Research Article Open Access
Utilization of Immediate Post-Partum Intra Uterine Contraceptive Device and Associated Factors: A Facility based Cross Sectional Study among Mothers Delivered at Public Health Facilities of Sidama Zone, South Ethiopia
Lidetu Bezabih Tefera1, Mulumebet Abera2, Chaltu Fikru3and Dawit Jember Tesfaye4*1Lidetu Bezabih Tefera, Program Officer, Engender Health, Hawassa, Ethiopia
2Department of Population and Family Health, College of Public Health and Medicine, Jimma University, Jimma, Ethiopia
3Department of Epidemiology, College of Public Health and Medicine, Jimma University, Jimma, Ethiopia
4School of Public Health, College of Medicine and Health Sciences, Hawassa University, Hawassa, Ethiopia
- *Corresponding Author:
- Dawit Jember Tesfaye
School of Public Health
College of Medicine and Health Sciences
Hawassa University, Hawassa, Ethiopia
Tel: 251912173129
E-mail: devanhijember@gmail.com
Received date: May 16, 2017; Accepted date: May 27, 2017; Published date: May 31, 2017
Citation: Tefera LB, Abera M, Fikru C, Tesfaye DJ (2017) Utilization of Immediate Post-Partum Intra Uterine Contraceptive Device and Associated Factors: A Facility based Cross Sectional Study among Mothers Delivered at Public Health Facilities of Sidama Zone, South Ethiopia. J Preg Child Health 4:326. doi:10.4172/2376-127X.1000326
Copyright: ©2017 Tefera LB, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Pregnancy and Child Health
Abstract
Background: Insertion of an Intra Uterine device (IUD) immediately after delivery have a proven record of very high effectiveness, protection against unintended pregnancy, cost effectiveness, suitability and high user satisfaction. Despite these benefits, information on Post-Partum Intra Uterine device (PPIUD) acceptance and utilization was limited in Ethiopia. Therefore, this study was aimed to assess postpartum intra uterine contraceptive device utilization and its associated factors among mothers delivered in selected facilities found in South Ethiopia. Methods: A facility based cross-sectional study was conducted in two health facilities providing PPIUD insertion service (Yirgalem hospital and Bursa health center). Data were collected using structured questionnaire among 310 selected women. Frequency tables and graphs were used to describe the study variables. Bivariate and multivariate logistic regression analysis methods were used to identify factors associated with postpartum intrauterine device use. Variables with P-value of <0.05 with 95% CI were used to declare statistical significance. Results: Postpartum intra uterine contraceptive device use within 48 h of delivery was 21.6% while 38% of the respondents were interested in using PPIUD. Only 22.8% of participant mothers were counselled during ANC, labor and postpartum period. Mother who do not have a plan to have another child [AOR=2.36, 95% CI, (1.25, 4.47)], undecided plan to have another child [AOR=0.17, 95% CI, (0.05, 0.58)], mothers who did not heard [AOR=0.41, 95% CI: 0.41 (0.20, 0.83)] and not counselled about PPIUD [AOR=0.17, 95% CI: 0.17 (0.06, 0.52)] were associated with PPIUD utilization. Conclusion: Despite more than one-third of participants were accepted PPIUD, the actual utilization was low. Most mothers were not counselled during the important contact points through the whole cascade of pregnancy. Program managers need to develop strategies to raise pregnant mother awareness on PPIUCD through media sources. This study also highlights, the need to improve and integrate standard PPIUD counselling scheme during FANC, labor and postpartum period.
Keywords
Post-partum intra uterine device; Contraceptive; Postpartum period
Introduction
In sub-Saharan Africa approximately 53% of women (58 million) who wanted to avoid a pregnancy were not using family planning or were using a traditional method in 2012. These women accounted for 91% of unintended pregnancies [1]. For many of these women, childbearing begins at an early age, intervals between pregnancies are too short, and lifetime fertility is high [2]. The resulting fertility patterns lead to excess mortality and morbidity for both mothers and offspring [1,2]. Postpartum family planning (PPFP) is the prevention of unintended and closely spaced pregnancies through the first twelve months following childbirth [3]. Post-partum women need a range of effective contraceptive methods to be able to prevent an unplanned pregnancy, within a short interval [3].
