of Jamaicans ages 15-74 years who had a ‘heart attack’ was depressed compared to 33.2% of those who had stroke, and 23.4% of those who were diagnosed with cancers. Now, with such a high percentage of Jamaican women indicated that they were depressed in 2007, there is evidence that heart attack is resulting in depression or vice versa, which is also the case for those who had a stroke or diagnosed with cancers. We can extrapolated from Wilks et al.’s work that the relationship between physical conditions and psychological conditions can be extended to sexual behaviour and that the economy can induce sexual promiscuity, which is an indication of psychiatric morbidity experienced by the individual. Hence, does sexual promiscuity increase the risk of psychiatric morbidity or does psychiatric morbidity make women more vulnerable for sexual exploitation by economically privileged men? In this study, we cannot categorically state where psychiatric morbidity as well as economic conditions is causing sexual promiscuity or sexual promiscuity is resulting in psychiatric morbidity and/or economic conditions, such a reality is highly comparable to the chicken and egg situation; but the association between aforementioned variables is real one.
Are the only psychological issues experienced my women with many sexual partners, those expressed above? The issue of sexual promiscuity among women goes deeper than the current expression to the 1) desire for acceptance and 2) cognitive development (Cotterell, 1996). The present study found that for the participants of this study 1) the age of first coitus was 16.0 years; 2) they have secondary level education and 3) they are engaged in non-paid sexual relations, which suggest that involvement into this lifestyle is embedded in the desire for acceptance and cognitive development. Jamaican women who are engaged in promiscuous sexual relations commence their sexual journey at 16 years old, which is in the period of adolescence. During this stage of development, they seek acceptance (Cotterell, 1996) and not have a strong religious belief, they become susceptible to sexual lures of adults. Adults are more likely to lure adolescents using material goods, owing to the economic vulnerability of the persons. This often explains the reason adolescents may not use contraceptive devices (Juarez & LeGrand, 2005; George et al., 2007) because of the dictate of the adults with the economic resources who have vetoing power of person. The vetoing powers of powerful adults allow them to lure vulnerable young women into sexual activities because of the economic vulnerability of the young women, particularly the unemployed ones. Orr et al. found that females who are initiated early in sexual activities are mostly those who have poor self-image (Orr, Wilbrandt, Brack et al., 1989), which is related to the psychological matter of self-esteem. So, we deduce from the current data, within the context of the literature that multiple sexual relationships among Jamaican women could eventually lead to depression this view is also forwarded by DiClemente et al. (DiClemente, Wingood, Crosby et al., 2001).
Many of the women in this study have multiple sexual partners outside of commercial sex. This indicates mental health issues such as frustration, psychological trauma, early neglect, substance use, seeing oneself as a risk taker, and therefore sexual promiscuity is an expression of psychosocial challenges. This has been empirically established by Kowaleski-Jones and Mott (Kowaleski-Jones & Mott, 1998). The fact that many of the sampled women commence coitus at an early age, this can be due to childhood sexual abuse. This state of early mental trauma can be expressed by sexual promiscuity, a retaliatory (or coping) approach by the abused, or long-term distress and justify posttraumatic stress disorder (PTSD) as well as eating disorder (Glasser et al., 2001; Kendall-Tackett et al., 1993; Fritsch & Warrier, 2004; Wonderlich et al., 2001). The mental health issue of sexual promiscuity has not been examined in Jamaica; but Coid et al., (Coid, Petruckevitch, Chung et al., 2003) found that women who were sexually abused in childhood were 5 times more likely to be diagnosed with PTSD in comparison to those who were not sexually abused during childhood. Another study empirically established that Borderline Personality Disorder, along with consequences, are features of sexual abuse in childhood (Yen et al., 2002; Yuan et al., 2006; Fergusson et al., 1996; Fergusson et al., 1997), indicating they there are secret trauma in adulthood following early forced sexual experience in childhood (Gorcey et al., 1986; Russell, 1986; Nagy et al., 1995; Springs et al., 1992) that accounts for sexual promiscuity in among Jamaican women in the reproductive years of 15-49 years.
