Research Article Open Access
Validity of the Adult Needs and Strengths Assessment with Substance Abuse Populations
Robert Sky Allen1* and Bradley D Olson21Regional Mental Health Center, Indianapolis Boulevard, East Chicago, Indiana, USA
2Community Psychology program of National Louis University, Chicago, Illinois, USA
- Corresponding Author:
- Robert Sky Allen
3903 Indianapolis Boulevard
East Chicago, IN 46312
Tel: 219 201 7613
Fax: 219 392 6998
E-mail: skyallen@comcast.net
Received date: June 22, 2015 Accepted date: July 30, 2015 Published date: August 06, 2015
Citation: Allen RS, Olson BD (2015) Validity of the Adult Needs and Strengths Assessment with Substance Abuse Populations. J Addict Res Ther 6:235. doi:10.4172/2155-6105.1000235
Copyright: © 2015 Allen RS, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Addiction Research & Therapy
Abstract
Objective: The purpose of this study was to introduce a relatively new assessment tool, and to evaluate its validity as a clinical instrument of measurement and placement. The study examined the validity of the Adult Needs and Strengths Assessment (ANSA) as a standardized screening device in the treatment of substance use disorders. The authors analyzed the ANSA scores of 191 participants who were assigned to an episode of substance abuse treatment, focusing on the Level of Need algorithmic calculation of the ANSA, as well as three specific ANSA domains, including Substance Use Disorder, Criminal Behavior, and Community Connection. ANSA clinical scores were compared to scores from a self-report substance abuse survey.
Methods: It is important for therapists to know that the instruments of measurement they employ are documenting their clients’ perspective accurately. Therefore, analyses examined whether clinical assessments were capturing participants’ self-reported changes in substance-related outcomes. When a pilot study for this research revealed a positive correlation between the ANSA comprehensive clinical assessment and a brief substance abuse survey, the authors expanded the study to ascertain if other domains of the ANSA were correlated with the survey.
Results: Relationships were found between change scores on the ANSA and change scores on the survey selfreport, with the exception of the Community Connection domain which yielded no measurable relationship. As the study was intended to be a preliminary investigation of the ANSA, recommendations for further exploration of the ANSA’s algorithmic properties, as well as further research into other domains of the ANSA, were included.
Conclusion: Preliminary evidence suggests that the ANSA is a valid tool of measurement, and that it does reflect the client’s perspective accurately, thus strengthening confidence in its use as a standardized screening instrument.
Keywords
ANSA; Substance abuse; Substance use disorders; Substance abuse treatment; Validity; Screening; Assessment
Introduction
How researchers and practitioners measure substance use patterns can have a profound impact on treatment protocols. Throughout the United States and around the world, various agencies employ sundry intake devices to determine the severity of substance abuse patterns and related problems from both a recent and lifetime perspective. Some of the more commonly used measures include the Addiction Severity Index (ASI) from National Institutes of Health (NIH), Substance Abuse Subtle Screening Inventory (SASSI) from Multi-Health Systems (MHS), and the Simple Screening Instrument for Alcohol and Other Drugs (SSI-AOD) from the Center for Substance Abuse Treatment (CSAT).
In recent years, however, the Adult Needs and Strengths Assessment (ANSA) has become the preferred instrument for many providers of substance abuse treatment [1]. The ANSA was created to support decision-making in relation to level of care and service planning, facilitate quality improvement initiatives, and allow for monitoring of outcomes. The ANSA currently is being utilized in a number of locations within the United States and Canada, in such diverse settings as hospitals, emergency rooms, rehabilitation programs, and mental health centers.
The ANSA was developed to craft a linkage between the assessment process and the design of individualized service planning founded upon evidence-based practices. The original version, the Severity of Psychiatric Illness (SPI), was created in the 1990s to study decisionmaking in psychiatric emergency systems. The ANSA expanded on the concepts of the SPI to include a broader description of functioning and to incorporate strengths with a recovery focus.
