Review Article Open Access
Vector Control Interventions to Prevent Dengue: Current Situation and Strategies for Future Improvements to Management of Aedes in India
Amarjeet Singh1 and Andrew W Taylor-Robinson2*1School of Pharmaceutical Sciences, Lovely Professional University, Jalandhar, Punjab 144411, India
2School of Health, Medical and Applied Sciences, Central Queensland University, Brisbane, QLD 4000, Australia
- *Corresponding Author:
- Andrew W Taylor-Robinson
Infectious Diseases Research Group, School of Health, Medical and Applied Sciences
Central Queensland University, 160 Ann Street, Brisbane, QLD 4000, Australia
Tel: +61 7 3295 1185
E-mail: a.taylor-robinson@cqu.edu.au
Received date: January 25, 2017; Accepted date: February 09, 2017; Published date: February 20, 2017
Citation: Singh A, Taylor-Robinson AW (2017) Vector Control Interventions to Prevent Dengue: Current Situation and Strategies for Future Improvements to Management of Aedes in India. J Emerg Infect Dis 2:123. doi: 10.4172/2472-4998.1000123
Copyright: © 2017 Singh A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Infectious Disease and Pathology
Abstract
Dengue is the most widespread vector-borne infectious disease of humans, existing in around 125 tropical and subtropical countries worldwide. The causative agent, a Flavirus, is transmitted from one person to another by female mosquitoes of the genus Aedes, primarily Ae. aegypti and Ae. albopictus, which breed in small, still bodies of freshwater such as storage tanks, buckets, plant pots and discarded household waste. Encouraging progress has been made in recent years towards the diagnosis and timely management of this debilitating and sometimes fatal disease. However, in the absence of an antiviral therapy or vaccine that is available and affordable in a low income setting, the means to combat dengue currently rely upon vector control measures that are directed against the immature aquatic stages, larvae and pupae, or adult mosquitoes. Although a number of different methods are in use, vector control has failed to prevent outbreaks from occurring and to avert an expansion of the geographical distribution of dengue. This is due to several limitations of present technologies that relate to dwindling financial resources, development of insecticide resistance, failure of long term sustainability and insufficient community involvement. In this context, there is a pressing need for an evidence-based selection process to determine how best to detect and exterminate the breeding of Aedes mosquitoes. This review considers existing vector control strategies as well as discussing some of the novel approaches that are in preparation, placing particular emphasis on relevance to the worsening public health issue of dengue endemicity in India.
Keywords
Dengue; Aedes; Mosquito; Vector; Control; Prevention; Intervention; India
Introduction
Dengue is one of the major human pathogens belonging to the family Flaviviridae, which also includes other arthropod-borne (arbo) viruses that cause yellow fever, Japanese encephalitis, West Nile encephalitis and Zika fever. From an epidemiological perspective, dengue is the most rapidly spreading vector-transmitted disease globally [1,2]. Over the last fifty years the incidence of dengue has increased approximately 30-fold [3]. Today, more than 2.5 billion people in the tropics and subtropics are at risk of infection [4], and there are an estimated 390 million dengue infections annually in approaching 130 nations and territories worldwide [5]. Estimates of the global incidence range between 200-400 million clinical cases per annum [3]. In India, since the first outbreak occurred in 1963 in Calcutta, now Kolkata, dengue has been also reported from most other regions of the country [6-8]. For 2016, 27 of 35 states and union territories reported the clinical incidence of dengue [9].
Clinical manifestations
Dengue infections can be asymptomatic or may develop into one of three traditionally recognized clinical manifestations; dengue fever, dengue haemorrhagic fever (DHF) or dengue shock syndrome (DSS) [10,11]. The World Health Organization (WHO) and the Special Programme for Research and Training in Tropical Diseases (TDR) recently revised the guidelines for dengue case classification. Clinical infection may be categorized as: mild self-limiting illness; dengue with a wide range of warning signs (abdominal pain, persistent vomiting, fluid accumulation, mucosal bleeding, lethargy, increasing haematocrit with decreasing platelets); or severe dengue (dengue with severe plasma leakage, severe bleeding, or organ failure) [1].