Intrauterine device (IUD) insertion during the post-partum period is an ideal method for some women, as it does not interfere with breastfeeding, is convenient for both women and their health care providers, allows women to obtain safe, long-acting, highly effective contraception while already within the medical system [4,5].
Even though Post-Partum Intra Uterine Device (PPIUCD) has many advantages as a method of family planning, it generally suffers from unpopularity in Ethiopia. Ethiopia Demographic Health Survey (EDHS) report indicated that only 1.1% of women in the general population used IUCD as their modern contraceptive method [6]. Within two years post-partum, 74% women have an unmet need for FP; total unmet need decreases as the number of months post-delivery increases. Among women, less than 6 months postpartum, the overall unmet need is 86% [7]. In Ethiopia, there is a scarcity of information and evidence on PPIUD utilization. Therefore, this study aimed to assess acceptance and utilization of postpartum intra uterine contraceptive device and its associated factors among mothers who delivered in selected public health facilities of Sidama zone, South Ethiopia.
Materials and Methods
Study design and setting
Facility based quantitative cross-sectional study was conducted from February 01-March 29, 2016, in Yirgalem hospital and Bursa health center, Sidama zone, south Ethiopia. These health facilities where selected because postpartum intra uterine contraceptive device insertion service was provided during the study period. The hospital and health are located 313 and 443 km far from Addis Ababa, the capital city of Ethiopia. The hospital serves an estimated population of 4.2 million people.
Selection of the study subjects
The study population were all selected mothers who gave birth in Yirgalem hospital and Bursa health center during the study period. The sample size was calculated using single population proportion formula [8], with the following assumptions. Estimated proportion of PPIUCD utilization 23.7% [9], 95% confidence level and 3% margin of error. Since the total population was <10,000, we used population correction formula. After adding 10% non-response rate, the final sample size was calculated to be 310. On average, delivery service was provided for about 322 and 120 mothers in Yirgalem hospital and Bursa health center and the sample size was allocated to the two health facilities using probability proportional to size. Therefore, 225 and 85 consecutive mothers who gave birth after 28 weeks of gestation were included in the study. Mothers with the following gynaecologic or obstetric problems were excluded from the study. Intra uterine infection or puerperal sepsis, had active Sexually Transmitted Diseases (STD) or other lower genital tract infection; had ruptured membranes for more than 24 h, ruptured uterus, unresolved postpartum hemorrhage or postpartum uterine atony requiring use of additional oxytocic agents in addition to active management of third stage of labor (AMTSL), extensive genital trauma and pelvic inflammatory disease.
Data collection instrument and procedure
Data were collected using interviewer administered structured questionnaire. The questionnaire was adapted from different reviewed literature and it contains basic, intermediate and immediate factors affecting PPIUD utilization [9-12]. First, the questionnaire was prepared in English language and then translated to the Amharic language for the purpose of data collection. The Amharic version questionnaire was back-translated into English to check for consistency. Before the actual data collection, the questionnaire was pre-tested on 15 women delivered in Adare primary hospital, Hawassa town. Based on the pre-test findings, necessary amendment and corrections were made. Data collectors and supervisors were trained for two days about the study objectives and data collection processes. All filled questionnaires were supervised on daily basis for completeness and consistency. Four diploma nurses and two bachelor degree nurses were involved in the data collection and supervision process. Participants were interviewed at labour ward during first stage of labour. To collect data on the actual PPIUD utilization, participants were interviewed again in the postnatal wards.