Lyons [2] explains that the ANSA was devised to focus on six core principles of measurement design. First, each item on the assessment has implications for differential action. In other words, the ANSA is a planning process for what should happen next in service delivery. Second, levels of each item of the assessment are translatable into action. A standard four-point scale, ranging from “no need for action” to “intensive action is needed,” is used to guide decision-making. Third, the assessment attempts to prevent undue influence of contextual factors such as services already in place, cultural matters, and personal development. Fourth, measurement is descriptive, and attempts to minimize cause-and-effect assumptions in order to pursue persondriven planning. Fifth, observation windows are recommended, but exist only to remind users that ratings should be implemented with flexibility, and should remain fresh. Finally, the assessment is a strategy for information integration, which is to say that the ANSA combines multiple streams of information into a single measure, making it more rigorous than a single-source tool.
According to the Praed Foundation, the reliability index of the ANSA is 0.75 with vignettes, 0.86 with case records, and above 0.90 withclinical cases. Over the years, the ANSA has been tested by analyzing the relationship between ANSA scores and level of care decisions made by case managers and others pursuant to symptoms, risk behaviors, and functioning. For instance, Nelson and Johnston [3] examined ANSA scores for a group of 272 participants over a two-year period to assess whether the scoring system was useful in predicting clinical placement for psychiatric treatment. Analyses showed that 85.9% of original LON placements were classified correctly, supporting the supposition that the ANSA scoring system is a practical tool for decision-making.
With any type of treatment, it is important for therapists to know that the instruments of measurement they employ are reflecting their clients’ perspective accurately. Do the instruments satisfy validity and reliability standards? Are community considerations and cultural sensitivities taken into account? Do the instruments reflect the vision of the people receiving services? Does that vision convey the health and well-being of the whole person and not just the health and well-being of the person vis-à-vis presenting problems?
It can be challenging to expose individuals to substance abuse treatment and then look for evidence that their lives indeed have improved. In other words, evidence of change from the perspective of the client may be different from evidence of change from the perspective of the therapist. Sometimes in the realm of substance abuse treatment, it is difficult to discern the difference. As screening instruments such as the ANSA are based upon clinical ratings, this study seeks to examine available tools, as imperfect as they are, to determine if they accurately reflect the client’s perception of change.
Although the ANSA has some research to support its use by substance abuse treatment providers as an accurate tool for measuring change, there is limited evidence in the literature to support its validity. Therefore, a preliminary study was devised to examine the validity of the ANSA and to measure whether changes reported by participants in substance abuse treatment also were being documented accurately in clinical assessments. Expressly, the purpose of the study was to examine whether change in scores on a well-established, reliable survey were correlated with change in scores on the more recent ANSA instrument.
It was hypothesized that change in scores pretest versus posttest on the substance abuse screening instrument would be correlated positively with change in scores pretest versus posttest on the ANSA clinical assessments of psychosocial functioning. Specifically, it was hypothesized that self-reported change scores as per participants would be correlated positively with clinical assessments as per therapists with regard to level of need, substance use disorders, criminal behavior, and community connection.
Because males, in general, are more than five times as likely to have an alcohol problem, and two or three times as likely to have a drug problem as women [4], more males than females were expected to participate in the study. Also, because Biglan et al. [5] reported a 25.4% drop-out rate in their study of attrition in substance abuse research, some attrition was expected.
Methods
Participants
A convenience sample of 191 adults, 155 males and 36 females ranging in age from 19 to 63 with a mean age of 37 and median age of 35, agreed to participate in an outcome study conducted at a community mental health center on the outskirts of a major United States city. Participants in the study had been referred to substance abuse treatment by family members, physicians, schools, legal sources, employers, or via self-referral, though it should be noted that the majority of participants had been court-mandated to receive services. Participants came from all walks of life, from a variety of backgrounds, and were representative of their community of origin. The center was equipped to provide outpatient and inpatient substance abuse treatment, psychiatric services, and 24-hour access to emergency services, as well as an assortment of consultation and education programs.
Traditionally, males are known to comprise a greater proportion of the substance abuse population, and this study was no exception as males constituted 81% of the sample. Because the literature informs that men are much more likely to have a substance use disorder than women, the proportion of males in this study, therefore, was judged to be consistent with the population of interest.
Thirty-six percent of the participants were European American, 32% African American, and 32% Hispanic/Latino/Latina. Eighty percent of participants reported their marital status as not married, never married, divorced, separated, or widowed. Seventy-seven percent had a high school education or beyond, while over half (52%) were unemployed.
