Value of C-Reactive Protein Determination in Cerebrospinal Fluid in Childhood Infective Meningitis
Received: 01-May-2023 / Manuscript No. nnp-23-98609 / Editor assigned: 03-May-2023 / PreQC No. nnp-23-98609 / Reviewed: 17-May-2023 / QC No. nnp-23-98609 / Revised: 19-May-2023 / Manuscript No. nnp-23-98609 / Published Date: 26-May-2023 DOI: 10.4172/2572-4983.1000313
Abstract
A prospective study to determine the value of C-reactive protein concentrations in cerebrospinal fluid to differentiate between acute bacterial, partially treated bacterial, aseptic & tubercular meningitis was performed in 51 consecutively observed patients (children), who underwent lumbar puncture due to suspected infective meningitis. Diagnosis included acute or presumed bacterial meningitis (n=11), acute or presumed viral meningitis (n=13), partially treated bacterial meningitis (n=6), tubercular meningitis (n=2) and control group (n=19).The sensitivity, specificity, predictive values and optimum cut-off levels of C-RP in CSF were determined to diagnose these various types of infective meningitis. Determination of C-RP in CSF is a useful additional test on CSF examination in distinguishing between bacterial and aseptic meningitis. CSF-CRP levels>1.3mg/dl is highly suggestive of acute bacterial meningitis.
Keywords
Meningitis; C-reactive protein (CRP); Cerebrospinal fluid (CSF)
Introduction
Meningitis is a significant cause of mortality and morbidity in infancy & childhood. The etiological diagnosis of meningitis remains a problem in clinical practice, as CSF biochemical analysis and cellular response often overlap and CSF gram staining and culture which is the gold standard for determining the causative organism has low positivity especially in developing countries. Moreover culture reports are available after 48 hours. A diagnostic conundrum on the evaluation of children with suspected bacterial meningitis is the analysis of CSF obtained from children already receiving antibiotic therapy.
C-reactive protein (CRP) an acute phase inflammatory response marker is produced by hepatocytes in liver on stimulation by microbial infections and other inflammatory diseases.
The CRP in serum may gain access to CSF by passive diffusion across the highly inflamed meninges in infective meningitis. Several reports have shown an ability of CRP in CSF to discriminate between patients with bacterial meningitis and patients with aseptic meningitis. Nevertheless, a considerable controversy still exists about the actual clinical value of determination of CSF-CRP levels.
The literature reveals that the work done over last few decades on CRP estimation in CSF for distinguishing bacterial from aseptic meningitis is qualitative. Some quantitative studies done out side India have shown significant increase of CRP in CSF but none has derived any cut off level to diagnose bacterial meningitis.
Due to availability of new and advanced automated analysers over the past few years, it has been possible to do an accurate quantitative estimation of CRP in CSF and determine its cut-off levels to diagnose different types of infective meningitis.
Subjects and Methods
Clearance was obtained from the institutional ethical committee to conduct this study. The study protocol was fully explained to the parents/guardians, and informed written consent was obtained.
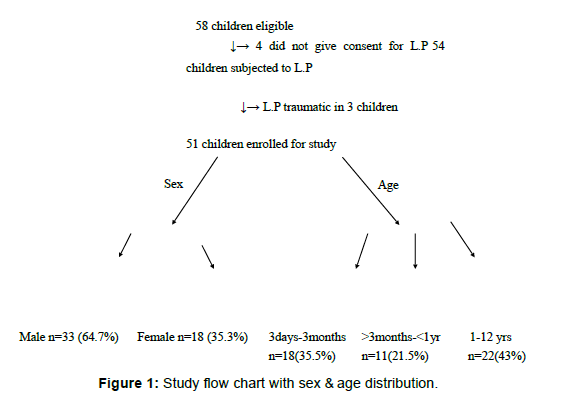
58 children in the age group of 3 days to 12 years admitted to the Pediatric Department of Yashoda Super Specialty Hospital Ghaziabad from April 2009 to April 2010 with clinical diagnosis of meningitis were eligible. However parents of 4 children did not give consent and in 3 cases lumbar puncture was traumatic. Remaining 51 children included in the study were further divided into 5 groups according to clinical, biochemical, cytological & bacteriological study of CSF (including PCR for herpes & tuberculosis), shown in (Figure 1).
