Case Report Open Access
When Heart Failure has to do with Past Abdominal Surgery
Julien Plessis1*, Laurianne LE Gloan1, Jean-Pierre Gueffet1, Frédéric Lerat2 and Patrice Guerin1
1Centre Hospitalier Universitaire de Nantes, Institut du Thorax, Service de Cardiologie, France
2Centre Hospitalier Universitaire de Nantes, Service de Radiologie, France
- *Corresponding Author:
- Julien Plessis
Centre Hospitalier Universitaire de Nantes
Institut du Thorax, Service de Cardiologie
CHU de Nantes-Hôpital Nord-Laennec
Bvd Jacques Monod
44093 Nantes Cedex
France
Tel: +33 240165009
Fax: +33 240165197
E-mail: plessis.ju@gmail.com
Received date: April 05, 2016; Accepted date: April 05, 2016; Published date: April 26, 2016
Citation: Plessis J, Gloan LLE, Gueffet JP, Lerat F, Guerin P (2016) When Heart Failure has to do with Past Abdominal Surgery. OMICS J Radiol 5:233. doi:10.4172/2167-7964.1000233
Copyright: © 2016 Plessis J, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Radiology
Abstract
A 70-year-old woman, with a past medical history of permanent atrial fibrillation, cholecystectomy for symptomatic gallstones and obesity (54 kg/m² body mass index), was admitted to the hospital for rapidly increasing dyspnea (NYHA class III). At admission, heart rate was 110 beats per minute (bpm) and blood pressure was 125/73 mmHg. Physical examination revealed clinical signs of right heart failure including major peripheral oedema, hepatomegaly, bilateral pleural effusion, and ascites with no signs of portal hypertension or hepatocellular insufficiency.
Keywords
Heart failure; High cardiac output; Porto systemic shunt; Pulmonary hypertension
Case Report
A 70-year-old woman, with a past medical history of permanent atrial fibrillation, cholecystectomy for symptomatic gallstones and obesity (54 kg/m2 body mass index), was admitted to the hospital for rapidly increasing dyspnea (NYHA class III). At admission, heart rate was 110 beats per minute (bpm) and blood pressure was 125/73 mmHg. Physical examination revealed clinical signs of right heart failure including major peripheral oedema, hepatomegaly, bilateral pleural effusion, and ascites with no signs of portal hypertension or hepatocellular insufficiency.
On the first transthoracic echocardiogram, preserved left ventricular ejection fraction with normal diastolic function was noticed. Interestingly, a major dilatation of the right ventricle, the right atrium, and the inferior vena cava (45 mm) were observed. Systolic pulmonary artery pressures were estimated as high as 60 mmHg with the tricuspid regurgitation, and cardiac index was increased, reaching 4.8 L/min/m2. Pulmonary assessment on the six-minute walk test was satisfying at 255 meters, and a small restrictive impairment was documented on a pulmonary function test (assigned to obesity). Finally, no perfusion defect was found on the ventilation/perfusion lung scan.
After a rapid but major relief of congestive symptoms using high doses of diuretics, our patient lost about 50 kg of weight. Then, she underwent a right heart catheterization revealing high right-sided pressures: mean pulmonary artery pressure of 28 mm Hg, systolic pulmonary artery pressure of 41 mmHg and mean pulmonary capillary wedge pressure of 12 mmHg. Cardiac output was high at 8 L/min (5.2 L/min/m2 for cardiac index using Fick method). Successive oxygen saturations analysis revealed no intra-cardiac shunt.