Participants in the study met with a certified therapist to receive the same 90-minute clinical assessment that all individuals seeking services at the center receive to determine their need, if any, for substance abuse treatment. The need was appraised according to diagnostic criteria developed by the American Psychiatric Association (2000) Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR) [6] defining a substance use disorder as a problematic pattern of substance use leading to clinically significant impairment or distress. Participants also were screened for presenting problems, physical and mental health status, risk behaviors, substance use disorders, and medication management issues.
The study received university Institutional Review Board (IRB) approval to ensure that ethical guidelines for conducting research with human participants were followed. Researchers and therapists alike adhered to clinical procedures for acquiring informed consent and protecting confidentiality. No incentives of any kind were offered other than the satisfaction of knowing that participation in the research could contribute to a better understanding of substance abuse treatment.
Instruments
As previously mentioned, participants in the study were assessed by a certified therapist, and were screened for presenting problems. They received a clinical assessment of psychosocial functioning as measured by the Adult Needs and Strengths Assessment. At the same time, they also were invited to complete a battery-style pretest survey derived from the Simple Screening Instrument for Alcohol and Other Drugs (SSIAOD) that asked seven dichotomous questions concerning the past six months. The questions were designed to create a snapshot evaluation such that any change from a positive response to a negative response indicated improvement. Spanish translation was available.
Adult Needs and Strengths Assessment (ANSA): Participants received an Adult Needs and Strengths Assessment based upon an indepth clinical interview. The ANSA employs a proprietary algorithm that calculates an ordered Level of Need (LON) score ranging from one to five, with one indicating less severe and five more severe psychosocial problems. These scores can change during treatment, and clients received an ANSA reassessment at least once every six months during the course of treatment, as well as a final assessment upon completion of treatment.
A pilot study for this research [7] involved 50 participants and focused exclusively on the LON score of the ANSA and self-reported substance use patterns. The LON was chosen because it is the fundamental metric of the clinical assessment, and the authors wanted to establish some confidence in its utility before proceeding with the study. Examining change scores, an analysis found a moderate positive correlation significant at the 0.05 level (r = 0.41, p < 0.05). That is to say, the analysis demonstrated that improvement of scores on a substance abuse survey was associated with improvement of scores on a clinical assessment of global functioning.
Following the pilot study, it was noted that three additional domains of the ANSA hold special interest for substance abuse treatment providers due to the potential direct and indirect relevance of these domains for treatment protocols, namely substance use disorders, criminal behavior, and community connection. The ANSA operationally defines substance use as the use of alcohol and other drugs, the misuse of prescription medications, and the inhalation of any substance. Criminal behavior is defined operationally as behavior and status offenses that may result from failing to follow required behavioral standards. And the operational definition of community connection encompasses involvement in the cultural aspects of life in the local community. The scores from these three domains not only contributed to participants’ overall ANSA LON appraisal, but were selected in the research for analysis.
Simple Screening Instrument for Alcohol and Other Drugs: In addition to the ANSA clinical assessment, substance abuse patterns were measured using a self-report survey known as the Simple Screening Instrument for Alcohol and Other Drugs (SSI-AOD) as developed by the Center for Substance Abuse Treatment (CSAT) [8] of the Substance Abuse and Mental Health Services Administration (SAMHSA) (see Appendix A). The SSI-AOD contains 16 dichotomous questions designed to screen for substance abuse problems occurring within the past six months. The SSI-AOD is in the public domain and for years has been a reliable tool for screening and assessment. Kills-Small, Simons, and Stricherz [9] evaluated the criterion validity of the SSI-AOD and found that the instrument correctly classified approximately 70% of the participants while demonstrating moderate to strong correlations with substance frequency, consumption, and problem indices.
For the purposes of this study, the instrument was modified to include only seven questions derived from the DSM-IV-TR criteria for diagnosing a substance use disorder. Although there is no known precedent for doing so, some questions were excluded from the original instrument because they were thought to be self-evident (i.e., have you gone to anyone for help because of your drinking or drug use?), beyond the scope of treatment (i.e., have you had any health problems?), or unrelated to the DSM-IV-TR criteria (i.e., have any of your family members ever had a drinking or drug problem?). The questions on the survey were as follows:
During the past six months. . .
• Have you used alcohol or other drugs?
• Have you been unsuccessful in trying to cut down or quit drinking or using drugs?
• Has drinking or other drug use caused problems between you and your family or friends?