Dengue virus serotypes, immunity and immunopathology
There are four closely related, antigenically distinct serotypes (DENV-1 to DENV-4) of enveloped, positive sense, single-stranded RNA virus of the genus Flavivirus, the aetiological agent that causes dengue infections [10-12]. The existence of a fifth distinct serotype was mooted recently, although its recognition remains to be ratified [13]. Infection with one serotype confers life-long immunity to the exposed serotype but will provide only transient protection against others [14-16]. Secondary infection with a heterotypic serotype generates crossreactive antibodies, which, when present in the peripheral circulation, increase the potential risk of antibody-dependent enhancement of disease, a form of immunopathology. Hence, recurrent infection is the major risk factor for the serious, often fatal, complications of DHF and DSS. Infants who are immunized passively via receipt of maternal antibodies from a dengue pre-immune mother are at high risk of severe dengue infection [17,18]. Different dengue serotypes vary in their capacity to cause severe illness, but there is no expert consensus as to the extent of a causal association [19]. Multiple serotypes are in circulation in India [20].
Vector identification, behaviour and distribution
The dengue virus is transmitted between humans primarily by Aedes aegypti and Ae. albopictus [21]. These mosquito species typically bite at dawn and dusk but may do so at any time of day throughout the year [22]. By preference, female mosquitoes lay their eggs in artificial containers like flower vases, old automobile tyres, upturned buckets, and also in poorly disposed waste such as used metal cans [23]. Ae. aegypti displays a peridomestic habit and is the dominant vector mosquito species in urban areas, whereas Ae. albopictus is found more in semi-urban and rural environments [24]. The distribution of Ae. albopictus has expanded rapidly [25], and this species is a potential vector in areas where Ae. aegypti is not established. The principal factors which contribute to the spread of dengue in India include rapid and unplanned urbanization, human population growth, inadequate municipal services, and increased use of non-biodegradable household products [3]. All these determinants promote the establishment of Aedes mosquitoes in habitats in which they come into intimate proximity to many millions of Indian citizens.
Dengue control strategies
Currently, there exists no specific therapy that is marketed for dengue, such as antiviral drugs or vaccination [26], placing a reliance on supportive treatments for symptoms, including oral rehydration, administration of intravenous fluids and/or blood transfusion. Significant progress in vaccine development during the last decade has led to the regulatory authority approval of the first product in 2016 [27]. However, its cost may prevent widespread use in developing countries, [28,29] where control of the mosquito vector will remain the most effective measure to combat dengue [30]. As such, the Partnership for Dengue Control, a unique global alliance of international health agencies created in 2013 to spearhead an integrated approach to sustainably control and prevent dengue, recommends health communities to continue to rely on vector control even when an effective dengue vaccine does become commercially available, since the two approaches should complement and enhance the effectiveness of one another [31]. Existing vector control strategies include environmental management and chemical or biological interventions.
Here, the current scenario of vector control in India is considered and a range of measures for possible future improvements is discussed.
Vector Control Strategies
The aim of vector control strategies is to prevent transmission of virus by controlling mosquito vectors and interrupting human-vector contact [32]. A number of strategies has been developed, several of which have proved effective in various situations in different countries. Although each of these methods has been found to control dengue to a certain extent, in order to eradicate completely disease transmission it is envisaged that to be successful a control programme must integrate a combination of appropriate measures [11].
Environmental management
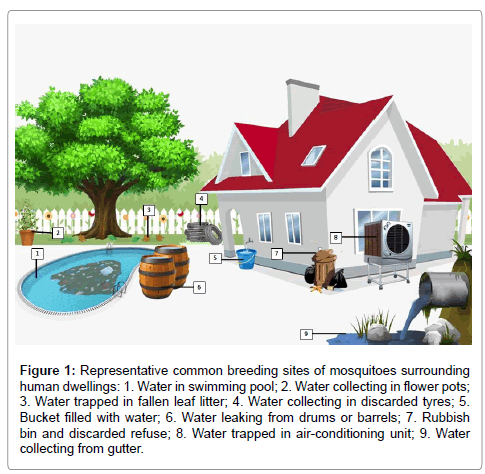
This is the most effective measure of vector control and includes prevention and reduction of vector propagation and human-vector contact by destruction, alteration, disposal or recycling of containers and natural larval habitats which produce the greatest number of adult mosquitoes [33,34]. Peridomestic sites in which mosquitoes are commonly observed to breed are indicated in Figure 1.
Figure 1: Representative common breeding sites of mosquitoes surrounding human dwellings: 1. Water in swimming pool; 2. Water collecting in flower pots; 3. Water trapped in fallen leaf litter; 4. Water collecting in discarded tyres; 5. Bucket filled with water; 6. Water leaking from drums or barrels; 7. Rubbish bin and discarded refuse; 8. Water trapped in air-conditioning unit; 9. Water collecting from gutter.
Reducing vector habitats/breeding sites–use of water storage containers, such as drums, overhead tanks and jars should be avoided or, if unavoidable, they should be covered with tightly fitting lids or screens [34]. Using polystyrene beads in water tanks also aids control of mosquito breeding by preventing mosquitoes from laying eggs on the surface [35].
