What is the Agreement Between 6MWD And CPET Performance in COPD?
Received: 04-Jul-2022 / Manuscript No. jcpr-22-69814 / Editor assigned: 06-Jul-2022 / PreQC No. jcpr-22-69814 (PQ) / Reviewed: 20-Jul-2022 / QC No. jcpr-22-69814 / Revised: 22-Jul-2022 / Manuscript No. jcpr-22-69814 (R) / Published Date: 29-Jul-2022 DOI: 10.4172/jcpr.1000169
Abstract
Introduction: Chronic Obstructive Pulmonary Disease patients typically present breathlessness and reduced exercise capacity. Our study aimed to better understand the correlation between 6MWD and CPET performance.
Methods: We conducted an observational prospective study. Consecutive stable COPD patients referred to the Lung Function Laboratory were recruited.
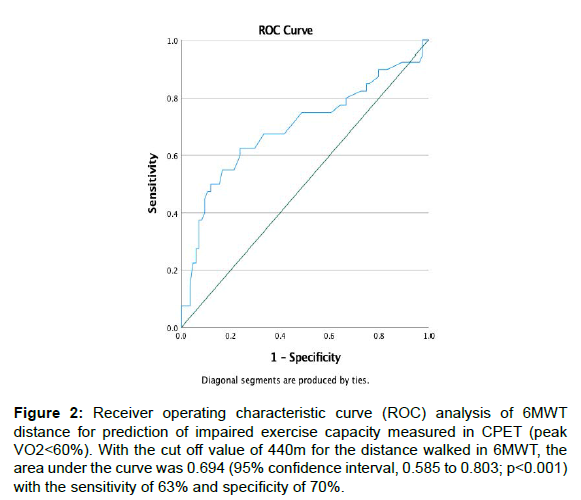
Results: Our 116 patients were predominantly male (88%), very symptomatic (68% GOLD B or D) and nonexacerbators (69%). Most patients had severe or very severe airflow limitation (55%) - median FEV1 was 48% (IQ 38-68). Median DLCO was 58% (IQ 46-75). Median 6MWD was 480m (406-515) and median workload (CPET) was 64W (46-88) with peakVO2 15.7L/min/kg (13.6-18.1). Median ΔSpO2 was 5% (3-9%) in 6MWT and 2% (1-6) in CPET. FEV1 and DLCO were important predictors of exercise capacity and desaturation in CPET and 6MWT. The 6MWD correlated with CPET peak workload and peak VO2; 6MWD of 440m estimates reduced exercise capacity in CPET (VO2 <60%).
Conclusion: 6MWD can estimate CPET peakVO2.
Keywords
COPD; Exercise performance; 6MWD, Peak VO2
Introduction
Chronic obstructive pulmonary disease (COPD) is a progressive disease characterized by breathlessness and daily life activities impairment [1]. Assessment of exercise capacity is an important marker for patients´ ability to perform daily tasks, to determine disease severity and progression over time, to assess treatment response it also it is a prognostic marker for survival [2-4].
The 6-minute walk test (6MWT) is the most used exercise test mainly due to the simplicity. The 6MWT is self-paced and can be continuous or intermittent, depending on whether the subject rests during the test. It is a quick, reproducible, robust, and cheap field exercise test and distance walked during the test is used to predict disease`s severity and rehabilitation response [5,6]. The variation in the 6 minute walking distance (6MWD) correlates well with spirometry and FEV1 [7,8] and predicts mortality in COPD patients [9-11] despite patients` comorbidities [11,12]. Oxygen desaturation during 6MWT is common in COPD patients independently of their comorbidities [13] and was also previously identified as a marker for exacerbations and survival [14].
The cardiopulmonary exercise test (CPET) is more complex than 6MWT but allows the thorough understanding of a patient’s level of exercise limitation and its causes [15,16]. For this purpose, it is the “gold standard” but also more expensive and may be difficult to execute. Peak VO2 obtained from CPET has also been shown to be a predictor of mortality in COPD [17] CPET is also used to indicate workload levels in rehabilitation programs [18].