• Have you been arrested or had other legal problems?
• Have you lost your temper or gotten into arguments or fights while drinking or using other drugs?
• Do you spend a lot of time thinking about or trying to get alcohol or other drugs?
• Do you feel bad or guilty about your drinking or other drug problem?
Scores from the adapted SSI-AOD were cross-referenced with ANSA scores, and were used not only to inform clinical placement decisions, but also to assess changes in substance use patterns over the course of treatment. Within the first 90 days subsequent to discharge, an attempt was made by a team of psychology interns and therapists to contact participants. Those participants who stayed through the duration of their scheduled treatment episode and were available to be contacted following discharge were invited to complete a posttest battery with the same seven questions as were asked on the pretest.
Design
In the sample treatment setting, multiple decisions must be made to determine what treatment modalities clients will receive based on their ANSA LON scores. Clients who received an LON score of one, two, or three were referred to an outpatient treatment program equipped to treat less severe substance use disorders. Those assessed with an LON score of four or five, as well as those unable or unwilling to maintain abstinence from substances during treatment, were referred to an intensive outpatient treatment program equipped to treat more severe substance use disorders. Others determined to be appropriate for an inpatient option, most often because they continued to remain unable or unwilling to maintain abstinence from substances, were referred to a residential treatment program equipped to treat the most severe substance use disorders.
All clients were screened at intake for co-occurring mental disorders. Those diagnosed with co-occurring disorders, as well as those deemed likely to benefit from pharmacotherapy in the treatment of substance use disorders, were referred for psychiatric assessment and medical management to augment their treatment regime. Participants in all modalities were expected to maintain abstinence from substances during treatment as determined by self-report and random drug and alcohol screens.
Analysis
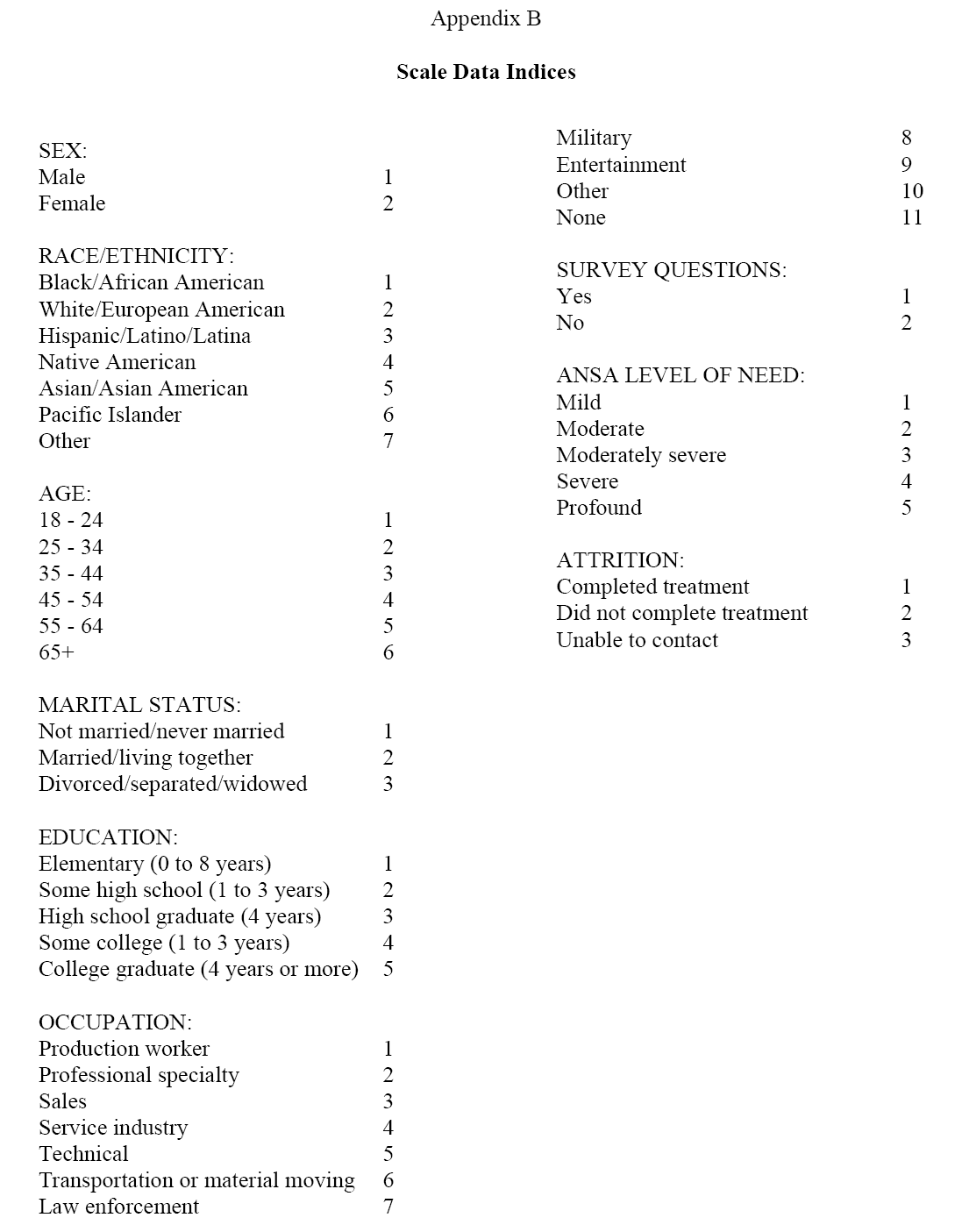