Solid waste management–solid waste refers to non-biodegradable items of household, community and industrial waste [34]. Accumulation of water in such solid wastes promotes breeding of dengue vectors; hence, the proper storage, collection and disposal of waste are essential for safeguarding public health [36]. Solid waste such as discarded tyres, bottles, and cans should be recycled on a regular basis [34].
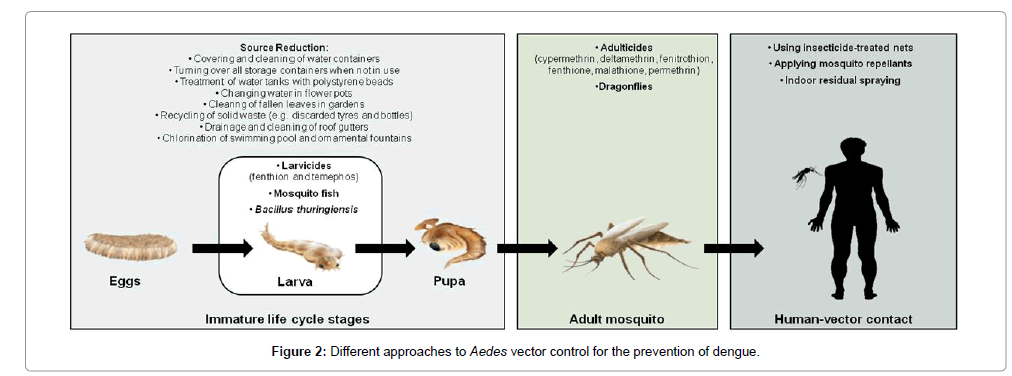
Modification of man-made breeding sites–improvement to house designs in order to reduce entry of mosquitoes, drainage and cleaning of roof gutters, outdoor sinks and condensate collection units under refrigerators and air-conditioners, and chlorination of ornamental pool or fountains are some of the habitat management measures which minimize the risk of the breeding of mosquitoes near human dwellings [34]. Figure 2 shows the various approaches which can be undertaken as a means of vector control.
Biological control
Biological control measures exploit the innate behaviour of a living creature in order to limit the population size of a targeted vector species. Such natural enemies of mosquitoes include predators, parasitoids and pathogens [37].
Predators–feed on mosquitoes, e.g. dragonflies and damselflies (known colloquially in India as ‘mosquito hawks’), frogs, toads and their tadpoles (such as the spade foot toad, green tree frog and giant tree frog), birds (notably swallows, martins and swifts, ducks and other waterfowl), fish (including goldfish, guppies, bass, bluegill and catfish). The most effective fish predator of mosquito larvae is Gambusia affinis (commonly called the ‘mosquito fish’) [37].
Parasitoids–are organisms the larval-like juvenile stage of which lives as a parasite inside a host mosquito before destroying it. A prime example is the protozoan Ascogregarina culicis, a parasite of Ae. aegypti larvae, that adversely affects the mosquito population [37]. Another bacterial parasite, Wolbachia pipientis, has been demonstrated to reduce the life span of Ae. aegypti under laboratory conditions [38].
Pathogens–of mosquitoes include viruses, bacteria, fungi and protozoa. Infection of mosquitoes with these pathogens decreases their rates of growth and feeding on humans, checks their reproduction, and even kill or seriously disable them [37]. Examples of such pathogens include: spores of entomopathogenic fungi (such as Beauveria bassiana and Metarhizium anisopliae), which affect larval and adult stages of mosquitoes [39]; Csp_P, a bacterium of the genus Chromobacterium that resides in the mosquito midgut and which reduces the survival of both larvae and adults [40]; and Bacillus thuringiensis H-14 (Bti), a mosquito larvicide that is commercially available under a number of trade names [34].
Chemical control
Chemical control is the application of natural or synthetic compounds that possess insecticidal properties in order to reduce the mosquito population within the local environment. These are available as larvicides (applied directly to water to control larvae), adulticides (used in wide-area fogging and spraying to combat adult mosquitoes) and synergists (not toxic in themselves but able to increase the efficiency of other administered chemicals) [41]. Examples of insecticides that have been deployed worldwide include organophosphates (e.g. fenitrothion, fenthione malathione) and pyrethroids (e.g. cypermethrin, deltamethrin, permethrin) [42].