Comparing 6MWT and CPET in COPD patients, previous studies suggested that both heart rate (HR) and dyspnoea were greater during the 6MWT than during CPET [19] but also that greater desaturation and a more profound hypoxemia occurs at the end of the field walking tests compared to the end of the CPET [20]. The reasons for this difference remain unclear but are probably related to increased ventilation/perfusion mismatching during walking; differences in body posture, functional residual capacity, and/or pulmonary hemodynamic; the effect of reflex impulses to the respiratory centres arising from the upper limb muscles, probably more active during walking than cycling; higher ventilation during cycling due to higher levels of lactate accumulation and an increased chemical drive to breathe while walking [8,20]. Recently Gupta R, et al. [21] identified diffusion capacity for carbon monoxide (DLCO) as the only significant independent predictor for the magnitude of O2 saturation variation (ΔSpO2) and the occurrence of O2 desaturation of at least 4% during the 6MWT [21] and DLCO cut-off 45% appeared promising to identify patients at risk for exertional hypoxemia during a 6MWT [18]. Previous studies proposed different equations to estimate peak VO2 using 6MWT parameters but the agreement between measured and estimated peak VO2 or peak work using these equations was poor to moderate and the 11 available equations did not estimate peak VO2 or peak work sufficiently to be used effectively for prescription of exercise intensity during rehabilitation [22].
The main objective of the present study was to better understand the relation between exercise performance accessed by 6MWT and CPET in COPD patients across all GOLD stages and analyse the correlation between the 6-minute walked distances (6MWD) and peak VO2 measured during CPET. The 6MWT may be a surrogate when CPET is unavailable, or patients cannot perform the test.
Methods
Study design and population
Single-centre, prospective study to investigate relation between exercise capacity evaluated by 6MWT, a field simple test and peak exercise parameters assessed by CPET with cycle ergometer. The study protocol and all amendments were reviewed by the Ethics Committee of the Hospital-199/2018. The study was conducted according to the ethical principles of the Declaration of Helsinki. All patients signed written informed consent before any assessment was performed.
Stable COPD outpatients referred to functional assessment between October 2018 and March 2019 were considered for the study, irrespective of their age, smoking history and GOLD stage. COPD was diagnosed according to the Global Initiative for Chronic Obstructive Lung Disease (GOLD) consensus and patients had to be able of completing exercise tests (cycle ergometry-incremental protocol and 6MWT). All bronchodilators and inhaled corticosteroids were allowed in the study.
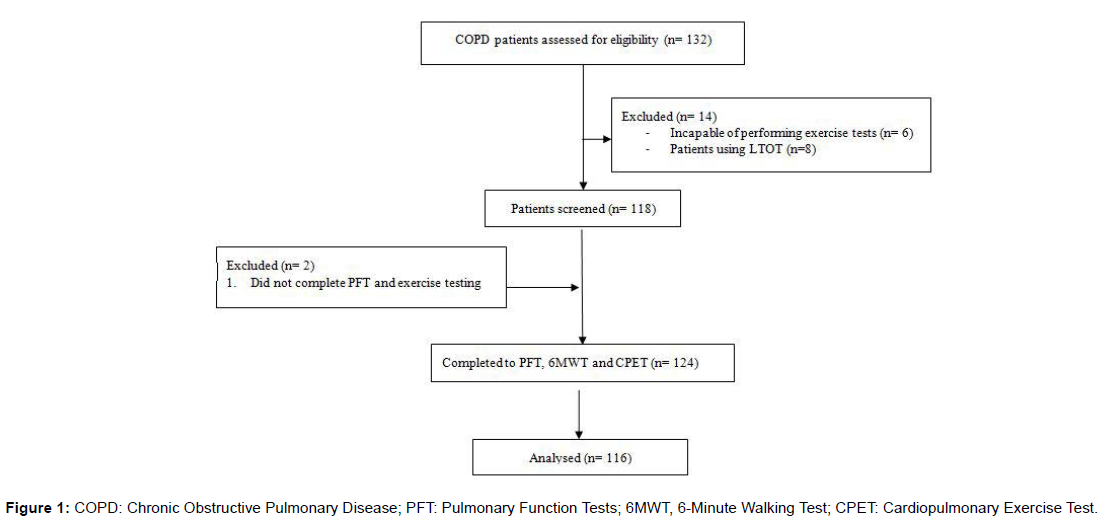
Exclusion criteria included: current documented diagnosis of asthma; a diagnosis of thyrotoxicosis; a history of myocardial infarction within 6 months; life-threatening cardiac arrhythmia; known active tuberculosis; patients with severe emphysema requiring endobronchial interventions within 6 months prior to screening; pregnancy, long term oxygen therapy (LTOT), recent COPD exacerbation (6 months) (Figure 1).