Substance use patterns, ANSA scores, age ranges, and education categories were converted into scale data, with differences measured according to indices created for those data (see Appendix B). Tests for internal consistency reliability using Cronbach’s alpha yielded a reliability coefficient of 0.75 on the adapted SSI-AOD pretest and 0.57 on the adapted SSI-AOD posttest. Presumably the lower result on the posttest coefficient was due to the high percentage of participants reporting improved outcomes, which restricted the range of variance and thus may have lowered the reliability coefficient. The hypothesis was tested by computing a one-tailed Pearson correlation. A one-tailed correlation was chosen because the direction of the hypothesis was expected to be positive.
Results
Of the 191 participants consenting to engage the study, 139 completed the treatment program while 52 did not complete the episode of treatment proposed by their therapists. Table 1 indicates that both the adapted SSI-AOD scores and ANSA LON scores were significantly lower following exposure to substance abuse treatment. The pretest mean for the adapted SSI-AOD was 3.12 and ANSA LON was 2.83, whereas the posttest mean for the adapted SSI-AOD was 0.88 and ANSA LON was 1.15, with lower scores indicating improved functioning.
| Measure | Pretest mean (Std.deviation) |
Posttest mean (Std.deviation) |
df | t-score | p-value |
|---|---|---|---|---|---|
| Positive responses to SSI-AOD questions | 3.12 (1.92) | 0.88 (1.20) | 123 | 12.37 | <0.05 |
| ANSA Level of Need assessment | 2.83 (0.99) | 1.15 (0.74) | 138 | 16.50 | <0.05 |
Note: N = 124. Lower number on measures denotes improvement. Standard deviation is in parentheses.
Table 1: SSI-AOD results and ANSA LON assessments of participants who completed treatment.
Table 2 indicates that the group comprised of participants disengaging prematurely from treatment did not differ statistically in terms of age or education from those who completed treatment. However, those who withdrew did have more severe pretest substance abuse and psychosocial problems than those who completed treatment. This difference was seen in higher pretest scores on the adapted SSIAOD survey for participants who withdrew (M = 4.15) versus those who completed (M = 3.12). This also was seen in higher ANSA LON pretest scores for those who withdrew from treatment (M = 3.17) versus those who completed treatment (M = 2.83).
| Measure | Withdrawing (Std.deviation) |
Completing (Std.deviation) |
p-value |
|---|---|---|---|
| Age | 2.62 (1.03) | 2.73 (1.29) | <0.05 |
| Education | 2.94 (0.87) | 3.05 (.78) | <0.05 |
| Positive responses to SSI-AOD questions | 4.15 (2.06) | 3.12 (1.92) | <0.05 |
| ANSA Level of Need assessment | 3.17 (0.83) | 2.83 (0.99) | <0.05 |
Note: N = 52 withdrawing from treatment, N = 124 completing treatment
Table 2: Independent samples t-tests of those withdrawing from treatment versus those completing treatment.