Integrated vector management
Integrated vector management (IVM) is a rational decision-making process for the optimal use of resources for vector control [43]. This approach was first promoted in 2004 by the WHO with the aim of making vector control more efficient, cost-effective, ecologically sound and sustainable. According to the WHO, planning and implementation of vector control involves analyzing the local determinants of disease, assessing requirements and resources, and designing locally appropriate implementation strategies at a national level [43]. The five key elements of an IVM strategy are: i) advocacy, social mobilization and legislation; ii) collaboration within the health sector and with other sectors; iii) an integrated approach; iv) evidence-based decision making; and v) capacity building [44]. Effective dengue control activities require collaboration between agencies involved in strategic planning, project development and operational management, and their productive partnership with other stakeholders in promoting a community-based control programme [45].
Dengue in India
Ongoing challenges
Under the Directorate General of Health Services, Ministry of Health and Family Welfare, Government of India, the National Vector Borne Disease Control Programme (NVBDCP) is the central nodal agency for implementation of activities for prevention and control of vector-borne diseases across the country. These include the protozoan diseases malaria and kala-azar (visceral leishmaniasis), the nematode infection lymphatic filariasis (elephantiasis), as well as several arboviruses, notably dengue, yellow fever, Japanese encephalitis, chikungunya and Zika [46].
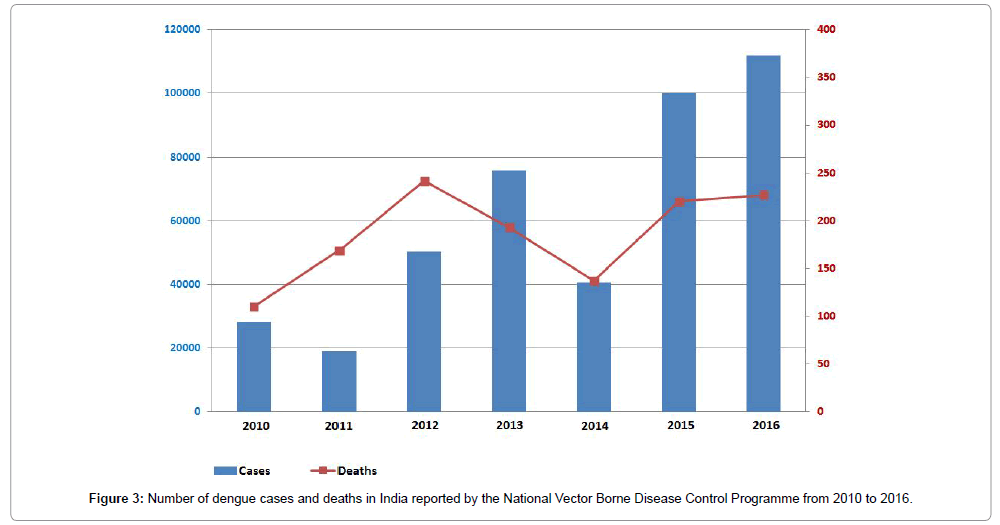
The NVBDCP is making extensive efforts to develop a suite of effective dengue control measures. Despite this programme the number of dengue cases, their severity and geographical distribution are escalating, as evidenced by the frequent outbreaks and re-emergence of dengue in several parts of the country. Disease is prevalent throughout India in most of the metropolitan cities and towns. Outbreaks have also been reported from rural areas of Haryana, Karnataka and Maharashtra [46]. Based on national statistics released by the NVBDCP, the last decade has witnessed a pronounced upward trend in the overall incidence of dengue, as represented since 2010 in Figure 3. The provisional total number of dengue cases reported in 2016 was 111,880, which resulted in 227 deaths [9].
The sustainable control of dengue vectors is recognized as an arduous task [47]. The significant challenges for vector control programmes include dwindling financial resources, development of insecticide resistance, failure of long term sustainability, lack of community involvement, and limited public knowledge regarding dengue transmission and prevention [48].
Historical control measures
In the early part of the twentieth century eliminating mosquito breeding grounds by drainage or poisoning with either the copper arsenite compound Paris green or pyrethrum, a naturally occurring Chrysanthemum-derived pyrethrin, was sometimes successful. While previous frequent use was also made of larvicides to combat mosquitoes in India, following the widespread introduction of the organochlorine insecticide dichlorodiphenyltrichloroethane (DDT) in the 1950s vector control became heavily dependent upon DDT spraying [49]. Once it was recognized as a persistent environmental pollutant and likely human carcinogen, by the 1990s DDT was banned in most developed countries but it remains available as an agricultural pesticide on the Indian subcontinent. However, as a consequence of extensive mosquito resistance, its application as a means of vector control is discouraged and has diminished considerably. Where DDT is still used it is applied not to crops but to the inside walls of houses to kill or repel mosquitoes, a practice now approved by the WHO in regions where malaria and dengue are of profound concern to public health. This intervention, called indoor residual spraying (IRS), greatly reduces environmental damage and the incidence of resistance to DDT and other pesticides used [50,51].