Measurements
PPIUD acceptance was defined as those women who were accepted PPIUCD as a method of family planning but refused the actual insertion after the post-placental period, but within 48 hours of delivery. PPIUD utilization: Women who accepted PPIUD as a method of family planning and had actual PPIUCD insertion after the postplacental period, but within 48 h of delivery. Those women who refused insertion of PPIUCD after the post-placental period, but within 48 h of delivery were classified as decline to utilize PPIUD. Knowledge about FP was measured among women in the immediate postpartum period and they were classified as knowledgeable if the participants know at least two of the modern FP methods (i.e., Pills, Injection, Implant and IUCD). Participants were classified as counselled about PPIUD during ANC or latent phase of labour or within 48 h of delivery if the midwives told her at least either of the benefit, side effect or duration of PPIUD use. Family wealth was measured using ownership of selected assets, such as animals like oxen, cow, ship goat and presence of television and radio, types of water access and sanitation facilities. Reliability test was performed using variables involved in measuring the wealth of the participant’s household. Crohnbach’s alpha was calculated and variables employed to compute the alpha value were entered in to the principal component analysis to estimate a relative household wealth index. Tercile of the wealth index was generated and respondents were ranked into low, middle and high economic classes.
Data analysis
Data were entered into Epi-Info version 3.5.3 statistical software and exported to SPSS version 20 for further analysis. Frequency tables, graphs, and descriptive summaries were used to describe the study variables. Bivariate logistic regression analysis methods were used to select candidate variables for multivariate analysis. To control the effect of confounding variables and to identify factors associated with postpartum intrauterine device utilization, multivariable logistic regression analysis method was used and strength of association was determined by odds ratio at 95% CI. Significant association was declared when the p-value was less than 0.05.
Ethical considerations
The study obtained ethical clearance from the Ethical Review Board (ERB) of College of Public Health and Medical Sciences, Jimma University. Permission paper was obtained from administration of Sidama zone health bureau. Verbal consent was obtained from each study participants. Identification of study participants by name was avoided to assure the confidentiality of the information obtained.
Results
Socio-economic and demographic characteristics
All sampled study subjects were participated in the study making the response rate 100 %. The mean age (± SD) of the participants was 25.8 (± 4.49). Majority 201 (64.8%) of the participants were found in the age group of 25-34. Most 288 (92.9%) were married. The majority of the respondent were protestant 288 (67.1%) by religion. More than one quarter 121 (39.0%) were illiterate and 175 (56.5%) were housewive. About 125 (40.3%) of the respondents had neither television nor radio. A similar distribution of wealth status was observed among the participants with low 103 (33.2%), middle 104 (33.5%) and high 103 (33.2%) wealth index category (Table 1).
| Quality indicators | F7 G10976A (genotype G/A or А/А) | F13 G103T (genotype GT or TT) |
|---|---|---|
| Sensitivity, CI 95% | 62.61 (56.12-68.77) | 73.11 (67-78.63) |
| Specificity, CI 95% | 16.42 (8.49-27.48) | 5.97 (1.65-14.59) |
| Positive Predictive Value (PPV), CI | 72.68 (66.04-78.66) | 73.42 (67.31-78.93) |
| Negative Predictive Value (NPV), CI | 11 (5.62-18.83) | 5.88 (1.63-14.38) |
| Overall Fraction Correct, CI | 52.46 (46.69-58.18) | 58.36 (52.61-63.95) |
| Likelihood ratios for positive test results LR+ | 0.74 | 0.77 |
| Likelihood ratios for negative test results LR- | 2.27 | 4.5 |
Table 1: Hereditary risk factors for retrochorial hematoma.