Data collection
As part of routine assessment, COPD patients did spirometry, lung volumes assessment by plethysmography and exercise tests (6MWT and CPET). Plethysmography, 6MWT and CPET were performed physicians and cardiopulmonary technicians) collected all data. by the Pulmonary Function Testing Laboratory cardiopulmonary technicians. After patients’ consent, the authors (pulmonology physicians and cardiopulmonary technicians) collected all data.
Pulmonary function testing followed the ATS/ERS guidelines [23], including routine post-bronchodilator spirometry [24] and lung volumes were assessed with plethysmography [25], using Master Screen Body (Jaeger, Wurzburg, Germany). DLCO value was corrected by haemoglobin [26].
CPET (Jaeger Vyntus CPX; Vyaire Medical) followed ATS/ ACCP standards [27,28]. An incremental modified Bruce protocol to exhaustion was specified for each participant based on reported exercise tolerance. Patients were evaluated with breath-by-breath monitoring of cardiopulmonary variables [pulmonary O2 uptake (VO2), pulmonary CO2 output (VCO2), minute ventilation (VE), heart rate (HR)], assessment of perceptual responses (dyspnoea and leg discomfort measured by BORG scale) and measurements such as exercise-related arterial oxygen desaturation and dynamic hyperinflation. Dynamic hyperinflation was assessed by measuring inspiratory capacity (IC) repetitively during CPET-patients were required to take a deep inspiration, after normal expiration, at predetermined intervals of 2 min [6]. Ventilatory limitation at peak exercise was defined by VE/maximum voluntary ventilation (MVV) above 85% [29,30]. All patients had arterial blood gas (ABG) collected before exercise testing to assess resting arterial oxygen pressure (pO2) and resting arterial carbon dioxide (pCO2) pressure: 2 ml blood were collected from the radial artery with a pre-heparinized syringe and immediately analysed using an ABL 90 flex plus blood gas analyser (Radiometer, Copenhagen, Denmark).
Exercise tolerance measured using the 6-minute walk distance testing followed the ATS recommendations [31-33]. Participants were permitted to stop during the test if their symptoms became intolerable but were encouraged to resume the walking as soon as possible. The 6MWT was monitored by a single operator who recorded the test parameters at the same time. The distance walked in the test was reported in meters and as a percentage of predicted value using reference equations previously developed for healthy population [34]. BORG scale results and pulse oxygen saturation variation (ΔSpO2) were also measured and recorded [34]. Oxygen desaturation was defined as a ≥4% reduction between arterial oxygen saturation measured by pulse oximetry pre- and post-test (Δ SpO2 ≥4%) and post-test SpO2 <90%, according to the Royal College of Physicians' guidelines [9,35]. Each patient did only one 6MWT mainly due to staff and time constraints and taking into account that we did not intent to evaluate patients over time [36].
Statistical analysis
For data description, mean ± standard deviation (sd) or median ± interquartile range (IQ) were used. Unpaired t-test and one-way ANOVA were used to compare patients’ characteristics between different groups. Correlation was evaluated by Pearson coefficient or the non-parametric Spearman rank. A significant level of p=0.05. A cut-off value for 6MWT median distance was investigated through Receiver Operating Characteristic (ROC) curve. All analyses were carried out using SPSS 26.
Statistical analysis For data description, mean ± standard deviation (sd) or median ± interquartile range (IQ) were used. Unpaired t-test and one-way ANOVA were used to compare patients’ characteristics between different groups. Correlation was evaluated by Pearson coefficient or the non-parametric Spearman rank. A significant level of p=0.05. A cut-off value for 6MWT median distance was investigated through Receiver Operating Characteristic (ROC) curve. All analyses were carried out using SPSS 26.
Results
One hundred thirty-two patients were screened for the study, but 6 patients were unable to complete exercise tests (morbid obesity or physical impairments), 2 patients failed the scheduled tests, and 8 patients were excluded due to LTOT (Figure 1).