Current detection measures
Since 2007, the NVBDCP has facilitated the diagnosis and clinical data collection for cases of dengue. Under the programme, 347 sentinel surveillance hospitals and 14 apex referral laboratories have been set up throughout the India. These are supplied with anti-dengue IgM capture ELISA test kits as a means of rapid detection by the National Institute of Virology located in Pune [52].
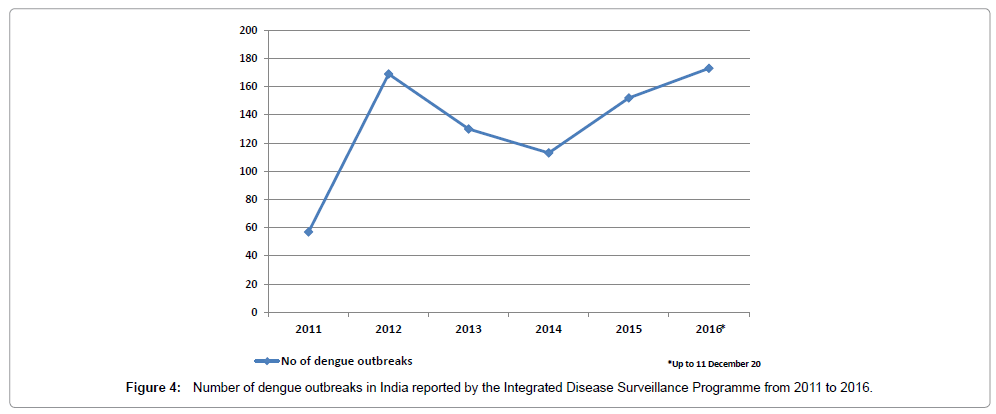
In order to strengthen disease detection across the country, an integrated disease surveillance programme (IDSP) was launched in 2004 to both detect and respond to disease outbreaks rapidly [53]. All disease outbreaks reported at a state level are compiled in the form of a Weekly Outbreak Report that is available on the IDSP website [54]. Figure 4 shows the national number of dengue outbreaks reported recently under the IDSP [55].
Current control measures
The present day approach to vector control implemented by the NVBDCP is interdisciplinary and includes a blend of components under a policy of IVM. These include: larvicides (such as the organophosphate temephos); source reduction engaging minor engineering methods (clearing the margins around large bodies of water, de-weeding to ensure proper flow of water, closing off or filling in small repositories in which water temporarily collects); IRS, insecticide-treated nets (ITNs), adulticides, and measures for reducing human-vector contact [49].
The effect on the control of Ae. aegypti of implementing community-based eco-health measures has been examined in Chennai (formerly Madras) in eastern India [56]. This study revealed that environmentally friendly vector control methods like covering water containers, solid waste management and urban ‘clean-up’ campaigns involving women’s groups and school children led to a substantial reduction in the density of dengue vectors. These findings suggest a way to optimize dengue vector control through an inclusive and translational approach that engages the local community as a partner in the control programme.
The combined factors of rainfall and power supply have a major influence on the spread of dengue [57]. Specifically, both poor rainfall and limited power supply prompt people to collect water in storage containers at times when electricity is available, thereby providing a man-made peridomestic habitat for Aedes to breed. Improved community education is called for in the furtherance of reducing this contemporary cause of dengue vector spread. To date, very few studies have been conducted to evaluate the cause and effect of variables on the frequent dengue outbreaks in different regions of India [20].
Future Perspectives
Dengue is among the most important public health problems that faces India today. With a view to minimizing the impact of any dengue outbreak that may occur, state and federal governments should strengthen their vector control programmes. Moreover, strategies to increase the degree of active participation of the general public are desirable [45,58,59].
Integrated vector management
Using multiple vector control methods simultaneously can help to reduce disease transmission to a very low level as compared to a single intervention [48]. This is evident from the evaluation of IVM as the most effective dengue vector control intervention, among several determined, in reducing entomological parameters (breteau index, container index and house index) [21]. Furthermore, instead of using multiple vector control measures for a single infectious disease, government ministries and health agencies should target multiple mosquito-borne diseases utilizing the same interventions and infrastructure. This will increase the cost effectiveness of the vector control programme.