Reproductive history and use of family panning
Majority 94 (38.4%) of the participants had a birth spacing of above 36 months followed by between 24 to 35 months, and less than 24 months 70 (28.6 %). Seventy-three (23.5%) of the participants current birth were not planned. Half 161 (51.9%) of the respondent had a plan to have another child in the future and 16 (9.9%) of the respondent were planned to have a child within 24 months in the future, 79 (49.1%) between 24 to 35 months and 66 (41%) after 36 and above months (Table 2).
| Indicators of hemostasis | 1st group (with RCH), n=468 | 2nd group (control), n=79 |
|---|---|---|
| Fibrinogen, g/l | 3.43 ± 0.88 | 2.96 ± 0.52 |
| (1.6-7.26) | (2.1-5.2) | |
| Thrombin time (TT), s | 18.64 ± 1.40 | 18.86 ± 1.84 |
| (13.0-25.7) | (14.0-22.4) | |
| Prothrombin time (PT), s | 12.5 ± 0.58* | 11.5 ± 0.73 |
| (9.8-15.6) | (10.5-13.5) | |
| Prothrombin index, % | 85.4 ± 4.85* | 93.7 ± 6.9 |
| (71-126) | (83-121) | |
| International normalized ratio (INR) | 1.06 ± 0.05* | 0.98 ± 0.06 |
| (0.84-1.44) | (0.88-1.24) | |
| Activated partial thromboplastin time (APTT), sec | 33.26 ± 3.26 | 31.37 ± 2.94 |
| (17.3-51.9) | (25.0-43.0) | |
| Soluble fibrin monomer complexes, mg% | 4.49 ± 1.63* | 3.3 ± 0.59 |
| (3.0-14.0) | (2.0-4.5) | |
| D-dimer, ng/ml | 739.4 ± 444.1* | 360.5 ± 179.0 |
| (205.0-3696.0) | (92.0-753.0) | |
| Factor VII activity, % | 99.83 ± 5.67** | 124.6 ± 2.75 |
| (84.5-117.9) | (104.7-138.1) | |
| Antithrombin III, % | 90.37 ± 26.39 | 83.34 ± 8.98 |
| (54-208) | (62-99) |
Table 2: Indicators of hemostasis in pregnant women with RCH and in women of the control group in terms of 6-11.6 weeks (Note: The comparison of the groups was performed by using the Mann-Whitney test, r�?0,05 *, ** p<0.01).
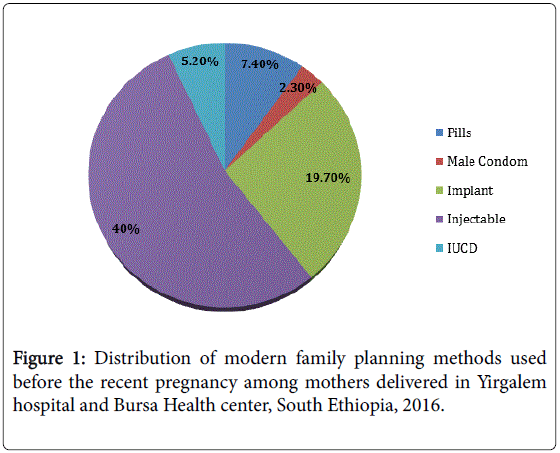
261 (84.2%) of the study participant were heard about modern FP method and 71.3% were knowledgeable about modern FP method. Among the study participants, most 199 (95.7%) were used family planning method before the recent pregnancy. Majority 124 (40%) were used injectable followed by 61 (19.7%) implant and 23 (7.4) pills. Almost all of the participants were used short term FP methods and interval IUCD was among the least used 16 (5.2%) method of family planning (Figure 1).
Regarding the antenatal follow-up, 261 (84.2%) of the study participant were followed ANC for their recent pregnancy either in the health center or hospital. Most of the study participants were delivered their recent child at the hospital (61.6%) and health center (34.5%). Only 3.9% of the participants were delivered at the health post. Of the total 310 participants, 222 (71.6%) of mothers mode of delivery were spontaneous vaginal delivery followed by 65 (21%) caesarean section.