Our group was predominately male (88%), age of 66±9 years old. Most patients reported significant symptoms - GOLD B or D (68%) and had severe or very severe airflow limitation (55%), with median FEV1 of 48% (IQ 38-68%). Static hyperinflation was present in 46 patients (40%) and 74% patients presented with dynamic hyperinflation during CPET. Forty-three patients (37%) were enrolled in pulmonary rehabilitation programs previously to study enrolment. Most patients had low DLCO (86%) – median 58% (IQ 46-75) (Table 1).
| COPD patients | |
|---|---|
| Sex: Male, n (%) | 102 (88) |
| Age (years-old) | 66 ± 9* |
| Smoking History | |
| Current smokers, n (%) | 34 (29) |
| Former smokers. N (%) | 74 (64) |
| UMA | 45 (27-60)# |
| BMI (kg/m2) | 26 ± 4* |
| Exacerbator, n (%) | 48 (41) |
| GOLD stage | |
| A, n (%) | 25 (22) |
| B, n (%) | 44 (38) |
| C, n (%) | 12 (10) |
| D, n (%) | 35 (30) |
| Inhaled Medication | |
| LAMA, n (%) | 104 (90) |
| LABA, n (%) | 108 (93) |
| ICS, n (%) | 64 (55) |
| Respiratory Rehabilitation, n (%) | 43 (37) |
| OSA, n (%) | 9 (8) |
| Heart Disease, n (%) | 17 (15) |
| ABG | |
| pO2 (mmhg) | 71± 9* |
| pCO2 (mmhg) | 41 ± 5* |
| Lung function | |
| FEV1 (%) | 48 (38-68)# |
| FVC (%) | 80 (69-92)# |
| IC (%) | 91 (74-105)# |
| TLC (%) | 115 (106-129)# |
| IC/TLC | 0.33 (0.26-0.39)# |
| RV (%) | 159(135-187)# |
| RV/TLC | 0.56 (0.48-0.62)# |
| DLCO (%) | 58 (46-75)# |
| KCO (%) | 70 (56-87)# |
| 6MWT | |
| 6MWD (m) | 480 (406-515)# |
| ∆SpO2 (%) | 5 (3-9)# |
| ∆Borg dyspnoea | 1 (0-3)# |
| ∆Borg fatigue | 2 (0-3)# |
| CPET | |
| Peak workload | 64 (46-88)# |
| Peak vo2 (ml/min) | 1100 (902-1315)# |
| Peak vo2 (ml/min/kg) | 15.7 (13.6-18.1)# |
| Peak VO2 (%) | 65 ± 14* |
| ∆SpO2 (%) | 2 (1-6)# |
| At (%peakvo2) | 47 (42-54)# |
| Ve/vco2@at | 37 (34-42)# |
| Peak o2/hr | 9.2 (7.7-10.7)# |
| Peak hr (%) | 79 (71-86)# |
| Peak VE (l/min) | 40 (32-49)# |
| Peak VE (%mvv) | 89 (71-102)# |
| Ventilatory limitation, n (%) | 82 (71) |
| Dynamic hyperinflation, n (%) | 86 (74) |
| Data presented as mean and standard deviation* or median and quartiles# and n/% for qualitative variables. AT: Anaerobic threshold; BMI: body mass index; bpm: beats per minute; CPET: Cardiopulmonary Exercise Test; DLCO: Lung diffusion capacity for carbon monoxide; FEV1: Forced Expiratory Flow in 1sec; FVC: Forced Vital capacity; GOLD: Global Initiative for Chronic Obstructive Lung Disease; HR: Heart rate; IC: Inspiratory capacity; ICS: Inhaled corticosteroid; LABA: Long acting beta agonist; LAMA: Long acting muscarinic antagonist; L: Liters; m: metres; ml: millilitre; Min: Minimum; min: minute; mmHg: millimetre of mercury; MVV: Maximal voluntary ventilation; n: number; OSA: Obstructive sleep apnoea; PaO2: Arterial pressure of oxygen; PaCO2: Arterial pressure of carbon dioxide; KCO: Carbon monoxide transfer coefficient; peak O2/HR: Peak oxygen pulse; peak W: peak incremental cycle work rate; peak VO2: peak oxygen uptake; RV: Residual volume; SpO2: pulse oxygen saturation; TLC: Total lung capacity; VE: Minute ventilation; VE/VCO2: Minute ventilation/carbon dioxide production; W: watt; 6MWT: 6-minute walk test; 6MWD: 6-minute walk distance; %: percentage; %pred: percentage predicted. |
|
Table 1: Characteristics of study participants.
