Research Article Open Access
What is the Most Effective Intervention for the Management of Dental Anxiety among Adults? A Systematic Review of Interventions
Oyedayo Mary Oyekunle, John Fulton* and Catherine HayesDepartment of Applied Sciences, University of Sunderland, Sunderland, SR1 3SD, UK
- *Corresponding Author:
- John Fulton
Faculty of Applied Sciences
University of Sunderland, Sunderland, SR1 3SD
United Kingdom
Tel: +44 191 515 2529
E-mail: john.fulton@sunderland.ac.uk
Received date: November 16, 2016; Accepted date: November 23, 2016; Published date: November 30, 2016
Citation: Oyekunle OM, Fulton J, Hayes C (2016) What is the Most Effect Treatment for the Management of Dental Anxiety among Adults? A Systematic Review of Interventions. J Comm Pub Health Nurs 2:146. doi:10.4172/2471-9846.1000146
Copyright: © 2016 Oyekunle OM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Community & Public Health Nursing
Abstract
This review aimed to find the most effective intervention for the management of dental anxiety among adults by way of a systematic review of Randomised controlled trials. Compared to European and US counterparts, the number of studies concerning the management of dental anxiety in the United Kingdom is limited. Several interventions have been reported with varying modes of action and duration. Two main groups of interventions: pharmacological and psychological/behavioural have been implemented. The pharmacological interventions employ the use of centrally acting sedatives whereas the psychological/behavioural interventions serve to change the behavioural and learning effects of dental anxiety. A third group operationally defined as “Complementary” for the purpose of this review consists of holistic therapies such as acupuncture, music distraction and aromatherapy for in the management of dental anxiety. Although reduction of dental anxiety before and after dental treatment has been recorded historically in the majority of trials, these have mainly investigated psychological/behavioural interventions. Exploring more recent trials, this study uncovers the benefits of complementary interventions for managing dental anxiety in adults and computer based variants of psychological/behavioural interventions. None compared the efficacy of one type or group against the other. Also, outcomes such as avoidance of dental treatment and economic implication of interventions were scarcely evaluated thus evidence on this remains inconclusive. The need for further investigation of these outcomes as well as those in Complementary Therapies is justified.
Keywords
Anxiety; Interventions; Complementary therapies
Introduction
Dental anxiety affects about 4-30% of adults across the world [1,2]. This condition is known to be associated with avoiding the dental environment all together as a mechanism to cope with the anxiety and further leads to a deterioration of oral health status and oral health related quality of life [2-6]. Factors implicated in the anxiety of dental anxiety include fear of dental pain, discomfort, perceived lack of control over dental events, perceived negative attitude of dental staff, influence of other dentally anxious peers, past traumatic dental experiences [7-11].
In the United Kingdom alone according to the 2009 adult dental health survey, 40% of the adult population had some degree of dental anxiety [10]. Anxiety towards dental procedures often results in delay, postponement or cancellation of appointments. It has been reported that dentally anxious patients had more decayed teeth, higher number of missing teeth and gum problems compared to non-anxious patients [12,13]. Many patients report that shame and embarrassment are common experiences; as dental conditions deteriorate tends to escalate and constitute a financial burden [14,15].
As a consequence, various interventions have been employed to reduce dental anxiety. These include the use of medication, the use of cognitive and behavioural approaches (psychological interventions and the use of alternative therapies. The ability of a dentist identify an anxious patient from the outset. Ancillary members of the dental team may also be able to contribute to the management of dental anxiety as they are often the first in line of management of a dental patient [16]. Another avenue that has been explored in the management of dental anxiety is use of online dental support groups for anxious adults. A study of an online support group reported that participants found the group to be useful in assisting them to confront their debilitating anxiety and successfully receive dental care [17].
The problem and management of dental anxiety as well as the negative impact on the oral health and oral health related quality of life has been researched since the 20th century [11,18]. Yet oral health policies in the United Kingdom till date are devoid of strategies to tackle such an important determinant of oral healthcare utilization [19]. Furthermore, guidelines for the management of dental anxiety in the United Kingdom are predominantly available for children [20]. The present management of dental anxiety among adults in the United Kingdom typically involves referring them to special care dentistry clinics or clinics of oral medicine [21].
