Case Report Open Access
Vancomycin Induced Neutropenia Associated with Fever: A Case Report
Adila Shaukat*, Muna Al Maslamani and Sumaira Rafiqui
Hamad Medical Corp Medicine- infectious diseases, Alwakra hospital, Doha, Qatar
- *Corresponding Author:
- Adila Shaukat
Hamad Medical Corp Medicine- infectious diseases
Alwakra hospital, Doha, Qatar
Tel: 00974-55408323
E-mail: Akashaf1@hamad.qa
Received date: September 26, 2017; Accepted date: October 06, 2017; Published date: October 10, 2017
Citation: Shaukat A, Maslamani M Al, Rafiqui S (2017) Vancomycin Induced Neutropenia Associated with Fever: A Case Report. J Infect Dis Ther 5:336. doi: 10.4172/2332-0877.1000336
Copyright: © 2017 Shaukat A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Infectious Diseases & Therapy
Abstract
Vancomycin-induced neutropenia is an uncommon but potentially serious side effect of prolonged vancomycin therapy. We present a case of a 19 year old male with disseminated methicillin-resistant Staphylococcus aureus (MRSA) Infection who was treated with IV vancomycin and developed fever and neutropenia. After discontinuation of IV vancomycin and substitution with clindamycin, both fever and neutropenia resolved within 72 h. Diagnosis of vancomycin-induced neutropenia and fever was considered as there was no alternative cause of this. In addition, quick resolution of fever and neutropenia upon removal of causative drug further supported the diagnosis. Since vancomycin is widely used in clinical practice, this adverse effect should be monitored carefully. Many studies report immune mediated mechanism to be the cause of this adverse effect. However, further studies need to be done in this regard to establish the exact mechanism.
Keywords
Vancomycin; Neutropenia; Fever; Adverse effect; Antibiotic
Introduction
Vancomycin is a bactericidal glycopeptide antibiotic in the use since 1958 [1-3]. It exhibits mainly gram-positive activity ,clinically used against methicillin resistant strain of coagulase positive and coagulase-negative Staphylococci and resistant enterococci [1,4].There are several reported cases of vancomycin-induced neutropenia over past 5 decades [5-16].However, only few case reports mentioned concomitant drug-induced fever [11-16].We are reporting an interesting case of vancomycin-induced neutropenia and fever where fever and neutropenia was quickly resolved within 72 h upon discontinuation of vancomycin.
Case summary
19 years old Pakistani boy with no comorbid condition presented to emergency department of our hospital with history of fever for 3 days duration associated with bilateral shoulder pain and generalized body ache. He was found to have right axillary abscess and perianal abscess and was admitted .Incision and drainage of axillary and perianal abscesses were done and he was started on ceftriaxone. Blood cultures and fluid culture from aspirated abscesses were sent. Blood and pus culture grew MRSA, sensitive to vancomycin, trimethoprim sulfamethoxazole, clindamycin and rifampicin. Infectious disease team was consulted and antibiotics were changed to IV vancomycin 1 g every 8 h. Later dose was increased 1.5 g every 8 h according to vancomycin trough level with the target range of 15-20 mcg/ml.
Patient was complaining of persistent pleuritic chest pain, but no other respiratory symptoms like cough or shortness of breath. Chest x-ray showed suspicious airspace opacities in both lower zones in retro-diaphragmatic region. CT thorax was done that showed multilocular right chest wall collection with enhancing walls suggesting abscesses. Bilateral basal consolidation, multiple pulmonary/subpleural airspace nodules suggesting septic emboli. Working diagnosis of disseminated MRSA infection (bacteremia, septic pulmonary emboli with pneumonia and skin and soft tissue infection) was made. Infectious disease physician recommended doing echocardiography to rule out infective endocarditis. However, transesophageal echocardiography did not show any evidence of endocarditis. It was decided to treat him as possible infective endocarditis (meets 1 major (Staphylococcus aureus bacteremia) and 2 minor (fever, septic emboli) criteria).
On day 3 of admission, patient complained of left sternoclavicular joint pain. On examination joint was tender and hot showing signs of inflammation. Septic arthritis of left sternoclavicular joint was suspected and MRI was done that showed features suggestive of osteitis of left clavicle with infective arthritis of sternoclavicular joint. Orthopedic team was consulted and they advised for conservative treatment with appropriate antibiotics.