The median 6MWD was 480 meters (406-515) and in CPET, median workload was 64 watts (46-88) with peak VO2 of 15.7 L/min/ kg (13.6-18.1), 65±14% predicted. Median ΔSpO2 in 6MWT was 5% (3-9%), which was greater than ΔSpO2 in CPET (2%, 1-6%). Lower FEV1 and DLCO correlated with reduced exercise capacity and ΔSpO2 in both CPET and 6MWT (Table 2).
| 6MWT | |||||
|---|---|---|---|---|---|
| Distance (m) | ∆SpO2 (%) | ∆Borg dyspnoea | ∆Borg fatigue | ||
| Lung function | FEV1 (%) | .239* | -.302** | -.324** | -0.108 |
| DLCO | .378** | -.454** | -.430** | -0.097 | |
| (%) | |||||
| ABG | pO2 (mmHg) | .276** | -.354** | -.209* | 0.013 |
| pCO2 (mmHg) | -0.119 | .265** | 0.062 | -0.086 | |
| BMI | -0.184* | -0.087 | -0.084 | 0.141 | |
| Significant correlations on bold, * p<0.05, ** p<0.01 | |||||
Table 2: Pearson’s correlations between BMI, FEV 1, DLCO and ABG parameters and exercise capacity evaluated by CPET and 6MWT.
Hypoxemia and hypercapnia assessed by ABG correlated with ΔSpO2 in CPET and 6MWT. Interestingly, lower pO2 and higher pCO2 also predicted lower peak workload in CPET.
Higher BMI was weakly associated with diminished 6MWD but conversely, in cyclergometry, the lower BMI had a moderate correlation with lower peak VO2 and lower peak O2/HR.
In 6MWT, the distance walked, ΔBorg dyspnoea and ΔSpO2 were associated with the majority of CPET parameters: peak workload, peak VO2, ΔSpO2, VCO2 equivalents, peak O2 pulse and peak maximum ventilation (Table 3).
| CPET | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Peak workload (watts) | Peak VO2 (mL/min) | Peak VO2 (%predicted) | Peak VO2/kg (ml/min/kg) | ∆SpO2 (%) | AT (%) | VE/VCO2 @AT |
Peak O2/HR | Peak HR (%predicted) | Peak VE (L) | Peak VE (%MVV) | ||
| Lung function | FEV1 (%) | .420** | .371** | .541** | .197* | -.285** | .260* | 0,120 | .313** | .230* | .676** | -.529** |
| DLCO (%) |
.482** | .588** | .577** | .313** | -.394** | .294** | -.368** | .461** | .260** | .358** | -.212* | |
| ABG | pO2 (mmHg) | .216* | 0.182 | 0.132 | 0.146 | -.261** | -0.107 | -0.078 | 0.069 | .219* | 0.176 | -0.181 |
| pCO2 (mmHg) |
-.236* | -0,142 | -0,088 | -0,125 | .272** | 0,137 | -.448** | -0,066 | -0,095 | -.452** | 0.101 | |
| BMI | 0,147 | .384** | .334** | -0,145 | -0,102 | .411** | -.220* | .490** | -0,069 | .187* | -0.134 | |
| Significant correlations on bold, * p<0.05, ** p<0.01 | ||||||||||||
Table 3: Pearson’s correlations between BMI, FEV 1, DLCO and ABG parameters and exercise capacity evaluated by CPET.
The distance walked in 6MWT correlated with exercise capacity in CPET, with higher peak workload and peak VO2 in patients that walked more meters. Increased ΔSpO2 and ΔBorg dyspnoea in 6MWT were associated with reduced exercise capacity in CPET (workload and peak VO2).
A shorter distance covered in the 6MWT was associated with a reduced peak VO2 in CPET and a distance < 440m related to peak VO2 <60% predicted, reflecting greater exercise impairment and bigger disability in COPD patients (Figure 2).