The purpose of the present review was to systematically review available literature and present evidence on the most effective intervention to reduce dental anxiety.
Methods
Search Strategy: A three stage search strategy [22] was used search for studies reporting randomized controlled trials RCTs published in English language spanning from January 2007 to June 2014. The first stage included a limited search of databases such as Cochrane Central register of trials, EMBASE, PUBMED and MEDLINE to identify search terms followed by an analysis of the text words in the title and abstract, and search terms in the article. A second stage search using all identified keywords and index terms was then undertaken. The third step consisted of a search of the reference lists of all identified reports and articles for additional studies as well as unpublished studies from grey literature. Hence the following databases : Cochrane Register of Trials, MEDLINE, EMBASE, Trip database, Clinical trials.gov, NHS evidence, DISCOVER, CINAHL were searched.
Study selection
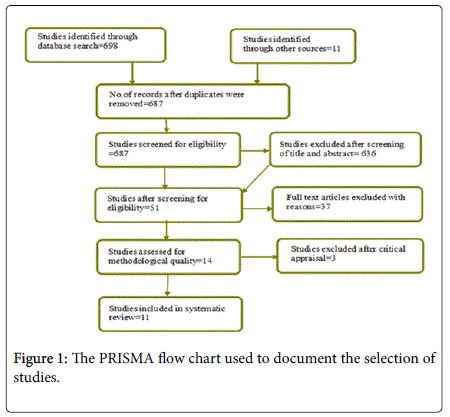
Studies had to fulfil the participant, intervention and outcome components of the question. and studies were all randomised controlled trials on interventions for management of dental anxiety among adults. Studies were excluded after screening through titles, abstracts and then inclusion and exclusion criteria. Participants were adults older than 18 years of age who did not have confounding anxiety disorders, learning disabilities or special needs. Included interventions were pharmacological interventions (use of benzodiazepines); non-pharmacological/psychological interventions (based on cognitive behavioural therapy and behavioural therapy (CBT/BT) and a third group called complementary therapies for the purpose of this study (these included acupuncture, music therapy, muscle relaxation, aromatherapy). Studies were not selected by outcome (Figure 1).
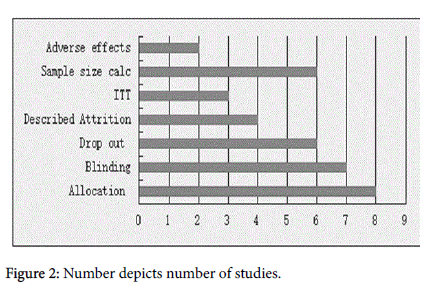
Assessment of quality of included studies
Studies in this review were assessed using the Critical Appraisal Skills Program (CASP) toolkit [23]. This tool kit evaluated randomization, accountability for patients, blinding of participants and investigator, withdrawals, treatment effect, applicability of study results to clinical practice or local context. This tool did not have a scoring system. Assessment of individual components of methodological quality was carried out and a pictorial representation of risk of bias is shown below (Figure 2).
Data Extraction: Data from the included studies were extracted using the Joanna Briggs institute data extraction tool.
Results (Data Synthesis)
After assessing for methodological quality and inclusion and exclusion criteria, 11 studies were included in this systematic review. A total of 1316 participants were randomized into groups and 1254 completed the studies with an age range of 18-65 years. The included studies were published between 2007 and 2013. Three of the studies took place in the USA [24-26]. Eight took place in Europe 2 in the UK [27,28], three in Germany [29-31] one in Austria [32,33]. another in Greece [33] and the last in Norway [34]. All 11 studies evaluated the effects of intervention on dental anxiety, state dental anxiety [27,28,30-32,34] dental phobia [29] and dental injection phobia [24].
The interventions included were: Pharmacological (4 mg of intranasal midazolam [30]; 0.5 mg and 0.75 mg Alprazolam [26]. The complementary interventions included the use of auricular acupuncture [30,32] Lavender scent oil [33]; brief relaxation and music therapy [31]. The psychological interventions included the use of Cognitive behavioural therapy (CBT) [34] Process simulations [27]; Eye movement desensitization and reprocessing (EMDR) [29] Completion of dental anxiety survey [28]; Biofeedback technique [24]; Computer assisted relaxation learning (CARL) [25].