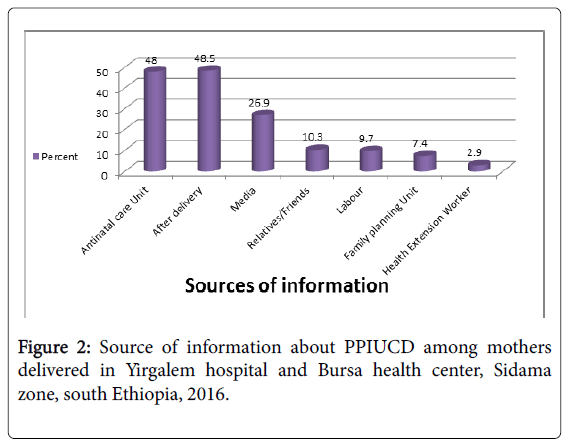
Utilization of post-partum intra uterine device
Among 175 (56.5%) participants who heard about PPIUCD, more than one third 118 (38.1%) were accepted PPIUD as a method of family planning and 21.9% (95% CI: 17.3, 26.5) of the study participants were utilized PPIUCD. The majority (48.0%) of the participants heard about PPIUD during antenatal follow up followed by post-natal care (43.8%). Only (2.9%) had used Health Extension Workers (HEWs) as their source of information (Figure 2).
Ninety-seven (43.3%) and 54 (24.1%) of the participants were counselled about PPIUCD after delivery and at ANC Follow up. Only 51 (22.8%) were counselled about PPIUD through the whole cascades of pregnancy contact points (Table 3).
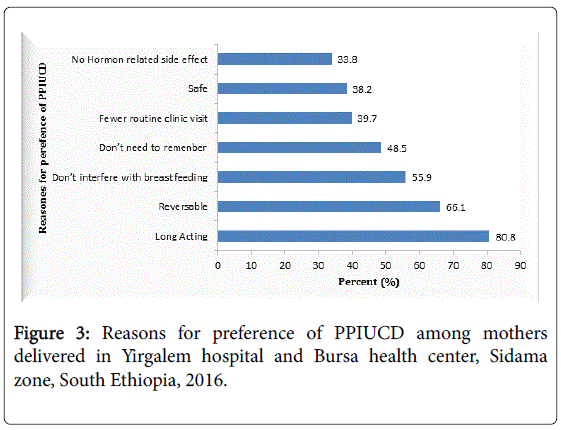
Among the study participants who accepted PPIUD, the majority of women (80.8) were due to the fact that it is a long-acting method. One third (66.1) of participants were accepted due to reversibility and more than half 56% considered PPIUD don’t interfere with breast feeding (Figure 3).
Factors associated with post-partum intra uterine device utilization
In multivariable logistic regression analysis, four variables were independently associated with PPIUD utilization. Mother who had a plan and undecided plan to have another child, heard about PPIUD and those who counselled were variables that showed significant association with PPIUD utilization.
The odds of PPIUD utilization were increased by 2.36 times among mothers who did not have a plan to have another child compared to mothers who had a plan to have another child [AOR=2.36, 95% CI, (1.25, 4.47)].
Mothers with undecided plan to have another child were less likely to utilize PPIUD than mothers who had a plan to have another child [AOR=0.17, 95% CI, (0.05, 0.58)]. Mothers who did not heard about PPIUD were less likely to utilize PPIUD than mothers who heard about PPIUD [AOR=0.41, 95% CI: 0.41 (0.20, 0.83)].
Mothers who are not counselled about PPIUD were less likely to utilize PPIUD than mothers who received counselling service about PPIUD [AOR=0.17, 95% CI: 0.17 (0.06, 0.52)] (Table 4).