Figure 2: Receiver operating characteristic curve (ROC) analysis of 6MWT distance for prediction of impaired exercise capacity measured in CPET (peak VO2<60%). With the cut off value of 440m for the distance walked in 6MWT, the area under the curve was 0.694 (95% confidence interval, 0.585 to 0.803; p<0.001) with the sensitivity of 63% and specificity of 70%.
Discussion
Our study included a large cohort of patients with clinically stable COPD across all GOLD severities (A-D) and was one of the few to consider the relationship between exercise capacities measured with both field and laboratory studies.
As previously described, we also found that FEV1 and DLCO were important predictors of exercise capacity and desaturation in both CPET and 6MWT [21]. ΔSpO2 was higher in 6MWT than CPET, also as expected [19,20]. Patients with hypoxemia and hypercapnia had higher ΔSpO2 in both tests, but they also had lower exercise capacity in CPET, despite these were poor correlations. Perez T, et al. [13] reported that resting SpO2 was a poor marker for desaturation during 6MWT. To our knowledge this is the first study to look at ABG resting parameter’s ability to predict exercise capacity measured by 6MWT and CPET. Further studies are necessary to improve the understanding of this correlation but pO2 and pCO2 may be helpful predictors of exercise capacity in stable COPD patients.
The distance walked during field walking test was high in our group compared to previous studies [13,22], which is probably related to the inclusion of patients from all GOLD stages and also due to the inclusion of patients already enrolled in pulmonary rehabilitation programs (37%). PR is known to improve exercise performance with 6MWT and CPET (mean improvements of 44 m and 11% peak in VO2 and 6.8 w in peak workload, respectively) [6] and probably contributed to the mean distance walked in the 6MWT and peak workload and VO2 in CPET, despite the severity of the patients enrolled. Walking but not cycling performance was negatively influenced by weight, corroborating Sava F, et al. findings [37] but further analysis of the overweight and obese COPD population can improve our comprehension of the underlying mechanisms of this association.
One limitation of our study is the lack of duplicate 6MWT but most of the included patients had previously performed the test (88%), minimizing the impact of a potential lack of the learning effect. Also, according to the ATS/ERS technical standards, a second test is more relevant for comparison over time than for single time evaluation studies [33].
It’s well established that the 6MWT is a powerful exercise test to evaluate and follow COPD patients over time [1,6,36] and it was also previously demonstrated that the mean walked distance and desaturation during 6MWT may also predict exacerbations and survival [9,14,17] but in our study, we corroborated that the walked distance correlated moderately to peak workload and peak VO2 achieved during the incremental CPET [17,19] and most importantly, we were able to establish that a walked distance bellow 440 m estimates reduced exercise capacity in CPET (VO2 <60%), which was never described before. This was previously tried by Kirkham AA, et al. [22], through equations capable of estimating peak VO2 or peak workload using the 6MWT parameters, but the agreement between measured and estimated peak VO2 or peak workload using these equations revealed to be below the threshold for reasonable clinical test validity. A significant relationship between VO2 measured by 6MWT and CPET was previously found in patients with more severe COPD but not in mild to moderate disease stages [38].
The sample size and wide spectrum of disease severity are strengths of the study. Another strength of our work is the representation of realworld clinical practice, since we included both non-smokers (7%) and smokers or former smoker patients and we did not exclude patients with cardiac disease-15% (5 patients had cardiac arrhythmias, 2 had valvular disease, 2 had ischemic heart disease and 6 had heart failure), contrasting with previous studies.
Conclusion
CPET and 6MWT are complementary tests but cannot be used interchangeably. CPET remains an important tool in COPD patient’s evaluation since it can provide information on the nature of the cardiopulmonary response to an exercise, which is not accessed by 6MWT. Nonetheless, 6MWT informs the clinician about exercise capacity, helps to predict exacerbations and survival and according to our study, a walked distance bellow 440 m can estimate reduced exercise capacity in CPET (VO2 <60%), which can be very useful in clinical practice, especially when patients are unable to cycle and/ or there is no access to laboratory exercise tests or to individualised exercise prescriptions in PR programs. Additional studies can further access the accuracy and utility of our findings.