Outcome measures were dental anxiety scales such as dental anxiety survey (DAS) ,modified dental anxiety scale (MDAS), visual anxiety scale (VAS), Spielberg state trait anxiety inventory; X1 form (STAI-X1) and dental fear scale (DFS). Results were expressed as mean scores of dental anxiety scale by group and p values of mean differences.
The findings, summarised in Table 1, will be discussed using intervention groups: Pharmacological, non-pharmacological/ psychological.
Meta-Analysis
This statistical analysis of data from trials in a study increases the how precise the estimate of a treatment effect is and can be applied when results are presented in odds ratios, relative risks [36]. This is not the case with this review. Trials in this review presented results using different interventions, diverse outcome measures, and varied methods of analysis. Though a meta-analysis was considered initially, it was not possible.
| No. | Author's name | Type of Design | Type of Intervention | Is study in favour of experimental or control group | Outcome measure | Outcome I | Outcome II | Intervention/Mean anxiety scale scores | Intervention/Mean anxiety scale scores |
|---|---|---|---|---|---|---|---|---|---|
| Pre treatment | Post treatment | ||||||||
| 1 | Coldwell et al. [27] | Randomised controlled trial | Pharmacological vs. Psychological intervention | No | DAS Scores | Dental anxiety | Avoidance of Dental Appointments | NR | NR |
| 2 | Karst et al. [31] | Randomised controlled trial | Pharmacological vs. Complementary intervention | Yest to both | STAI-IX and VAS Scores | State dental anxiety | (STAI-IX) Aur Acu: 50.47(8.83) Pla Acu:49.32(13.49) Mida:56.53(9.61) CNTRL:53.00(9.61) |
Aur Acu: 41.84 (12.72)Â Pla Acu: 39.16(9.87) Mida: 38.68(9.19) CNTRL: 47.20(12.78) |
|
| 3 | Haukebo et al. [35] | Randomised controlled trial | cognitive behavioural therapy, one vs. five sessions and wait-list | Yest to both | DAS, BAT, DFS, DBS scores | State dental anxiety | Avoidance of dental treatments | (DAS) One S: 16.6 (2.8) Five S: 16.6 (2.8) |
One S: 10.4 (3.4) Five S: 10.1 (3.2) |
| 4 | Hull and Humphris [29] | Randomised clinical trial | Behavioural therapy | Yes, dental anxiety reduced when patient knew that dentist received Das and discussed their anxiety with them | Mean STAI-s scores | State dental anxiety | NR | NR | |
| 5 | Kritsidima et al. [34] | Cluster Randomised controlled trial | Complementary intervention (Lavender vs. control) | Yes | STAL-6 score, MDAS | State dental anxiety | (STAI-6) LAV: 9.84 (4.74) CNTRL: 10.65 (5.40) |
LAV: 7.41 (2.43) CNTRL: 10.71 (4.35) | |
| 6 | Michalek-Sauberer et al. [33] | Randomised controlled trial | Complementary intervention (Acupuncture vs. control) | Yes | STAI, VAS scores | State dental anxiety | (STAI)Aur Acu: 54.7 (10.8) Sham: 51.9 (10.2) CNTRL: 51.0 (11.7) |
Aur Acu: 46.9 (10.4) Sham: 48.4 (10.0) CNTRL: 54.0 (11.6) | |
| 7 | Lahmann et al. [32] | Randomised controlled trial | Complementary intervention (Brief relaxation, music distraction and control) | Yes | STAI, HAQ scores | State dental anxiety | (STAI) BR: 42.4 (10.4) MD: 41.3 (9.6) CNTRL: 41.9 (11.5) | BR: 29.4 (6.3) MD: 36.8 (9.8) CNTRL: 41.9 (11.5) |
|
| 8 | Doering et al. [30] | Randomised controlled trial | Â Psychological intervention (Eye movement densitisation and reprocessing vs. wait-list group) | Yes | Post treatment DAS scores 3.6.12 month follow up with DAS, DFS scores | Dental phobia | Avoidance of dental visits | (DAS) EMDR: 18.2 (1.6) CNTRL: 18.1 (1.8) |
 EMDR: 12.2 (2.9) CNTRL: 17.9 (1.2) |
| 9 | Morarend et al. [25] | Explorator Randomised controlled trial | Â Psychological intervention (Biofeedback technique and control) | Yes | VAS, DAS scores | Negative feeling toward dental injection (Dental Anxiety) | (VAS) RESP: 15.05 (2.91) CNTRL: 14.20 (3.11) |
RESP: 9.9 (2.94) CNTRL: 8.88 (2.34) |
|
| 10 | Armitage and Reidy [28] | Explorator Randomised controlled trial | Â Psychological intervention (Process simulation of dental treatment) | Yes | STAI scores | State dental anxiety | (STAI) P.S: 2.06 (0.80) CNTRL: 1.55 (0.51) |
P.S: 2.20 (0.83) CNTRL: 1.73 (0.46) |
|
| 11 | Heaton et al. [26] | Randomised clinical trial |  Psychological intervention (Computerised systemic densitisation and control) | Yes | MDAS, DAS scores | Denatl fear | (MDAS) CARL:19.6 (14.0) CNTRL: 20.5 (3.0) |
 CARL: 13.5 (3.0) CNTRL: 18.5 (3.0) |
Table 1: Summary of findings.
