Short Communication Open Access
Venous Neurovascular Pathways to Neuroinflammation in Neurodegenerative Disorders
Tsamopoulos NG1*, Kalodimou VE2 and Sakka P31Mediterraneo Hospital, Department of Interventional Neuroradiology, Athens, Greece
2Department of Flow Cytometry Research & Regenerative Medicine, IASO Maternity & Research Hospital, Athens, Greece
3AKTIOS Alzheimer Unit Athens, Athens Association of Alzheimer’s disease and Related Disorders, Greece
- *Corresponding Author:
- Tsamopoulos NG
Mediterraneo Hospital
Department of Interventional Neuroradiology
Greece
Tel: 302109117010, 306974445011
E-mail: tsamopoulos@gmail.com
Received date: September 15, 2014; Accepted date: September 26, 2014; Published date: September 28, 2014
Citation: Tsamopoulos NG, Kalodimou VE, Sakka P (2014) Venous Neurovascular Pathways to Neuroinflammation in Neurodegenerative Disorders. Microinflammation 1:112. doi: 10.4172/2381-8727.1000112
Copyright: © 2014 Tsamopoulos NG, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at International Journal of Inflammation, Cancer and Integrative Therapy
Alois Alzheimer first notice in 1907 that the disease that bears his name could be caused by micro vascular changes. Neuroinflammation, has been considered as a hallmark of Alzheimer’s disease. The presence of anatomic or functional central nervous system’s venous stenosis, leads, to actual or functional capillary venous hypertension due to reflected pressure waves. This results in dysfunction of tight junctions, perivenous edema and compromised blood-brain-barrier (BBB) function, affecting parenchymal homeostasis, causing astrocyte and oligodendrocyte dysfunction and perpetuating neurodegeneration. Increased filtration pressure due to venous hypertension and intravascular fluid and protein leakage due to BBB breakdown can lead to increases in interstitial fluid (ISF). Lymphatic drainage of the Central Nervous System (CNS) regulates the balance of ISF and solutes within the CNS microenvironment and represents an accessory route through which excess fluid and proteins can flow from the interstitial spaces back into the blood. Also, plays an important role in neuroimmunological reactions, through physiological drainage of antigens from the brain to regional lymph nodes, mostly cervical and lumbar. In other words, altered lymph flow due to increased production or decreased outflow may affect both neuronal milieu and immune response. The molecular basis of the link between Neurovascular change and Neurodegenerative disorders may determine future therapeutic approaches [1].
In the theoretical framework the presence of anatomic or functional central nervous system’s impaired venous drainage leads to actual or functional capillary venous hypertension also due to reflected pressure waves. This results in dysfunction of tight junctions, perivenous edema and compromised BBB function, affecting parenchymal homeostasis and causing astrocyte and oligodendrocyte dysfunction. Increased filtration pressure due to venous hypertension and intravascular fluid and protein leakage due to BBB breakdown can lead to increases in interstitial fluid (ISF). Any factor that increases interstitial fluid also increases lymph flow [2]. Lymphatic drainage of the CNS regulates the balance of ISF and solutes within the CNS microenvironment and represents an accessory route through which excess fluid and proteins can flow from the interstitial spaces back into the blood. It also plays an important role in neuroimmunological reactions through physiological drainage of antigens from the brain to regional lymph nodes, mostly cervical and lumbar [3]. In other words, altered lymph flow due to increased production or decreased outflow may affect both neuronal milieu and immune response.
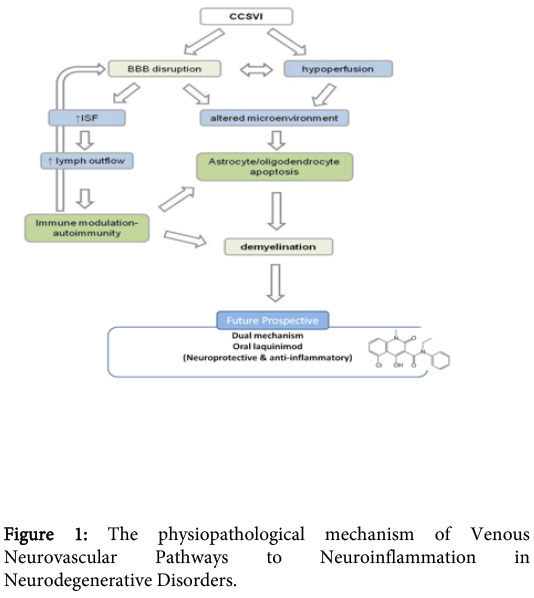
•The physiopathological mechanism has as follow (Figure 1).