References
- Singh D, Agusti A, Anzueto A, Barnes PJ, Bourbeau J, et al. (2019) Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Lung Disease: the GOLD science committee report 2019. Eur Respir J 53: 1900164.
- Jones P, Miravitlles M, van der Molen T, Kulich K (2012) Beyond FEV(1) in COPD: a review of patient-reported outcomes and their measurement. Int J Chron Obstruct Pulmon Dis 7: 697-709.
- Calverley PMA (2006) Dynamic hyperinflation: is it worth measuring?. Proc Am Thorac Soc 3: 239-244.
- Garcia-Aymerich J, Lange P, Benet M, Schnohr P, Anto JM (2006) Regular physical activity reduces hospital admission and mortality in chronic obstructive pulmonary disease: a population based cohort study. Thorax 61: 772-778.
- Ambrosino N (1999) Field tests in pulmonary disease. Thorax 54: 191-193.
- Puente-Maestu L, Palange P, Casaburi R, Laveneziana P, Maltais F, et al. (2016) Use of exercise testing in the evaluation of interventional efficacy: an official ERS statement. Eur Respir J 47: 429-460.
- Agrawal MB, Awad NT (2015) Correlation between Six Minute Walk Test and Spirometry in Chronic Pulmonary Disease. J Clin Diagn Res 9: 1-4.
- Mak VH, Bugler JR, Roberts CM, Spiro SG (1993) Effect of arterial oxygen desaturation on six minute walk distance, perceived effort, and perceived breathlessness in patients with airflow limitation. Thorax 48: 33-38.
- Casanova C, Cote C, Marin JM, Pinto-Plata V, de Torres JP, et al. (2008) Distance and oxygen desaturation during the 6-min walk test as predictors of long-term mortality in patients with COPD. Chest 134: 746-752.
- Pinto-Plata VM, Cote C, Cabral H, Taylor J, Celli BR (2004) The 6-min walk distance: change over time and value as a predictor of survival in severe COPD. Eur Respir J 23: 28-33.
- Karanth MS, Awad NT (2017) Six Minute Walk Test: A Tool for Predicting Mortality in Chronic Pulmonary Diseases. J Clin Diagn Res 11: 34-38.
- Freitas CG, Pereira CA, Viegas CA (2007) Inspiratory capacity, exercise limitation, markers of severity, and prognostic factors in chronic obstructive pulmonary disease. J Bras Pneumol 33: 389-396.
- Perez T, Deslée G, Burgel PR, Caillaud D, Le Rouzic O, et al. (2019) Predictors in routine practice of 6-min walking distance and oxygen desaturation in patients with COPD: impact of comorbidities. Int J Chron Obstruct Pulmon Dis 14: 1399-13410.
- Chang CH, Lin HC, Yang CH, Gan ST, Huang CH, et al. (2020) Factors Associated with Exercise-Induced Desaturation in Patients with Chronic Obstructive Pulmonary Disease. Int J Chron Obstruct Pulmon Dis 15: 2643-2652.
- Ferrazza AM, Martolini D, Valli G, Palange P (2009) Cardiopulmonary Exercise Testing in the Functional and Prognostic Evaluation of Patients with Pulmonary Diseases. Respiration 77: 3-17.
- Boutou AK, Zafeiridis A, Pitsiou G, Dipla K, Kioumis I, et al. (2020) Cardiopulmonary exercise testing in chronic obstructive pulmonary disease: An update on its clinical value and applications. Clin Physiol Funct Imaging 40: 197-206.
- Cote CG, Pinto-Plata V, Kasprzyk K, Dordelly LJ, Celli BR (2007) The 6-min walk distance, peak oxygen uptake, and mortality in COPD. Chest 132: 1778-1785.
- Stringer W, Marciniuk D (2018) The Role of Cardiopulmonary Exercise Testing (CPET) in Pulmonary Rehabilitation (PR) of Chronic Obstructive Pulmonary Disease (COPD) Patients. Copd 15: 621-631.
- Turner SE, Eastwood PR, Cecins NM, Hillman DR, Jenkins SC (2004) Physiologic Responses to Incremental and Self-Paced Exercise in COPD: A Comparison of Three Tests. Chest 126: 766-773.
- Poulain M, Durand F, Palomba B, Ceugniet F, Desplan J, et al. (2003) 6-minute walk testing is more sensitive than maximal incremental cycle testing for detecting oxygen desaturation in patients with COPD. Chest 123: 1401-1407.