Discussion
The number of Randomised controlled trials (RCTs) in this review reporting the use of pharmacological and complementary interventions is limited compared to those reporting the use of psychological/behavioural interventions as 6 of 11 trials used psychological approaches such as one or five sessions of CBT [34]; systematic desensitization [25,26]; biofeedback techniques [24]; process simulations [27]; eye movement desensitisation and reprocessing (EMDR) [29] and completion of dental anxiety questionnaires with the knowledge that the dentist would be willing to discuss their anxiety [28]. Results were found to statistically significant
in five of these RCTs. Two RCTs reported the use of pharmacological interventions where the reduction in dental anxiety was not statistically significant. The third group applied the use of music distraction [31], auricular acupuncture [32] and aromatherapy (lavender scent oil) [33] and were found to reduce dental anxiety among patients.
Other outcomes such as reduction of avoidance behaviour, adverse outcomes and economic implication were scarcely evaluated in included RCTs. Four studies in this review assessed this outcome with follow up periods of up to one year. Economic implication of interventions were not reported in any of the trials, however authors of the two complementary interventions concluded that they were inexpensive as they did not require any specialised equipment [31,33]. Adverse reactions were reported in two RCTs where 7% of participants who received intranasal midazolam (pharmacological intervention) described burning sensations in their nostrils [30]. 20% of participants who received auricular acupuncture also complained of tingly sensations on the ear where they had received acupuncture [32].
Another important finding was the use of computer based interventions. Computer assisted relaxation learning (CARL) which is based on systematic desensitisation [24-26] and even cognitive behavioural therapy (CBT) were shown to reduce dental anxiety. This mode of administration could become useful and easily accessible to anxious adults from the comfort of their home. A meta-analysis of internet and computer based CBT showed that they were superior to control conditions in the reduction of anxieties in adults [36].
The reduction in dental anxiety was reported by various dental anxiety scales and questionnaires without uniformity or particular detail on number or percentage of participants who actually showed this reduction or the magnitude of the reduction. Adequate diagnosis and stratification of levels of dental anxiety among participants was reported in only two studies [26,29]. This lack of diagnosis makes it difficult to accurately measure rate of improvement of participants hence results are only generalizable without specific indication for management of people with lower or higher levels of dental anxiety/ phobia.
This review included trials which were published within the last seven years. A longer duration and a wider hand search to include journals and studies not published in English language may also have returned more studies. Some studies scored low on the CASP toolkit used to assess for methodological quality but were included in this review. This gave the opportunity to compare various studies, note strengths and limitations and then make recommendations.
Recommendations for Research
Diagnosis
Different levels of dental anxiety would require different forms of intervention and in some cases a combination of interventions. Hence case-studies or trials matching interventions to level of anxiety are recommended.
Sample sizes
Sample sizes of trials in this review were quite small as they ranged from 31 to 340 participants which minimizes generalizability the chances of concluding that positive results in a small population will be the same in the larger general population.