Conclusion
In summary, risky behaviour among some women in Jamaica is a national issue because of the increased prevalence of STIs, teenage pregnancies, high school drop-outs, increased cervical cancers, psychiatric disorders and the cost to society. The fact that many of these women demand and utilize public health care services, this makes risky sexual behaviour a public health matters of national importance due to the potential increase in medical costs. Sexual promiscuity among Jamaican women has many mental health issues and consequences that must be taken into consideration when seeking to address risky sexual behaviour. Serious efforts are needed to comprehend, alleviate and rectify these practices – education, training on the use of contraception, women empowerment through income generation, arresting sexual abuse during childhood, and financial independence. Women in Jamaica that are involved in promiscuity are unemployed, of the middle-to-upper class, engaged in sexual behaviour as early as in secondary school, infrequently use condoms and those are characteristics of the highly sexed women. The present findings are far reaching, but should not be taken as the totality of the research necessary for understanding this phenomenon, sexual promiscuity. A multilevel approach is needed to address multiple sexual partnerships among women in Jamaica, which should target middle-to-upper class women.
Recommendations
This study should open the door for empirical inquiries on psychiatric morbidity and sexual behaviour among Jamaican women. The appetite of scholars and policy makers should have been increased to the point where research should begin in the area of 1) the economics of sexual promiscuity, 2) cognitive mapping of people’s views on sexual behaviour and psychiatric morbidity, 3) is there a causal link between sexual behaviour and psychiatric conditions, 4) social consequences of sexuality promiscuity on fertility and parenting, 5) psychohistoriographic of women who have multiple sexual partners, 6) psychotherapy for induced sexual expressions following prolonged period of individual economic misfortunes, and 7) the psychopharmacology and sexual promiscuity.
Limitations
This work has one limitation, the use of secondary data to examine a phenomenon. The primary data were not collected for the current purpose. This dataset did not seek to examine psychological issues (substance use disorder and psychiatric disorder) and their influence on sexual expressions and so this is a major limitation for this study; but it can provide insights into the matter despite this limitation.
Conflict of interest
The authors have no conflict of interest to report.
Disclaimer
The researchers would like to note that while this study used secondary data from the Reproductive Health Survey, any of the errors in this paper should be ascribed to the National Family Planning Board, but to the researchers.
References
- Alleyne, G. A. O. (2001). Health and economic growth. In: Pan American Health Organisation. Equity and health: Views from the Pan American Sanitary Bureau, Occasional Publication No. 8. Washington DC, 265-269
- Andersson-Ellstrom, A., Forssman, L., &Milsorn, I. (1996). Age of sexual debut related to life-style and reproductive health factors in a group of Swedish teenage girls. ActaObstetriciaetGynecologicaScandinavica, 75,484-489
- Bain, B. (2005). HIV/AIDS: The rude awakening/stemming the tide. In: Morgan O, eds. Health issues in the Caribbean. Kingston: Ian Randle Publishers, 62-76
- Bourne, P.A. (2008a).Medical Sociology: ModellingWell-being for elderly People in Jamaica. West Indian Medical Journal,57, 596-04
- Bourne, P. A. (2008b). Health Determinants: Using Secondary Data to Model Predictors of Wellbeing of Jamaicans. West Indian Medical Journal, 57, 476-81
- Bourne, P. A. (2009a). An epidemiological transition of health conditions, and health status of the old-old-to-oldest-old in Jamaica: a comparative analysis. North American Journal of Medical Sciences, 1, 211-219
- Bourne, P. A. (2009b). Good Health Status of Older and Oldest Elderly in Jamaica: Are there differences between rural and urban areas? Open Geriatric Medicine Journal,2, 18-27
- Bourne, P.A. (2009c).Social determinants of self-evaluated good health status of rural men in Jamaica.Rural and Remote health, 9, 1280
- Bourne, P. A. (2009f).Impact of poverty, not seeking medical care, unemployment, inflation, self-reported illness, health insurance on mortality in Jamaica.North American Journal of Medical Sciences, 1, 99-109
- Bourne, P.A., & Charles, C.A.D. (2010). Sexual behavior and attitude towards HIV testing among non-HIV testers in a developing nation: A public health concern. North American Journal of Medical Sciences, 2, 419-426.