Criteria for diagnosis of various types of meningitis on CSF examination were taken as follows: [1]
For bacterial meningitis: CSF- WBC count>100cells/cu.mm predominantly polymorphs; protein>45mg/ dl (>120mg/dl in neonates); CSF sugar<75% of serum sugar.
For aseptic meningitis: WBC count>5cells/cu.mm (>30 in neonates) predominantly monocytic/ lymphocytic; protein>45mg/dl (>120mg/dl in neonates), CSF sugar normal.
For tubercular meningitis: WBC count>10cells/cu.mm predominantly lymphocytic, protein>100mg/dl, CSF sugar<75% of serum sugar.
For partially treated bacterial meningitis: WBC count>5cells/ cu.mm (30cells in neonates) with predominance of polymorphs or ambiguous cytology, protein>100mg/dl, CSF sugar<75% of serum sugar.
Besides CSF exam, patients were subjected to other investigations like Hb, TLC, DLC, Platelet Count, Blood Culture, Montoux Test, Radiology (CXR, CT, MRI) wherever indicated to aid in diagnosis.
CRP estimation in CSF was done by a fully automated biochemistry analyzer Spectra-XL by Vital Scientific N.V. Netherlands and the reagent kit CRP – Turbilatex from Spinreact, S.A.V. Spain was used.
The principle of this analysis is that the latex particles coated with specific anti-human CRP are agglutinated when mixed with samples containing CRP. The agglutination causes an absorbance range, dependent upon the CRP contents of the patient’s sample. The reagent absorbance is analyzed by the analyzer based on photometric measurements.
Statistical analysis was done by using Mann-Whitney test (nonparametric) by comparing CRP levels in CSF in each group against the control i.e. ‘No CNS Infection’ group. P value < 0.05 was considered to be significant. Software used was SPSS of 16.0 versions.
Results
The median value and range of CRP concentrations in CSF were as given in (Table 1).
| Group Final diagnosis value(significant<0.05) | No.of (%) | cases CRP Median ( range) | levels | in | CSF(mg/dl) | P- | |
|---|---|---|---|---|---|---|---|
| I II III IV V |
Bacterial meningitis Aseptic meningitis Tubercular meningitis Partially treated bacterial meningitis No CNS Infection |
11(19.6) 13(21.6) 02(3.9) 06(11.8) 19(37.2) | 3.40 (1.0-7.7) 0.40 (0.2-2.0) 3.55 (2.8-4.3) 1.25 (0.8-2.2) 0.40 (0.1-1.1) | 0.000 0.209 0.022 0.002 | |||
Table 1: Group distribution & CSF-CRP levels in study groups.
It was observed that CRP levels rise significantly in bacterial meningitis as compared to the cases who were having normal CSF examination(control group), p=0.000. Significant rise was also seen in partially treated bacterial meningitis (p=0.002) and tubercular meningitis (p=0.022), however number of cases in tubercular meningitis was low (n=2).
There was no significant difference in CRP levels between aseptic meningitis group & control group. But significant CRP levels were seen in three cases of aseptic meningitis who were having brain parenchymal lesions documented by MRI (median value of 1.3mg/dl (range 1.0 – 2.0mg/dl, p=0.011).
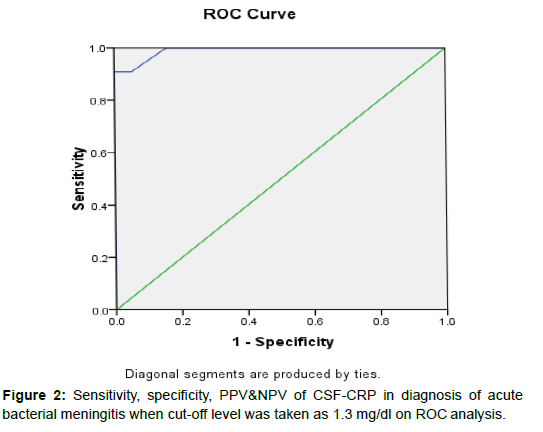
On ROC curve analyses, when optimum cut-off level of CSFCRP in bacterial meningitis was taken as 1.3mg/dl the sensitivity and specificity was 90.9% and 100% with a PPV and NPV of 100% & 95% respectively. The diagnostic accuracy determined by area under curve (AUC) was 99% (Figure 2).