Fifteen participants were unavailable for the posttest because their phone numbers were incorrect, their answering service was not functioning, or they did not return phone calls. One participant reportedly was incarcerated following treatment, and another participant had died. Table 3 indicates that the group comprised of those unavailable for the posttest did not differ statistically in terms of age or education from those available for the posttest. However, those unavailable for the posttest did have less severe pretest substance abuse and psychosocial problems. This difference was seen in lower scores on the adapted SSI-AOD survey for participants unavailable for the posttest (M = 2.73) versus those who were available (M = 3.12). This also was seen in lower ANSA LON scores for those unavailable for the posttest (M = 2.20) versus those available for the posttest (M = 2.83).
| Measure | Unavailable (Std.deviation) |
Available (Std.deviation) |
p-value |
|---|---|---|---|
| Age | 3.00 (1.20) | 2.73 (1.29) | <0.05 |
| Education | 2.87 (0.74) | 3.05 (0.78) | <0.05 |
| Positive responses to SSI-AOD questions | 2.73 (1.87) | 3.12 (1.92) | <0.05 |
| ANSA Level of Need assessment | 2.20 (1.08) | 2.83 (0.99) | <0.05 |
Note: N = 15 unavailable for posttest, N = 124 available for posttest
Table 3: Independent samples t-tests of those unavailable for posttest versus those available.
Correlations
The one-tailed Pearson bivariate analysis revealed a moderate positive correlation between change scores pretest versus posttest on the adapted SSI-AOD self-report survey and change scores on the ANSA LON clinical assessment significant at the 0.01 level (r = 0.31, p < 0.01), supporting the research hypothesis that as participants were reporting improved change scores, they also would be assessed by their therapists as having achieved improved overall functioning.
A moderate positive correlation also was found between change scores pretest versus posttest on the adapted SSI-AOD self-report survey, and change scores on the ANSA Substance Use Disorder clinical assessment. The one-tailed Pearson bivariate analysis revealed a low positive correlation of 0.21, p < 0.01, suggesting that as participants were reporting improvement with regard to substance use patterns on the adapted SSI-AOD survey, they also were being assessed by their therapists with improved scores on the related domain of the ANSA, thus supporting the research hypothesis.
A one-tailed Pearson bivariate correlation supported the research hypothesis that there would be a positive linear relationship between change scores pretest versus posttest on the adapted SSI-AOD selfreport survey, and change scores on the ANSA Criminal Behavior clinical assessment. The Pearson correlation was small but significant (r = 0.15, p < 0.05), suggesting that as participants reported fewer substance use problems on the adapted SSI-AOD survey; they also were being assessed by their therapists as having engaged in less criminal activity.
It was hypothesized that change scores pretest versus posttest on the adapted SSI-AOD self-report survey would be correlated with change scores on the ANSA Community Connection clinical assessment because it was expected that as participants reported fewer substance abuse problems, they also would become more sociable and enjoy a greater sense of community. This hypothesis was not supported as a one-tailed Pearson bivariate correlation analysis revealed an inverse correlation that was not statistically significant, and likely due to chance.
Discussion
The results of the data are important because clinicians need to be aware of their clients’ progress, and to know that clinical tools of measurement are assessing their clients accurately. The validity of such tools is essential because the complexity of the intake process requires that abstract information be translated quickly and easily into quantifiable data that can be tracked over time.
During the intake interview, many clients are focused inward on the initial problems, symptoms, and concerns that caused them to seek therapy in the first place. Instruments such as the ANSA can bring meaning and interpretation to such problems, symptoms, and concerns, and can help untangle clients’ stories so that their needs, objectives, and goals are identified and addressed. When clients perceive that they are being understood, which in turn may help clients understand themselves better, they may overcome their initial difficulties in communicating their stories, and may feel more hopeful about the therapy process.
Overall, clinical assessments of the ANSA were found to be useful for documenting the experience of the clients by revealing a direct correlation between change scores on the adapted SSI-AOD selfreport survey and change scores on the ANSA Level of Need clinical assessment, Substance Use Disorder assessment, and Criminal Behavior assessment. This demonstration of validity should increase therapists’ confidence in the ANSA as an objective tool for interpreting subjective, abstract clinical information, especially during the intake process.