Novel vector control methods
The technological advancement of emerging vector control tools for large-scale deployment and to long-lasting effect progresses continuously. The RNAi-based release of insects carrying a dominant lethality (RIDL) system for mass rearing of male mosquitoes has been developed, a technique which involves injection of a lethal gene into mosquito eggs [60]. Integration of the lethal gene into the mosquito genome leads to formation of many toxic metabolites in the larva, causing either its death or sterility. Another pioneering study reported the ωMelPop-CLA strain of Wolbachia as an effective agent for preventing dengue transmission by causing cytoplasmic incompatibility, reducing the life span of Ae. aegypti and, in so doing, interfering with viral transmission [61]. Only older mosquitoes transmit the dengue virus, so this is predicted to reduce transmission. Over just a few generations, the bacterium is able to spread, infected mosquitoes replace the wild population, and reduce their reproductive capability. Both RIDL and Wolbachia are potentially powerful weapons in the fight against dengue, but their further development and field trial testing will require the overcoming of policy and regulatory barriers as well as cross-border collaboration among scientists, politicians and communities.
Conclusions
In a bid to arrest the upsurge of dengue in India in recent times rather than to focus primarily on patient-centred, curative and medicine-intensive disease management, approaches to improve environmental health and to manage vector habitats should be prioritized. Dengue vector control is an effective tool in reducing Aedes mosquito populations, particularly when control strategies utilize a community-based and integrated approach, combined with educational programmes to increase knowledge, awareness, attitudes and practices of people in the local community.
While it is apparent that in India IVM has been implemented by NVBDCP as an ongoing vector control measure over the last decade as yet there has not been a follow-up survey to assess the relative success of its implementation. It would be worthwhile to conduct such studies in order to determine the current status of IVM and to identify challenges to implementation in both urban and rural areas of India. Monitoring and evaluation are integral to every aspect of the programme and critical to its success.
Taking a holistic perspective, for effective management of dengue, the coordinated and multidisciplinary efforts of different government departments with regard to sanitation, urban development and education are essential. Moreover, local communities must be engaged to take active responsibility for their own protection by supporting elimination of Aedes breeding sites and taking personal measures towards prevention of infection, such as use of mosquito repellents.
Conflict of Interest
The authors declare that they have no competing issues of interest.
Acknowledgements
- Nathan MB, Dayal-Drager R, Guzman M (2009) Epidemiology, burden of disease and transmission. In: Dengue: Guidelines for Diagnosis, Treatment, Prevention and Control. World Health Organization and the Special Programme for Research and Training in Tropical Diseases, Geneva 3-21.
- Guha-Sapir D, Schimmer B (2005) Dengue fever: new paradigms for a changing epidemiology. Emerg Themes Epidemiol 2: 1.
- Gyawali N, Bradbury RS, Taylor-Robinson AW (2016) The epidemiology of dengue infection: harnessing past experience and current knowledge to support implementation of future control strategies. J Vector Borne Dis 53: 293-304.
- Bhatt S, Gething PW, Brady OJ, Messina JP, Farlow AW, et al. (2013) The global distribution and burden of dengue. Nature 496: 504-507.
- Higa Y (2011) Dengue vectors and their spatial distribution. Trop Med Health 39: 17.
- Tewari SC, Thenmozhi V, Katholi CR, Manavalan R, Munirathinam A, et al. (2004) Dengue vector prevalence and virus infection in a rural area in south India. Trop Med Int Health 9: 499-507.
- Victor TJ, Malathi M, Asokan R, Padmanaban P (2007) Laboratory-based dengue fever surveillance in Tamil Nadu, India. Ind J Med Res 126: 112-115.
- Roop K, Priya S, Sunita P, Mujib M, Kanhekar LJ, et al. (2016) Way forward for seasonal planning of vector control of Aedes aegypti and Aedes albopictus in a highly dengue endemic area in India. Austin J Infect Dis 3: 1022.
- National Vector Borne Disease Control Programme (2016) Dengue Cases and Deaths in the Country since 2010.
- Burke DS, Monath TP (2001) Flavivirus. In: Field Virology, 4th edn. Lippincott Williams & Wilkins, Philadelphia 852-921.
- Malavige GN, Fernando S, Fernando DJ, Seneviratne SL (2004) Dengue viral infections. Postgrad Med J 80: 588-601.
- Gubler DJ, Clark GG (1995) Dengue/dengue hemorrhagic fever: the emergence of a global health problem. Emerg Infect Dis 1: 55-57.
- Taylor-Robinson AW (2016) A putative fifth serotype of dengue – potential implications for diagnosis, therapy and vaccine design. Int J Clin Med Microbiol 1: 101-102.