•Abnormal neurovascular outflow creates localized increase in intravascular pressure at the venous and of the capillary bed (local hypertension) which provokes rupture of endothelial tight junctions and BBB breakdown [4]. Increased venous capillary pressure lead to Hypo perfusion and virtual Hypoxia [5].
•Increased filtration pressure due to venous hypertension and intravascular fluid and protein leakage due to BBB breakdown can lead to increases in interstitial fluid.
•Any factor that increases interstitial fluid also increases lymph flow [6].
•Fraction of CSF drains through the cribriform plate into the nasal submucosa and ultimately to cervical lymph nodes [7].
•NMO-IgG target the protein aquaporin 4 in the cell membranes of astrocytes which acts as a channel for the transport of water across the cell membrane. Aquaporin 4 is found in the processes of the astrocytes that surround the blood–brain barrier [8].
•BBB break down+Hypoperfusion lead to significant changes in neuronal microenvironment, increased ISF and lymph production, local activation of the inflammatory cascade, iron deposition, oligodentrocyte loss, attraction of phagocytes , demyelination and eventually plaque formation [9].
In conclusion the treatment of venous abnormalities would attenuate this process by alleviating venous hypertension and BBB damage. Thus, a combined haemodynamic-immune paradigm of central nervous system’s venous insufficiency emerges, which may explain its potential role in neurodegenerative diseases, such as Alzheimer’s disease and provide a theoretical framework for future research. The decreased perfusion pressure would also result in decreased ISF and lymph production and ultimately in decreased antigen transport and presentation to regional lymph nodes. The closing remarks in this short commentary is that a combined haemodynamic-immune paradigm of CNS insufficiency emerges, which may have a role in Neurodegenerative disorders, such as Alzheimer’s disease and provide a theoretical framework for future research.
References
- De la Torre JC (2005) Is Alzheimer's disease preceded by neurodegeneration or cerebral hypoperfusion?Ann Neurol 57: 783-784.
- Guyton AC, Hall JE (2006) Textbook of medical physiology. 11th ed. Philadelphia: Elsevier Saunders 192.
- Weller RO, Djuanda E, Yow HY, Carare RO (2009) Lymphatic drainage of the brain and the pathophysiology of neurological disease.ActaNeuropathol 117: 1-14.
- Talbert DG (2008) Raised venous pressure as a factor in multiple sclerosis.Med Hypotheses 70: 1112-1117.
- Tucker TW (2011) A physics link between venous stenosis and multiple sclerosis.Med Hypotheses 77: 1074-1078.
- Guyton AC, Hall JE (2006) Textbook of medical physiology. 11th ed. Philadelphia: Elsevier Saunders 192.
- Johnston M, Zakharov A, Papaiconomou C, Salmasi G, Armstrong D (2004) Evidence of connections between cerebrospinal fluid and nasal lymphatic vessels in humans, non-human primates and other mammalian species.Cerebrospinal Fluid Res 1: 2.
- Wingerchuk DM (2006) Neuromyelitisoptica.Int MS J 13: 42-50.
- Talbert DG (2008) Raised venous pressure as a factor in multiple sclerosis. Med Hypotheses 70: 1112-1117.
Relevant Topics
Recommended Journals
- Journal of Lung Cancer Diagnosis & Treatment
- Advances in Cancer Prevention
- Breast Cancer: Current Research
- Cancer Surgery
- Immunology: Current Research
- Current Trend in Gynecologic Oncology
- Journal of Cancer Diagnosis
- Journal of Gastrointestinal Cancer and Stromal Tumors
- Cervical Cancer: Open Access
- Journal of Mucosal Immunology Research
- Journal of Oncology Research and Treatment
- Journal of Orthopedic Oncology
- Journal of Prostate Cancer
- Research and Reviews on Pathogens
Article Tools
Article Usage
- Total views: 14702
- [From(publication date):
September-2014 - Apr 05, 2025] - Breakdown by view type
- HTML page views : 10114
- PDF downloads : 4588