Cut-off level Sensitivity Specificity PPV NPV of CSF-CRP1.3 mg/ dl 90.9% 100% 100% 95%.
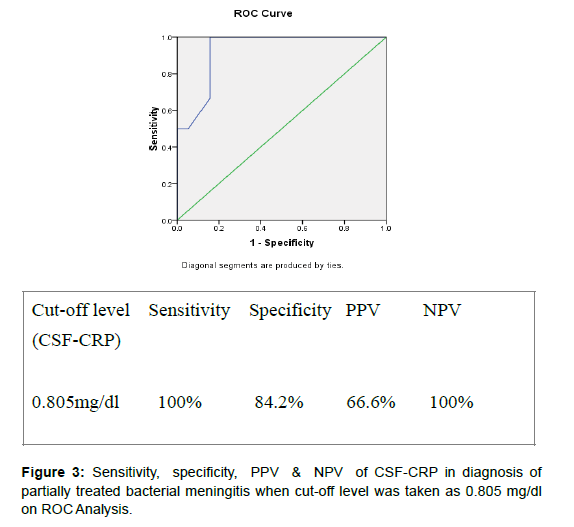
On taking optimum cut-off level of CSF-CRP as 0.805mg/dl in partially treated bacterial meningitis group the sensitivity & specificity of the test was 100% & 84.2% respectively with a PPV & NPV as 66.6%& 100% with a diagnostic accuracy(AUC) of 93% (Figure 3).
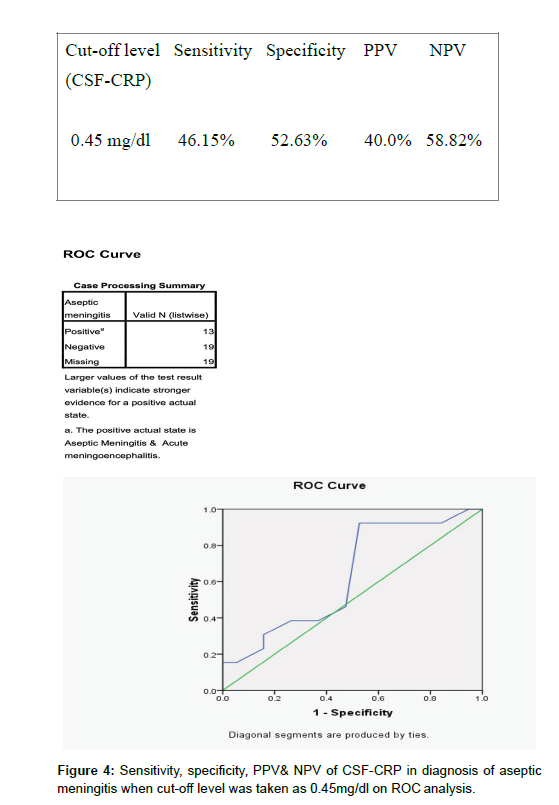
In case of Aseptic meningitis when optimum cut-off level of CSFCRP was taken as 0.45mg/dl,the sensitivity & specificity was 46.15% & 52.63% and PPV & NPV 40% & 58.8% respectively with a diagnostic accuracy of 63.2%.(Figure 4).
In view of low number of cases in tubercular meningitis ROC curve analyses was not done in this group.
Discussion
CSF culture and gram staining was positive in 18% cases (2 out of 11). Organisms isolated were strep. pneumoniae (n = 1) and staph aureus (n = 1).
Blood cultures was positive in 3 patients of partially treated bacterial meningitis (E. coli in 2 cases & pseudomonas in 1) and total leukocyte counts & differential counts were taken into consideration in the remaining 3 cases in support of CSF findings in this group to differentiate them from aseptic meningitis cases .PCR for Herpes was positive in 2 cases.