The changes in ANSA scores following treatment were not unexpected because many psychosocial problems reported by participants were known to be substance-related. In other words, financial stressors, relational problems, physical illnesses, and so forth, often are the result, directly and indirectly, of substance abuse patterns. Thus, a lower score on the adapted SSI-AOD survey coupled with a lower score on ANSA assessments was heartening, but must be understood within the context of the complexities of substance abuse research.
However, because the research did find that scores on the adapted SSI-AOD survey were associated with scores on the ANSA LON clinical assessment, it could be said, then, that change scores as selfreported by participants were found to be correlated positively with change scores as clinically measured by therapists during an assessment interview. This result not only means that improvements in substance use patterns were associated with improvements in global functioning across ANSA domains, but also that the validity of the ANSA as a tool of measurement was supported.
A moderate positive correlation was found between improved scores on the adapted SSI-AOD and improved scores on the ANSA Substance Use Disorder clinical assessment. This suggested that, in general, as participants reported improvement with regard to substance use patterns, they were assessed by their therapists as improving on the Substance Use Disorder domain of the ANSA. Though the correlation was expected to be higher, in the moderately strong to very strong range, the results were encouraging and further validated the ANSA. Possible explanations for why the correlation was not stronger include that, because of denial and other factors, individuals early in recovery often think they are doing better than they really are, or that therapists often remain cautious about recognizing psychosocial improvement until substantial time (perhaps measured in years) has passed. The observation that the correlation was slightly stronger at pretest (r = 0.25, p < 0.01) than at posttest (r = 0.22, p < 0.05) may support this conjecture. It should be noted, as well, that the scoring system of the ANSA makes a distinction between early remission from substances (defined as less than one year), and sustained remission (defined as more than one year), and many participants had yet to sustain remission for greater than one year due to the limited timeframe of the study.
A weak but statistically significant positive correlation was found between improved scores on the adapted SSI-AOD and improved scores on the ANSA Criminal Behavior clinical assessment. This result was understood to mean that, as participants reported fewer substance use problems, by and large they were being assessed by their therapists as engaging in less criminal activity. One possible explanation for why the correlation was not stronger, at least in the moderate to moderately strong range, may be that the scoring system of the ANSA makes a distinction between criminal behavior conducted during the past year versus criminal behavior conducted more than one year ago. It should be noted that the vast majority of participants court-mandated to treatment had been arrested for crimes committed more than a year ago due to the deliberate pace of the criminal justice system. Thus, their ANSA scores would not be expected to show much improvement on this domain.
Contrary to expectations, no correlation was found between scores on the adapted SSI-AOD and scores on the ANSA Community Connection clinical assessment. This result was surprising as one might expect that individuals gaining mastery over a substance use disorder then would become more involved in the cultural aspects of community life, would be more accepted by their neighbors, and would form new informal networks of friends. However, it is unclear how therapists would know about such changes, or how such changes could be made to occur during a therapeutic program lasting just weeks or months. Thus, it is not known whether the lack of correlation reveals a weakness in the instrument, or a lack of association between substance use and community life.
Possible explanations for why no correlation was found between these two variables include that community connection is unlikely to change much over weeks and months, i.e., the timeframe of the study. Also, the scoring system of the ANSA makes a distinction between short-term and long-term ties to the community, with long-term ties, such as involvement in a neighborhood group, acceptance by neighbors, or forming informal networks of friends, defined as more than one year, a timeframe beyond the scope of the study. Additionally, perhaps the case could be made that sobriety caused some participants to become less sociable by limiting their involvement in cultural events that revolve around substances, such as neighborhood beer gardens.
Limitations
One hundred thirty-nine of the 191 participants engaging the study completed the recommended treatment program, while 52 did not complete the episode of treatment proposed by their therapists. This 27% attrition rate is comparable to the 25.4% rate reported in the literature. The attrition rate in this study may have been elevated, in part, because one therapist in the program took an extended medical leave of absence, causing some clients to seek services elsewhere. The significance is that attrition may produce an effect whereby treatment outcomes are elevated. This may occur because participants highly motivated to complete treatment also are motivated to make therapeutic progress, which could have skewed the results of this study.
Also, the three-month follow-up window may overstate improvement if participants relapse after the assessment and thus require further treatment. An extended follow-up period with a more precise endpoint may provide a better evaluation of ongoing progress and enduring changes, and a more accurate determination of the longterm trajectory of outcomes.