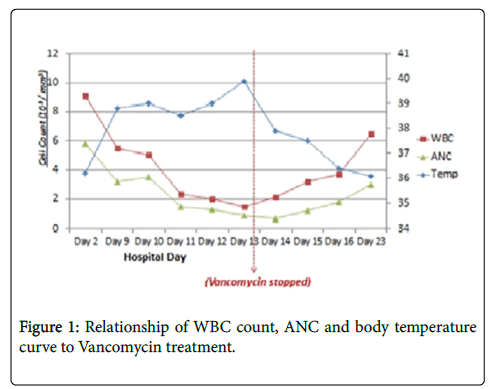
Repeated blood cultures were negative, fever subsided. Inflammation markers were decreasing. He was continued on vancomycin IV with plan to continue for total 6 weeks. On day 9 of admission, he started to have fever with T maximum 39°C. No other associated symptoms apart from feeling fatigue. The sternoclavicular joint was mildly tender with improvement in the pain. WBC was 5. Blood cultures were repeated. As there was no obvious cause of fever, patient was symptomatically managed. On day 13 patients developed drop in white blood cell 1.5 with neutropenia ANC 0.9. Repeated blood culture showed coagulase-negative Staphylococcus, most likely contamination. Urinalysis was unremarkable. EBV/adeno/CMV viral PCR was negative. Febrile neutropenia secondary to vancomycin was a possibility so antibiotics were changed to clindamycin and rifampicin. On the day 2 after changing antibiotics fever subsided and white blood cell count started to rise, reaching 3.7 with ANC 1.8 after 72 h of stopping vancomycin.
Patient stayed in the hospital for 2 more days on IV clindamycin and was discharged in good general condition on oral clindamycin 450 mg every 8 h for 2 more weeks. He was followed in infectious disease clinic after 2 weeks and found to have full recovery without further fever or neutropenia. Antibiotics were stopped. Upon follow-up visit after 3 months he stayed well and was discharged from infectious disease clinic.
Discussion
Neutropenia is recognized but rare adverse effect related to prolonged use of vancomycin, occurring at minimum of 7 days up to 20 days after initiation of treatment [5-7]. In addition to delayed onset, it is reported as reversible [13], resolves spontaneously upon stopping the drug within few days, however recovery can be prolonged in hemodialysis patients [8,9].
Therapeutic options for patients who need continuation of treatment after developing this side effect are not clear [9]. Usually selection of appropriate antimicrobial with similar spectrum of coverage or according to sensitivity pattern of the culture is practiced.
Koo et al. stopped vancomycin for 1 week and reinitiated with lower dose to complete the duration of therapy but vancomycin at lower dose was given for only 5 days [10]. However this approach is not practical to use for prolonged treatment with vancomycin as neutropenia can recur after reinitiation of antibiotic and on the other hand, using lower than the recommended dose of vancomycin can induce resistance/ treatment failure.Lai et al used Granulocyte Colony Stimulating Factor (GCSF) along with vancomycin to maintain neutrophil count in 2 patients [11].
Stephen et al. substituted vancomycin with teicoplanin and the neutropenia resolved [9].
Association of vancomycin-induced neutropenia with fever is described in only few case report [1,12-16]. The clinical pattern of vancomycin-induced fever coincides with vancomycin-induced neutropenia, typically starts after 7 days or more of treatment and resolves within 48-72 h of discontinuation of therapy [13]. Our patient had onset of fever at day 7 on IV vancomycin treatment while neutropenia appeared at day 13. Time of onset is consistent with other reported cases (Figure 1).
Mechanism for vancomycin introduced neutropenia and fever is unclear [9,11]. Multiple theories suggest immunological basis with IgG or IgM immune mediated hypersensitivity reaction [11,13]. It was supported by anti-granulocyte antibody positivity in serum of the patient with vancomycin-induced neutropenia as described by Michael D. Schwartz [7]. It is postulated that drug or other metabolite first binds to host protein to form drug protein complex that acts as an antigen. Antibodies are formed against that antigen and antigen antibody immune complex mediated complement activation, leads to destruction of neutrophils. It leads to neutropenia and as a result of this process lymphocytes are sensitized and pyrogenic substances are released leading to fever [7,14].
Incidence of vancomycin-induced neutropenia is reported as around 2% in literature [12,13]. There is no direct correlation of vancomycin-induced neutropenia and therapeutic serum drug concentration or total cumulative dosing [1,7,13]. Our patient had vancomycin trough level in therapeutic range throughout the treatment period.
It is advisable to monitor CBC including differential count at least once weekly for the patients taking vancomycin longer than 7 days duration [1] as neutropenia can be a serious adverse effect leading to morbidity and mortality.
Although, unfortunately no bone marrow biopsy or antineutrophil antibody testing was done in our patient but appearance of fever followed by neutropenia after completion of 7 days of IV vancomycin while patient was clinically responding and rapid reversibility upon stopping vancomycin makes it likely that neutropenia and fever was induced by vancomycin .In addition, there was no alternative cause of these symptoms and patient was not taking any other confounding medicine apart from paracetamol when necessary for fever and pain (Table 1).