- Bourne, P.A., &McGrowder, D.A. (2009e).Rural health in Jamaica: Examining and refining the predictive factors of good health status of rural residents. Journal of Rural and Remote Health,9,1116
- Bourne, P.A., &Rhule, J. (2009d). Good Health Status of Rural Women in the Reproductive Ages. International Journal of Collaborative Research on Internal Medicine & Public Health, 1,132-155.
- Burleson, M. H., Trevathan, W. R., &Todd, M. (2007).In the mood for love or vice versa? Exploring the relations among sexual activity, physical affection, affect, and stress in the daily lives of mid-aged women.Archives of Sexual Behavior, 6(3), 357-68
- Case histories from the Drop-in Centre Clinics. (2004). Thiruvananthapuram and Thrissur: Foundation for Integrated Research in Mental Health, 1999-2001. In: Jayasree A. K. Searching for justice for body and self in a coercive environment: Sex work in Kerala, India. Reproductive Health Matters,12, 58-67
- Coid, J., Petruckevitch, A., Chung, W.S., Richardson, J., Moorey, S., &Feder, G. (2003). Abusive experiences and psychiatric morbidity in women primary care attenders. British Journal of Psychiatry, 183,332-339
- Coker, A.L., Richter, D.L., Valois, R.F., et al. (1994).Correlates and consequences of early initiation of sexual intercourse.Journal of School Health, 64, 372-377
- Cooper, D., Hoffman, M., Carrara, H., et al. (2007). Determinants of sexual activity and its relation to cervical cancer risk among South African women. BMC Public Health, 7
- Cotterell, J. (1996). Social Networks and Social Influences in Adolescence, 1st edition. London: Routledge.
- Cromer, B.A., & Brown, R.T. (1992). Update on pregnancy, condom use, and prevalence of selected sexually transmitted diseases in adolescents. Current opinion in obstetrics & gynecology, 4, 855-9.
- Davis, K.R., & Weller, S.C. (1999).The effectiveness of condoms in reducing heterosexual transmission of HIV.Family Planning Perspectives, 31, 272-279
- DiClemente, R. J., Wingood, G. M., Crosby, R. A.,et al. (2001). A prospective study of psychological distress and sexual risk behavior among black adolescent females.Pediatrics,108(5), E85.
- Duncan, J., Gebre, Y., Grant, Y., et al. (2010). HIV prevalence and related behaviors among sex workers in Jamaica. Sexually Transmitted Diseases, 37,306-310
- Elmore-Meegan, M., Conroy, R.M., &Agala, C.B. (2004). Sex workers in Kenya, numbers of clients and associated risks: An exploratory survey. Reproductive Health Matters, 12, 50-57
- Eversley, R.B., &Newstetter, A. (1989).AIDS risk among women with multiple sexual partners: HIV risk screening data from a family planning population. International Conference on AIDS, 5, 750
- Fergusson, D.M., Horwood, L.J., &Lynskey, M.T. (1996). Childhood sexual abuse and psychiatric disorders in young adulthood: Part II: Psychiatric outcomes of sexual abuse. Journal of the American Academy of Child and Adolescent Psychiatry, 35, 1365 - 1374.
- Fergusson, D.M., Horwood, L.J., &Lynskey, M.T. (1997).Childhood sexual abuse, adolescent sexual behaviours and sexual revictimization.Child Abuse and Neglect, 21, 789 - 803
- Fritsch, R.C., &Warrier, R.R. (2004). Commentary on a first-person account of sexual abuse: From experience to theory and treatment. Psychiatry: Interpersonal & Biological Processes, 67, 239-245
- George, C, Alary, M., &Otis J. (2007).Correlates of sexual activity and inconsistent condom use among high-school girls in Dominica.West Indian Med Journal,56(5), 433-438.