More seriously, adapting the comparison instrument reduces the precision of the analysis and limits the methodological claims that can be made from this study. Further, because the magnitude of the correlations was statistically significant but small, the results may explain very little shared variance. And while there was speculation about the reason for the poor posttest alpha, it is unclear what impact the low alpha may have had on the results. These limitations, however, provide opportunities for further exploration. If practicable, future research could involve a true experimental design with a comparison group and multiple levels of correlation analyses examining all of the domains of the ANSA.
Conclusions and Recommendations
Future studies employing both quantitative and qualitative research methods are needed to discover what particular concepts within the ANSA increase validity and reliability, and what concepts are predictive of improved substance abuse outcomes. Also, because the ANSA is used as a device for measuring psychosocial improvement, the central components of its psychometric construct should be examined and analyzed more extensively. Nevertheless, taken as a whole, the preliminary evidence does suggest that the ANSA is a valid tool of measurement, and that it does reflect the client’s perspective accurately, thus strengthening confidence in its use as a standardized screening instrument.
Future research should seek to discover if attrition, relapses, modality of treatment, co-occurring disorders, the low occurrence of marriage, and the high occurrence of unemployment were confounding factors in this study. In addition, it should be noted that those who withdrew from treatment had slightly more severe substance abuse and psychosocial problems, and those who were unavailable for the posttest had slightly less severe substance abuse and psychosocial problems. Future studies should seek to understand what correlation, if any, exists among these variables.
Essentially, this research should be understood as a summary of technical reports with regard to one group moving through an episode of substance abuse treatment together. The analysis of the data is very descriptive, and the statistical analysis focusing only on correlations is limited in scope. It is hoped that in the future, the objectives of the study will be amplified, and that more complex statistical analyses, such as multivariate testing, will be conducted.
References
- http://praedfoundation.org/tools/the-adult-needs-and-strengths-assessment-ansa/
- LyonsJS (2009) Communimetrics: A communication theory of measurement in humanservice settings. (1st Edition)Springer Publishing Company, New York.
- Nelson C,Johnston M (2008) Adult needs and strengths assessment: Abbreviatedreferral version to specify psychiatric care needed for incoming patients,exploratory analysis. Psychological Reports 102: 131-143.
- Brady KT,Randall CL (1999) Gender differences in substance use disorders. AddictiveDisorders 22: 1-13.
- Biglan A,Hood D, Brozovsky P, Ochs L, Ary D, et al. (1991) Subject attrition inprevention research. In W. Bukoskiand K. Leukefeld (Eds.), Drug abuseprevention research: Methodological issues. NIDA Research Monograph 107(pp. 213-223). National Institute on Drug Abuse, Rockville, Maryland
- AmericanPsychiatric Association (2000) Diagnostic and Statistical Manual of MentalDisorders, (4th Edition), Text Revision. American PsychiatricAssociation, Washington, D.C.
- Allen RS(2014) Strengths and challenges of client outcomes in substance abuse treatment:What and why of effective therapy (Unpublished doctoral dissertation).National Louis University, Chicago, Illinois.
- http://www.ncdhhs.gov/mhddsas/DWI/dual diagnosis/SSI-AOD.pdf
- Kills-Small NJ, Simons JS, Stricherz M (2007) Assessing criterion validity of the simple screening instrument for alcohol and other drug abuse in a college population. Addictive Behaviors 32: 2425-2431.

Relevant Topics
- Addiction Recovery
- Alcohol Addiction Treatment
- Alcohol Rehabilitation
- Amphetamine Addiction
- Amphetamine-Related Disorders
- Cocaine Addiction
- Cocaine-Related Disorders
- Computer Addiction Research
- Drug Addiction Treatment
- Drug Rehabilitation
- Facts About Alcoholism
- Food Addiction Research
- Heroin Addiction Treatment
- Holistic Addiction Treatment
- Hospital-Addiction Syndrome
- Morphine Addiction
- Munchausen Syndrome
- Neonatal Abstinence Syndrome
- Nutritional Suitability
- Opioid-Related Disorders
- Relapse prevention
- Substance-Related Disorders
Recommended Journals
Article Tools
Article Usage
- Total views: 16997
- [From(publication date):
September-2015 - Nov 21, 2024] - Breakdown by view type
- HTML page views : 12505
- PDF downloads : 4492