- Leitmeyer KC, Vaughn DW, Watts DM, Salas R, Chacon IV, et al. (1999) Dengue virus structural differences that correlate with pathogenesis. J Virol 73: 4738-4747.
- Young PR, Hilditch PA, Bletchly C, Halloran W (2000) An antigen capture enzyme-linked immunosorbent assay reveals high levels of dengue virus protein NS1 in the sera of infected patients. J Clin Microbiol 38: 1053-1057.
- Alcon S, Talarmin A, Debruyne M, Falconar A, Deubel V, et al. (2002) Enzyme-linked immunosorbent assay specific to dengue virus type 1 nonstructural protein NS1 reveals circulation of the antigen in the blood during the acute phase of disease in patients experiencing primary or secondary infections. J Clin Microbiol 40: 376-381.
- Beltramello M, Williams KL, Simmons CP, Macagno A, Simonelli L, et al. (2010) The human immune response to Dengue virus is dominated by highly cross-reactive antibodies endowed with neutralizing and enhancing activity. Cell Host Microbe 8: 271-283.
- Wahala WMPB, de Silva AM (2011) The human antibody response to dengue virus infection. Viruses 3: 2374-2395.
- Endy TP (2002) Epidemiology of inapparent and symptomatic acute dengue virus infection: a prospective study of primary school children in Kamphaeng Phet, Thailand. Am J Epidemiol 156: 40-51.
- Barnett LJ, Taylor-Robinson AW (2016) Vigilance to limit the bidirectional introduction and co-circulation of virus serotypes aims to reduce risk of severe dengue disease in North East India. J Emerg Infect Dis 1: 1000115.
- Erlanger TE, Keiser J, Utzinger J (2008) Effect of dengue vector control interventions on entomological parameters in developing countries: a systematic review and meta-analysis. Med Vet Entomol 22: 203-221.
- Islam R, Salahuddin M, Ayubi MS, Hossain T, Majumder A, et al. (2015) Dengue epidemiology and pathogenesis: images of the future viewed through a mirror of the past. Virol Sin 30: 326-343.
- Getachew D, Tekie H, Gebre-Michael T, Balkew M, Mesfin A (2015) Breeding sites of Aedes aegypti: potential dengue vectors in Dire Dawa, East Ethiopia. Interdiscip Perspect Infect Dis 2015: 706276.
- Dutta P, Mahanta J (2006) Potential vectors of dengue and the profile of dengue in the north-eastern region of India: an epidemiological perspective. Dengue Bull 30: 234-242.
- Lambrechts L, Scott TW, Gubler DJ (2010) Consequences of the expanding global distribution of Aedes albopictus for dengue virus transmission. PLoS Negl Trop Dis 4: e646.
- Ansari S, Taylor-Robinson AW (2014) Strategic approaches to multivalent vaccine development against dengue virus infection. Ann Vaccine Immuniz 1: 1005.
- Kirkpatrick BD, Whitehead SS, Pierce KK, Tibery CM, Grier PL, et al. (2016) The live attenuated dengue vaccine TV003 elicits complete protection against dengue in a human challenge model. Sci Transl Med 8: 330.
- Halstead SB (2016) Licensed dengue vaccine: public health conundrum and scientific challenge. Am J Trop Med Hyg 95: 741-745.
- Harapan H, Fajar JK, Sasmono RT, Kuch U (2016) Dengue vaccine acceptance and willingness to pay. Hum Vaccin Immunother 1: 1-5.
- Kroeger A, Lenhart A, Ochoa M, Villegas E, Levy M, et al. (2006) Effective control of dengue vectors with curtains and water container covers treated with insecticide in Mexico and Venezuela: cluster randomised trials. Brit Med J 332: 1247-1252.
- Achee NL, Gould F, Perkins TA, Reiner RC, Morrison AC, et al. (2015) A critical assessment of vector control for dengue prevention. PLoS Negl Trop Dis 9: e0003655.
- World Health Organization (2017) Dengue Control.
- Rozendaal JA (1997) Vector Control: Methods for Use by Individuals and Communities. World Health Organization, Geneva 412.
- World Health Organization (1997) Vector Surveillance and Control. In: Dengue Haemorrhagic Fever: Diagnosis, Treatment, Prevention and Control, WHO, Geneva, 48-59.
- Sivagnaname N, Amalraj DD, Mariappan T (2005) Utility of expanded polystyrene (EPS) beads in the control of vector-borne diseases. Indian J Med Res 122: 291-296.
- Dutta P, Khan S, Khan AM, Mahanta J (1999) Solid waste pollution and breeding potential of dengue vectors in an urban and industrial environment of Assam. J Environ Biol 20: 343-345.