Follow-up
Only two studies assessed effect of intervention on participants at follow-up intervals ranging from 1month to a year; and therefore could not assess the long term benefits. It is therefore recommended that studies measure outcomes at longer follow up intervals.
Recommendations for Practice
Evidence from this review supports the application of psychological/ behavioural interventions in the management of dental anxiety among adults. The use of dental anxiety questionnaires may be employed as a routine measure within general medical and dental practices to identify dentally anxious adults, refer where necessary and manage as appropriate. Computer-based psychological interventions have been indicated as effective in reducing dental anxiety.
Conclusion
Although this review set out to compare the effectiveness of one intervention against the other, studies were mostly found to be compared against a control condition with the exception of one study. The results of this systematic review indicate the short term benefits of psychological interventions over the pharmacological and complementary interventions in reducing dental anxiety within a clinical setting. This conclusion is not considered firm due to the lack of uniform measurement of dental anxiety; inadequate evidence of adverse effects and economic implication and short length of follow-up in most of the trials.
References
- Milgrom P, Heaton LI, Newton IT (2013) Different Treatment Approaches in Different Cultures and Health-Care Systems: Cognitive Behavioral Therapy for Dental Phobia and Anxiety.
- McGrath C, Bedi R (2004) The association between dental anxiety and oral health-related quality of life in Britain. Community Dentistry and Oral Epidemiology 32: 67âÂ?Â?72.
- Newman MG, Llera SJ (2011) A novel theory of experiential avoidance in generalized anxiety disorder: A review and synthesis of research supporting a contrast avoidance model of worry. Clinical Psychology Review 31: 371-382.
- Oosterink FM, de Jongh A, Hoogstraten J (2009) Prevalence of dental fear and phobia relative to other fear and phobia subtypes. Eur J Oral Sci 117: 135-143.
- Oosterink FMD, De Jongh A, Aartman IHA (2009) Negative events and their potential risk of precipitating pathological forms of dental anxiety. Journal of Anxiety disorders 23: 451-457.
- Cohen SM, Fiske J, Newton JT (2000) The impact of dental anxiety on daily living. Br Dent J 189: 385-390.
- Abrahamsson KH, Berggren U, Hallberg L, Carlsson SG (2002) Dental phobic patients' view of dental anxiety and experiences in dental care: A qualitative study. Scand J Caring Sci 16: 188-196.
- Klingberg G (2008) Dental anxiety and behaviour management problems in paediatric dentistry-a review of background factors and diagnostics. European Archives of Paediatric Dentistry 9: 11-15.
- Raghad H, Walsh LJ (2009) Dental anxiety: Causes, complications and management approaches. Journal of Minimum Intervention in Dentistry 2: 67-78.
- Locker D, Thomson WM, Poulton R (2001) Psychological disorder, conditioning experiences and the onset of dental anxiety in early adulthood. Journal of dental research 80: 1588-1592.
- Skaret E, Soevdsnes EK (2005) Behavioural science in dentistry. The role of the dental hygienist in prevention and treatment of the fearful dental patient. International journal of dental hygiene 3: 2-6.
- Tvermyr K, Hoem AF, Elde KM (2012) Clinical management of the adult patient with dental anxiety.
- Hakeberg M, Berggren U, Gröndahl HG (1993) A radiographic study of dental health in adult patients with dental anxiety. Community dentistry and oral epidemiology 21: 27-30.
- Locker D (2003) Psychosocial consequences of dental fear and anxiety. Community Dent Oral Epidemiol 31: 144-151.
- Bourley A (2012) Dentistry cost exceed cancer spend.
- Skaret E, Soevdsnes EK (2005) Behavioural science in dentistry. The role of the dental hygienist in prevention and treatment of the fearful dental patient. Int J Dent Hyg 3: 2-6.
- Buchanan H, Coulson NS (2007) Accessing dental anxiety online support groups: An exploratory qualitative study of motives and experiences. Patient education and counselling 66: 263-269.
- Armfield JM (2010) Towards a better understanding of dental anxiety and fear: cognitions vs. experiences. Eur J Oral Sci 118: 259-264.
- DH (2013) Delivering better oral health: an evidence-based toolkit for prevention-third edition.
- (2014) NICE guidelines.