- George, C., Alary, M., & Otis, J. (2007).Correlates of sexual activity and inconsistent condom use among high-school girls in Dominica.West Indian Medical Journal, 56, 433-438
- Glasser, M., Kolvin, I., Campbell, D., Glasser, A., Leitch, I., &Farrelly, S. (2001). Cycle of child sexual abuse: Links between being a victim and becoming a perpetrator. British Journal of Psychiatry, 179, 482-494
- Gorcey, M., Santiago, J.M., &McCall-Perez, F. (1986). Psychological consequences for women sexually abused in childhood. Social Psychiatry, 21, 129 - 133
- Grossman, M. (1972).The demand for health - a theoretical and empirical investigation. New York: National Bureau of Economic Research
- Hernandez-Giron, C.A., Cruz-Valdez, A., Quiterio-Trenado, M., et al. (1999). Factors associated with condom use in the male population of Mexico City. International Journal of STD & AIDS, 10, 112-117
- Hutchinson, G., Simeon, D.T., Bain, B.C., Wyatt, G.E., Tucker, M.B., LeFranc, E. (2004).Social and Health determinants of well-being and life satisfaction in Jamaica.International Journal of Social Psychiatry, 50, 43-53
- Jamaica Gleaner.(2013). Increase in teenage pregnancy across the region. Kingston: Jamaica Gleaner
- Jayasree, A.K. (2004). Searching for justice for body and self in a coercive environment: Sex work in Kerala, India.Reproductive Health Matters, 12, 58-67
- Juarez, F., &LeGrand, T.(2005). Factors influencing boys' age at first intercourse and condom use in the Shantytowns of Recife, Brazil.Studies in Family Planning,36(1),57-70
- Kaestle, C.E., Halpern, C.T., Miller, W.C., et al. (2005). Young age at first sexual intercourse and sexually transmitted infections in adolescents and young adults. American Journal of Epidemiology, 161, 774-780
- Kendall-Tackett, K., Williams, L. M., &Finkelhor, D. (1993). Impact of sexual abuse on children: A review and synthesis of recent empirical studies. Psychological Bulletin, 113,164-180
- Kishore, J., & Joshi, T.K. (2001).Health status and health seeking behaviour of male workers in Delhi.Indian Journal of Community Medicine, 26,192-917
- Kowaleski-Jones, L., & Mott, F.L. (1998). Sex, contraception and childbearing among high risk youth: do different factors influence males and females? Family Planning Perspectives,30(4), 163-9
- Marmot, M. (2002). The influence of Income on Health: Views of an Epidemiologist. Does money really matter? Or is it a marker for something else? Health Affairs,21, 31-46
- Nagy, S., DiClemente, R., & Adcock, A.G. (1995). Adverse factors associated with forced sex among southern adolescent girls. Pediatrics,96, 944 - 946
- National Family Planning Board (NFPB). (2005). Reproductive Health Survey 2002. Kingston: NFPB
- Norman, L.R. (2003).Predictors of consistent condom use: A hierarchical analysis of adults from Kenya, Tanzania and Trinidad. International Journal of STD & AIDS, 14, 584-590
- Orr, D.P., Wilbrandt, M.L.,Brack, C.J., et al.(1989). Reported sexual behaviors and self-esteem among young adolescents.American journal of diseases of children, 143(1), 86-90.