| Exam/Day | On admission | Day 1 of vancomycin | D6 | D9 | D13 | D1 of discontinuation of vancomycin | D2 of discontinuation of vancomycin | D3 of discontinuation of vancomycin | D15 of discontinuation of vancomycin |
|---|---|---|---|---|---|---|---|---|---|
| White Blood cells | 25.6 | 15.4 | 9.1 | 5.5 | 1.5 | 2.1 | 3.2 | 3.7 | 6.5 |
| Neutrophil | 22.7 | 10.5 | 5.8 | 3.2 | 0.9 | 0.7 | 1.2 | 1.8 | 3 |
| Lymphocyte | 1.7 | 2.9 | 1.8 | 1.2 | 0.4 | 1.1 | 1.5 | 1.3 | 2.3 |
| Eosinophil | 0 | 0.8 | 0.7 | 0.4 | 0.2 | 0.1 | 0.2 | 0.1 | 0.6 |
| Hb | 9.8 | 9.5 | 9.1 | 10 | 9.5 | 10 | 9.8 | 10 | 10.8 |
| Platelet | 472 | 684 | 616 | 393 | 166 | 185 | 202 | 240 | 238 |
| CRP | 285 | 107 | 37 | 35 | 76 | 63 | <5 | ||
| Procalcitonin | 1 | ||||||||
| ESR | 77 | 105 | 67 | 74 | 10 |
Table 1: Impact of vancomycin treatment on Complete blood count and inflammatory markers.
Conclusion
Vancomycin-induced neutropenia and fever is potentially serious adverse effect for patients receiving prolonged vancomycin treatment. So clinicians must carefully observe the patients for neutropenia and fever if vancomycin treatment is longer than 1 week. Many studies report immune mediated mechanism to be the cause of these phenomena. However, further studies need to be done in this regard to establish the exact mechanism.
References
- Nailor, Sobel (2009) Antibiotics for gram-positive bacterial infections: vancomycin, teicoplanin, quinupristin/dalfopristin, oxazolidinones, daptomycin, dalbavancin, and telavancin. Infect Dis Clin North Am. 23: 965-982.
- Elting LS, Rubenstein EB, Kurtin D, Kenneth R, Fangtang J, et al. (1998) Mississippi mud in the 1990s: risks and outcomes of vancomycin-associated toxicity in general oncology practice. Cancer 83: 2597-2607.
- Deborah LH, Ray C, Dmitri VD, Joey L, Terry W, et al. (2005) Telavancin, a multifunctional lipoglycopeptide, disrupts both cell wall synthesis and cell membrane integrity in methicillin-resistant Staphylococcus aureus. Antimicrob Agents Chemother 49: 1127-1134.
- Crozier JA, Swaika A, Vendrell N, Laura Finn (2015) Vancomycin Induced Neutropenia: A Case Report. J Clin Case Rep 5:1.
- Black E, Lau TT, Ensom MH (2011) Vancomycin-Induced Neutropenia: Is it Dose- or Duration-Related? Ann Pharmacother 5: 629-638.
- R L Mackett, D R Guay (1985) Vancomycin-induced neutropenia. Can Med Assoc J 132: 39–40.
- Henry K, Steinberg I, Crossley KB (1986) Vancomycin-induced neutropenia during treatment of osteomyelitis in an outpatient. Drug intelligence and clinical pharmacy 20: 783-785.
- Mandl DL, Garrison MW, Palpant SD (1997) Agranulocytosis induced by vancomycin or ticarcillin/clavulanate. Ann Pharmacother 31: 1321-1323.
- Sanche SE, Dust WN, Shevchuk YM (2000) Vancomycin-Induced Neutropenia Resolves after Substitution with Teicoplanin. Clin Infect Dis 3: 824–825.
- KB Koo, RL Bachand, AW Chow (1986) Vancomycin-induced neutropenia. Drug intelligence & clinical pharmacy.
- KK Lai, J Kleinjan, P Belliveau (1996) Vancomycin-induced neutropenia treated with granulocyte colony-stimulating factor during home intravenous infusion therapy. Clin Infect Dis 23: 844-845.
- Schwartz MD (2002) Vancomycin-induced neutropenia in a patient positive for an antineutrophil antibody. Pharmacotherapy 22: 783-788.
- Smith PF, Taylor CT (1999) Vancomycin-induced neutropenia associated with fever: similarities between two immune mediated drug reactions. Pharmacotherapy 19: 240-244.
- Mackowiak PA (1987) Southwestern internal medicine conference. Drug fever: mechanisms, maxims and misconceptions. Am J Med Sci 294: 275–286.
- Shahar A (2000) Fever, rash, and pancytopenia following vancomycin rechallenge in the presence of ceftazidime. Ann Pharmacother 34:263–264.
- Strikas R, Studlo J, Venezio FR, O’Keefe JP (1982) Vancomycin induced neutropenia [letter]. J Infect Dis 146: 575.
Relevant Topics
- Advanced Therapies
- Chicken Pox
- Ciprofloxacin
- Colon Infection
- Conjunctivitis
- Herpes Virus
- HIV and AIDS Research
- Human Papilloma Virus
- Infection
- Infection in Blood
- Infections Prevention
- Infectious Diseases in Children
- Influenza
- Liver Diseases
- Respiratory Tract Infections
- T Cell Lymphomatic Virus
- Treatment for Infectious Diseases
- Viral Encephalitis
- Yeast Infection
Recommended Journals
Article Tools
Article Usage
- Total views: 8022
- [From(publication date):
October-2017 - Nov 23, 2024] - Breakdown by view type
- HTML page views : 7303
- PDF downloads : 719