- Boman WU, Carlsson V, Westin M, Hakeberg M (2013) Psychological treatment of dental anxiety among adults: A systematic review. European journal of oral sciences 121: 225-234.
- Higgins JP, Green S (2005) Cochrane handbook for systematic reviews of interventions 4.2.5. The Cochrane Library.
- Public Health Resource Unit (PHRU) (2006) The critical skills appraisal programs: Making sense of evidence. Public Health Resource Unit, England.
- Morarend QA, Spector ML, Dawson DV, Clark SH, Holmes DC (2011) The use of a respiratory rate biofeedback device to reduce dental anxiety: An exploratory investigation. Applied psychophysiology and biofeedback 36: 63-70.
- Heaton LJ, Leroux BG, Ruff PA, Coldwell SE (2013) Computerized Dental Injection Fear Treatment: A Randomized Clinical Trial. Journal of dental research 92: 37-42.
- Coldwell SE, Wilhelm FH, Milgrom P, Prall CW, Getz T, et al. (2007) Combining alprazolam with systematic desensitization therapy for dental injection phobia. Journal of anxiety disorders 21: 871-887.
- Armitage CJ, Reidy JG (2012) Evidence that process simulations reduce anxiety in patients receiving dental treatment: Randomized exploratory trial. Anxiety, Stress & Coping 25: 155-165.
- Hull P, Humphris GM (2010) Anxiety reduction via brief intervention in dentally anxious patients: A randomized controlled trial. Social Science and Dentistry.
- Doering S, Ohlmeier MC, Jongh A, Hofmann A, Bisping V (2013) Efficacy of a trauma focused treatment approach for dental phobia: a randomized clinical trial. European journal of oral sciences 121: 584-593.
- Karst M, Winterhalter M, Munte S, Francki B, Hondronikos A, et al. (2007) Auricular acupuncture for dental anxiety: a randomized controlled trial. Anesthesia & Analgesia 104: 295-300.
- Lahmann C, Schoen R, Henningsen P, Ronel J, Muehlbacher M, et al. (2008) Brief relaxation versus music distraction in the treatment of dental anxiety. J Am Dent Assoc 139: 317-324.
- Michalek-Sauberer A, Gusenleitner E, Gleiss A, Tepper G, Deusch E (2012) Auricular acupuncture effectively reduces state anxiety before dental treatment: A randomized controlled trial. Clinical oral investigations 16: 1517-1522.
- Kritsidima M, Newton T, Asimakopoulou K (2010) The effects of lavender scent on dental patient anxiety levels: A cluster randomized controlled trial. Community dentistry and oral epidemiology 38: 83-87.
- Haukebo K, Skaret E, ÃÂ?st LG, Raadal M, Berg E, et al. (2008) One-vs. five-session treatment of dental phobia: A randomized controlled study. Journal of behavior therapy and experimental psychiatry 39: 381-390.
- Haidich AB (2010) Meta-analysis in medical research. Hippokratia 14: 29-37.
- Reger MA, Gahm GA (2009) A meta-analysis of the effects of internet and computer based cognitive behavioral treatments for anxiety. Journal of Clinical Psychology 65: 53-75.
Relevant Topics
- Chronic Disease Management
- Community Based Nursing
- Community Health Assessment
- Community Health Nursing Care
- Community Nursing
- Community Nursing Care
- Community Nursing Diagnosis
- Community Nursing Intervention
- Core Functions Of Public Health Nursing
- Epidemiology
- Epidemiology in community nursing
- Health education
- Health Equity
- Health Promotion
- History Of Public Health Nursing
- Nursing Public Health
- Public Health Nursing
- Risk Factors And Burnout And Public Health Nursing
- Risk Factors and Burnout and Public Health Nursing
Recommended Journals
- Epidemiology journal
- Global Journal of Nursing & Forensic Studies
- Global Nursing & Forensic Studies Journal
- global journal of nursing & forensic studies
- journal of community medicine& health education
- journal of community medicine& health education
- Palliative Care & Medicine journal
- journal of pregnancy and child health
Article Tools
Article Usage
- Total views: 5746
- [From(publication date):
November-2016 - Mar 31, 2025] - Breakdown by view type
- HTML page views : 4827
- PDF downloads : 919