- Gupta R, Ruppel GL, Espiritu JRD (2020) Exercise-Induced Oxygen Desaturation during the 6-Minute Walk Test. Med Sci (Basel) 8: 8.
- Kirkham AA, Pauhl KE, Elliott RM, Scott JA, Doria SC, et al. (2015) Utility of Equations to Estimate Peak Oxygen Uptake and Work Rate From a 6-Minute Walk Test in Patients With COPD in a Clinical Setting. J Cardiopulm Rehabil Prev 35: 431-438.
- Culver BH, Graham BL, Coates AL, Wanger J, Berry CE, et al. (2017) Recommendations for a Standardized Pulmonary Function Report. An Official American Thoracic Society Technical Statement. Am J Respir Crit Care Med 196: 1463-1472.
- Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, et al. (2005) Standardisation of spirometry. Eur Respir J 26: 319-338.
- Stocks J, Godfrey S, Beardsmore C, Bar-Yishay E, Castile R (2001) Plethysmographic measurements of lung volume and airway resistance. ERS/ATS Task Force on Standards for Infant Respiratory Function Testing. European Respiratory Society/ American Thoracic Society. Eur Respir J 17: 302-312.
- Graham BL, Brusasco V, Burgos F, Cooper BG, Jensen R, et al. (2017) 2017 ERS/ATS standards for single-breath carbon monoxide uptake in the lung. Eur Respir J 49: 1600016.
- American Thoracic Society; American College of Chest Physicians (2003) ATS/ACCP statement on cardiopulmonary exercise testing. Am J Respir Crit Care Med 167: 211-277.
- Ross RM (2003) ATS/ACCP statement on cardiopulmonary exercise testing. Am J Respir Crit Care Med 167: 1451.
- Sue DY, Hansen JE (1984) Normal values in adults during exercise testing. Clin Chest Med 5: 89-98.
- Palange P, Ward SA, Carlsen KH, Casaburi R, Gallagher CG, et al. (2007) Recommendations on the use of exercise testing in clinical practice. Eur Respir J 29: 185-209.
- ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories (2002) ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med 166: 111-117.
- Erratum (2016) ATS Statement: Guidelines for the Six-Minute Walk Test. Am J Respir Crit Care Med 193: 1185.
- Holland AE, Spruit MA, Troosters T, Puhan MA, Pepin V, et al. (2014) An official European Respiratory Society/American Thoracic Society technical standard: field walking tests in chronic respiratory disease. Eur Respir J 44: 1428-1446.
- Oliveira MJ, Marcoa R, Moutinho J, Oliveira P, Ladeira I, et al. (2018) Reference equations for the 6-minute walk distance in healthy Portuguese subjects 18-70 years old. Pulmonology.
- Wedzicha JA (1999) Domiciliary oxygen therapy services: clinical guidelines and advice for prescribers. Summary of a report of the Royal College of Physicians. J R Coll Physicians Lond 33: 445-447.
- Holland AE, Spruit MA, Troosters T, Puhan MA, Pepin V, et al. (2014) An official European Respiratory Society/American Thoracic Society technical standard: field walking tests in chronic respiratory disease. Eur Respir J 44: 1428-1446.
- Sava F, Laviolette L, Bernard S, Breton MJ, Bourbeau J, et al. (2010) The impact of obesity on walking and cycling performance and response to pulmonary rehabilitation in COPD. BMC Pulm Med 10: 55.
- Vonbank K, Marzluf B, Knotig M, Funk GC (2020) Agreement between Cardiopulmonary Exercise Test and Modified 6-Min Walk Test in Determining Oxygen Uptake in COPD Patients with Different Severity Stages. Respiration 99: 225-230.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Ladeira I, Oliveira P, Martins C, Ricardo Lima MD, Guimarães M (2022) What is the Agreement Between 6MWD And CPET Performance in COPD? J Card Pulm Rehabi 6: 169. DOI: 10.4172/jcpr.1000169
Copyright: © 2022 Ladeira I, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 2603
- [From(publication date): 0-2022 - Apr 29, 2025]
- Breakdown by view type
- HTML page views: 2163
- PDF downloads: 440