- Pan American Health Organization (PAHO). (2001a). Investment in health: Social and economic returns, Scientific and Technical Publication, No. 582. Washington DC: PAHO, WHO
- Pan American Health Organization (PAHO). (2001b). Equity and health: Views from the Pan American Sanitary Bureau, Occasional Publication, No. 8. Washington DC: PAHO, WHO
- Planning Institute of Jamaica (PIOJ), & Statistical Institute of Jamaica (STATIN). (1990-2008). Jamaica Survey of Living Conditions, 1989-2007. Kingston: PIOJ & STATIN
- Planning Institute of Jamaica (PIOJ).(1991-2009). Economic and Social Survey Jamaica, 1990-2008. Kingston: PIOJ
- Ramrakha, S., Paul, C., Bell, M. L., Dickson, N., Moffitt, T. E., &Caspi, A. (2013). The relationship between multiple sex partners and anxiety, depression, and substance dependence disorders: A cohort study. Archives of Sexual Behavior, 42(5), 863-72
- Russell, D.E.H. (1986). The Secret Trauma: Incest in the Lives of Girls and Women. New York: Basic Books
- Santelli, J.S., Brener, N.D., Lowry, R., et al. (1998). Multiple sexual partners among U.S. adolescents and young adults.Family Planning Perspective, 30, 271-275
- Searle, N. (2009). Sexual behavior and its mental health consequences.MSc thesis Swansea University
- Shelton, J.D. (2009). Why multiple sexual partners? Lancet, 374, 367-369
- Smith, J.P., &Kington, R.(1997).Demographic and Economic Correlates of Health in Old Age.Demography, 34, 159-70
- Springs, F.E., & Friedrich, W.N. (1992).Health risk behaviours and medical sequelae of childhood sexual abuse. Mayo Clinic Proceedings, 67, 527 - 532
- Van Agt, H.M.E., Stronks, K., &Mackenbach, J.P. (2000). Chronic illness and poverty in the Netherlands.European Journal of Public Health, 10,197-200
- Van Doornum, G.J., Prins, M., Juffermans, L.H., et al. (1994). Regional distribution and incidence of human papillomavirus infections among heterosexual men and women with multiple sexual partners: A prospective study. Genitourinary medicine, 70, 240-246
- Wagstaff, A. (2001). Poverty, equity, and health: Some research findings. In: Equity and health: Views from Pan American Sanitary Bureau. Pan American Health Organization, Occasional publication No. 8, Washington DC, US, 56-60
- Wilkinson, R. G., & Marmot, M. (2003).Social Determinants of Health. The Solid Facts, 2nd ed. Copenhagen: World Health Organization
- Wilks, R., Younger, N., Tulloch-Reid, M., et al. (2008).Jamaica Health and Lifestyle Survey 2007-2008. Technical Report. Kingston: Epidemiology Research Unit, Tropical Medicine Research Institute, University of the West Indies, Mona, pp. 1-50
- Wonderlich, S.A., Crosby, R.D., Mitchell, J.E., Thompson, K.M., Redlin, J., Demuth, G., et al. (2001). Eating disturbance and sexual trauma in childhood and adulthood.International Journal of Eating Disorders, 30,401-412.
- World Health Organization (WHO).(2005). Preventing Chronic Diseases a vital investment. Geneva: WHO
- Yan, H., Chen, W., Wu, H., et al. (2009). Multiple sex partner behavior in female undergraduate students in China: A multi-campus survey. BMC Public Health, 9, 305
- Yen, S., Shea. T., Battle, C.L., Johnson, D.M, Zlotnick, C., Dolan-Sewell, R., et al. (2002). Traumatic exposure and posttraumatic stress disorder in borderline, schizotypal, avoidant, and obsessive-compulsive disorders: Findings from the Collaborative Longitudinal Personality Disorders Study. The Journal of Nervous and Mental Disease, 190, 510-518
- Yuan, N.P., Koss, M.P., &Stone.M. (2006).The Psychological Consequences of Sexual Trauma. Harrisburg, PA: VAWnet, a project of the National Resource Center on Domestic Violence/Pennsylvania Coalition Against Domestic Violence. Retrieved month/day/year, from: http://www.vawnet.org.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 21727
- [From(publication date):
March-2015 - Apr 03, 2025] - Breakdown by view type
- HTML page views : 17013
- PDF downloads : 4714