CSF culture positivity is low in our study as compared to that reported by various workers from India, which is around 30 – 60% [2]. One reason for low positivity in our study could be the use of human blood agar instead of sheep blood agar in our microbiology lab. Although S.pneumoiae, S.aureus, S.pyogenes grow on HuBA, the colony size tends to be very small, the morphology often varies from that present on animal blood agar, & hemolysis is minimal. As colony size, colony morphology & hemolysis are all critical to the identification of these organisms, there is a much greater chance that these organisms from human specimens cultured on HuBA will be overlooked or misidentified [3].
In our study we observed that CSF-CRP rises significantly in acute bacterial meningitis. Taking 1.3mg/dl of CRP in CSF as optimum cut-off level, we were able to diagnose acute bacterial meningitis with a sensitivity = 90.9%; specificity = 100%; PPV = 100% & NPV = 95%. CSFCRP rise was also significant in partially treated bacterial meningitis and tubercular meningitis. However the number of cases in tuberculous group was too low (n=2) to draw the conclusion. On taking optimum cut-off level of CSF-CRP in partially treated bacterial meningitis as 0.805mg/dl, sensitivity & specificity were 100% & 84.2% respectively.
It was noticed that CSF-CRP does not rise significantly in aseptic meningitis; however there was significant rise of CRP in CSF in cases that were having brain parenchymal lesion documented by radioimaging. The potential explanation for this observation could be local production of CRP in central nervous system by the affected tissues [4]. Based on these observations of our study, we conclude that CRP in CSF is a useful additional test for distinguishing between bacterial meningitis from aseptic meningitis. This is true even with prior antibiotic therapy.
CSF-CRP level > 1.3mg/dl is highly suggestive of bacterial meningitis [5]. However if CRP levels in CSF are raised significantly and other biochemical & cytological findings on CSF examination is suggestive of aseptic meningitis, then one should actively search for brain parenchymal lesion by doing neuro-imaging. Limitations of our study were small sample size, low culture positivity, less number of cases in tubercular meningitis group and despite taking into consideration of all evidences there might have been overlap of cases between aseptic and partially treated bacterial meningitis on the basis of CSF cytology & biochemistry [6].
Contributors
Concept and design of the study was provided by AP, which was carried out by KR. Data analysis and interpretation of results were done by KR and finally revised and approved by AP & AK. Laboratory assays were done by MC. The final manuscript was approved by all authors.
Funding
None
Competing Interests
None stated.
References
- Nelson textbook of pediatrics. CSF in central nervous system disorders; Lumbar puncture and cerebrospinal fluid examination. 2: 2440- 2441.
- Kumar L, Chitlengiya S, Ayyagiri A (1980) The current status of pyogenic meningitis in children. Indian Pediatr 17:438-440.
- FM Russell, SSN Biribo, G Selvaraj, F Oppedisano, JR Carapetis (2006) As a bacterial culture medium, citrated sheep blood agar is a practical alternative to citrated human blood agar in lab of developing countries. Clin Microbio 44(9): 3346-3351.
- Yasojima K, Schwab C, McGee (2000) Human neurons generate C-reactive protein & amyloid P: up regulation in Alzheimer disease. Brain Res 887: 80-89.
- Tillett WS, Fracis t Jr (1980) Serological reactions in pneumonia with a non-protein somatic fraction of pneumococcus. J. Exper. Med, 1980; 52: 561-571.
- Hanley JA, McNeil BJ (1982) The meaning and use of area under a receiver operating characteristic curve. Radiol 143: 29-36.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Raheja K, Rahim K, Prakash A, Dubey S, Arora R (2023) Value ofC-Reactive Protein Determination in Cerebrospinal Fluid in Childhood InfectiveMeningitis. Neonat Pediatr Med 9: 313. DOI: 10.4172/2572-4983.1000313
Copyright: © 2023 Raheja K, et al. This is an open-access article distributed underthe terms of the Creative Commons Attribution License, which permits unrestricteduse, distribution, and reproduction in any medium, provided the original author andsource are credited.
Share This Article
Recommended Conferences
42nd Global Conference on Nursing Care & Patient Safety
Toronto, CanadaRecommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 980
- [From(publication date): 0-2023 - Feb 01, 2025]
- Breakdown by view type
- HTML page views: 893
- PDF downloads: 87