- Sarwar M (2015) Reducing dengue fever through biological control of disease carrier Aedes mosquitoes (Diptera: Culicidae). Int J Prev Med Res 1: 161-166.
- McMeniman CJ, Lane RV, Cass BN, Fong AW, Sidhu M, et al. (2009) Stable introduction of a life-shortening Wolbachia infection into the mosquito Aedes aegypti. Science 323: 141-144.
- Scholte EJ, Knols BG, Samson RA, Takken W (2004) Entomopathogenic fungi for mosquito control: a review. J Insect Sci 4: 19.
- Ramirez JL, Short SM, Bahia AC, Saraiva RG, Dong Y, et al. (2014) Chromobacterium Csp_P reduces malaria and dengue infection in vector mosquitoes and has entomopathogenic and in vitro anti-pathogen activities. PLoS Pathog 10: e1004398.
- National Pesticide Information Center (2017) Pesticides Used in Mosquito Control
- Manjarres-Suarez A, Olivero-Verbel J (2013) Chemical control of Aedes aegypti: a historical perspective. Rev Costarr Salud Pública 22: 68-75.
- World Health Organization (2012) Handbook for Integrated Vector Management. WHO, Geneva, 68.
- Chanda E, Govere JM, Macdonald MB, Lako RL, Haque U, et al. (2013) Integrated vector management: a critical strategy for combating vector-borne diseases in South Sudan. Malar J 12: 369.
- Chang MS, Christophel EM, Gopinath D, Abdur RM (2011) Challenges and future perspective for dengue vector control in the Western Pacific Region. Western Pac Surveill Response J 2: 9-16.
- National Vector Borne Disease Control Programme (2017) Government of India Initiatives for Dengue and Chikungunya.
- Sivagnaname N, Gunasekaran K (2012) Need for an efficient adult trap for the surveillance of dengue vectors. Indian J Med Res 136: 739-749.
- Golding N, Wilson AL, Moyes CL, Cano J, Pigott DM, et al. (2015) Integrating vector control across diseases. BMC Med 13: 249.
- Srivastava PK, Sharma RS, Sharma SN, Singh S, Das Gupta RK, et al. (2014) Integrated vector management: policy and implementation under National Vector Borne Disease Control Programme, India. J Commun Dis 46: 46-50.
- Sy O, Cisse B, Tairou F, Diallo A, Ba E, et al. (2015) Acceptability of indoor residual spraying in the Central-Western of Senegal. Bull Soc Pathol Exot 108: 213-217.
- Paredes-Esquivel C, Lenhart A, del Río R, Leza MM, Estrugo M, et al. (2016) The impact of indoor residual spraying of deltamethrin on dengue vector populations in the Peruvian Amazon. Acta Trop 154: 139-144.
- Cecilia D (2014) Current status of dengue and chikungunya in India. WHO South-East Asia J Public Health 3: 22-28.
- National Centre for Disease Control (2017) Integrated Disease Surveillance Programme (IDSP).
- Integrated Disease Surveillance Programme (2017a) Weekly Outbreak Surveillance, 20 January.
- Integrated Disease Surveillance Programme (2017b) State/Disease Wise Compiled Outbreaks Reported Under IDSP.
- Arunachalam N, Tyagi BK, Samuel M, Krishnamoorthi R, Manavalan R, et al. (2012) Community-based control of Aedes aegypti by adoption of eco-health methods in Chennai City, India. Pathog Glob Health 106: 488-496.
- Chandran R, Azeez PA (2015) Outbreak of dengue in Tamil Nadu, India. Curr Science 109: 171-176.
- Gupta N, Srivastava S, Jain A, Chaturvedi UC (2012) Dengue in India. Indian J Med Res 136: 373-390.
- Gyawali N, Bradbury RS, Taylor-Robinson AW (2016) Knowledge, attitude and recommendations for practice regarding dengue among the resident population of Queensland, Australia. Asian Pac J Trop Biomed 6: 360-366.
- Alphey L, Nimmo D, O'Connell S, Alphey N. (2008) Insect population suppression using engineered insects. Adv Exp Med Biol 627: 93-103.
- Yeap HL, Mee P, Walker T, Weeks AR, O'Neill SL, et al. (2011) Dynamics of the ‘‘popcorn’’ Wolbachia infection in outbred Aedes aegypti informs prospects for mosquito vector control. Genetics 187: 583-595.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 17518
- [From(publication date):
March-2017 - Apr 06, 2025] - Breakdown by view type
- HTML page views : 15812
- PDF downloads : 1706