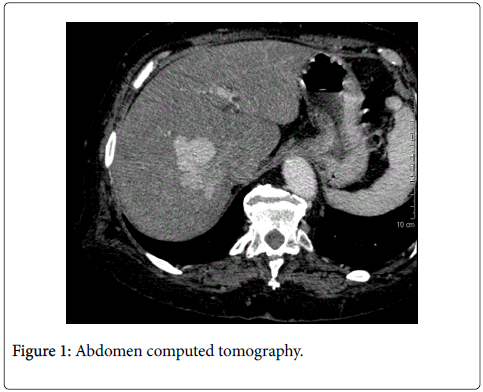
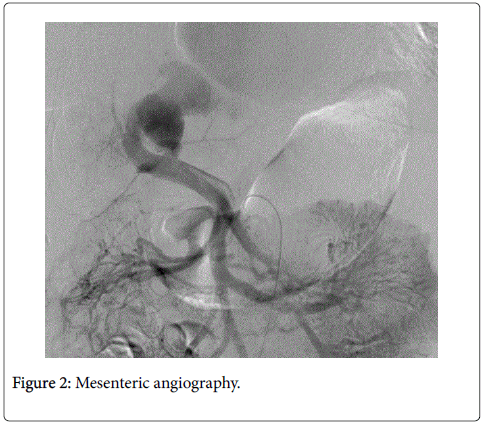
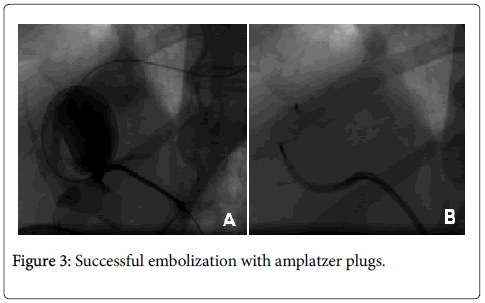
Thyroid function and haemoglobin were in physiological ranges, and therefore helped excluding differential diagnoses of congestive heart failure with high cardiac output. Hepatic cirrhosis was excluded as well. A chest, abdomen and pelvis computed tomography found a large porto-systemic shunt between the right side of the portal vein and the right sub-hepatic vein (Figure 1), a major dilatation of the inferior vena cava and the right atrium with no anomalous pulmonary venous return. A mesenteric angiography was subsequently performed and confirmed the porto-systemic shunt (Figure 2) which was successfully embolized with amplatzer plugs (Figure 3). During a 2 year-follow-up period, our patient did not experience any other episode of congestive heart failure. Furthermore, the echocardiogram confirmed the normalization of pulmonary artery pressures and rightsided cavities dimensions.
The most common etiologies of high cardiac output and increased pulmonary pressure include anemia, renal disease, cirrhosis, hyperthyroidism, arteriovenous fistulae and intracardiac shunts [1]. Intrahepatic portosystemic venous shunts without portal hypertension or abdominal trauma are extremely rare in adults [2] (20 patients have been reported so far). Usually, porto-systemic shunt is revealed by hepatic encephalopathy, glycoregulation disorders or liver failure but exceptionally by high cardiac output with pulmonary hypertension (only 2 cases described [3,4]). Several etiologies are possible (congenital or acquired).
In our patient, the porto-systemic shunt was probably secondary to the past cholecystectomy and it highlights that congenital intrahepatic portosystemic venous shunts are an extremely rare etiology of high output heart failure but still a curable one.
References
- Mehta PA, Dubrey SW (2009) High output heart failure. QJM Mon J Assoc Physicians102: 235-241.
- Rouveyrol F, Meyer M, Lusson JR, Dauphin C, Vanlieferinghen P, et al. (2006) Idiopathic intrahepatic portosytemic shunts in 4 children. Arch PédiatrieOrgane Off SociéteFrPédiatrie13:251-255.
- McKie PM, McCully RB, Kamath PS, Bower TC, McKusick MA, et al. (2012) Amelioration of high cardiac output and pulmonary hypertension by occlusion of congenital porto-systemic shunt. Circulation 126:2533-2534.
- Imamura H, Momose T, Kitabayashi H, Takahashi W, Yazaki Y, et al. (2000) Pulmonary hypertension as a result of asymptomatic portosystemic shunt. JpnCirc J 64: 471-473.
Relevant Topics
- Abdominal Radiology
- AI in Radiology
- Breast Imaging
- Cardiovascular Radiology
- Chest Radiology
- Clinical Radiology
- CT Imaging
- Diagnostic Radiology
- Emergency Radiology
- Fluoroscopy Radiology
- General Radiology
- Genitourinary Radiology
- Interventional Radiology Techniques
- Mammography
- Minimal Invasive surgery
- Musculoskeletal Radiology
- Neuroradiology
- Neuroradiology Advances
- Oral and Maxillofacial Radiology
- Radiography
- Radiology Imaging
- Surgical Radiology
- Tele Radiology
- Therapeutic Radiology
Recommended Journals
Article Tools
Article Usage
- Total views: 11207
- [From(publication date):
August-2016 - Mar 29, 2025] - Breakdown by view type
- HTML page views : 10389
- PDF downloads : 818