Discussion
The IUD is one of the most highly effective, convenient, and costeffective FP method that does not interfere with breastfeeding and allow women to obtain safe and long-acting FP [13]. In this study, PPIUCD acceptance was 38.1%. However, only 21.9 % (95% CI: 17.3, 26.5) of the participants had actual PPIUD insertion within 48 hours of delivery. A similar finding was reported in the study conducted in Assuit, Egypt [9], where 28.9% accepted the use of IUCD after delivery and 23.7% had the actual insertion of IUCD. Other study conducted in obstetrics and gynecology department in MLB Medical College Jhansi reported 21.77% of women accept to use PPIUCD insertion [10]. Likewise, study conducted in 49 health centers involved in the initial rollout of PPIUD services in Ethiopia reported 8,374 deliveries and of these, a total of 1,647 (19.7%) women accepted PPIUD [14]. However, the Ethiopian Demographic and Health Survey (EDHS) showed that only less than 2% users of any contraceptive method use the interval IUCD, in spite of its low cost and effectiveness [15]. A plausible explanation for the relatively good acceptance of PPIUCD than the general public may be the presence of health care providers training and material support from a non-governmental organization in the study area. Postpartum IUCD insertion is an opportunity not to be missed in developing countries, where delivery may be the only time when a healthy woman comes into contact with health care providers and the chances of returning for contraceptive advice is uncertain [13].
In this study, those mothers who do not have a plan to have another child were more likely to use PPIUD than mothers who had a plan to have another child. Similar findings were reported in the study conducted in India [16]. This could be due to the fact that women who had a short pregnancy interval (have more children) to the index pregnancy required a long acting and reliable method of contraception [10]. This also has the added advantage of giving the mother enough time to recover from the physical stress of one pregnancy before moving on to the next and gives enough time for lactation. As a result, healthy timing and spacing of pregnancies provides an opportunity to have a positive effect on maternal health and new-born outcomes.
Mothers who did not heard about PPIUD were less likely to use PPIUD than mothers who heard about PPIUD. The finding of this study showed, majority (87.4%) of the participants were not aware about PPIUCD. Among those women who were utilized PPIUCD, less than half heard about the PPIUCD from the antenatal and postnatal clinic. This could be because the PPIUCD is a relatively new method of contraception in this community and one of the commonest reasons for non-use of contraception is lack of awareness.
In this study, counselling about PPIUD was significantly associated with PPIUD utilization. According to WHO, postpartum family planning counselling should optimally begin during ANC [17] and it is the ideal time to counsel women, but counselling during early labor and immediately postpartum is also acceptable. In this study, most acceptors (45.5%) received counselling during early labor, one-fourth (24.7%) were counselled during the immediate postpartum period and 16.7% were counselled during ANC. This finding indicates the importance of integrating post-partum family planning counselling nto ANC, early labor, and the immediate postpartum period to increase PPIUD utilization.
Conclusion and Recommendation
More than one-third of participants were interested in PPIUD use. However, only less than one-quarter of participant mothers were utilized PPIUCD. Although the majority of participants were counseled about PPIUD, most mothers were not counselled during the important contact points through the whole cascade of pregnancy. Most of the women preferred short term methods of FP despite they don’t have a plan to have another child within two years. Therefore, it is important to educate women on long-term methods of FP like PPIUD through developing strategies that aim to raise public awareness using different media sources. The best opportunity to provide information about FP is during child birth when they are in contact with healthcare providers. Thus, this study highlights, the need to improve and integrate standard PPIUD counselling scheme through the whole process of pregnancy; during focused ANC, labor and postpartum period.
Author Contribution
LB conceived the study and was involved in the design, coordination, field supervision, analysis and report writing. MA and CF were involved in proposal preparation, report writing and commented the draft manuscript. DJ participated in the design, data analysis, report writing and drafted the manuscript. All authors read and approved the manuscript.
Acknowledgement
Jimma University gave ethical clearance for the study but has no role in the design, data collection, analysis, report writing and decision on the manuscript submission. The authors appreciate the study participants for their cooperation in providing the necessary information. We acknowledge the local administrators and the community for their strong support during the study.
References
- Pri-paz SM (2012) Placenta previa, obstetric maging. Elsevier-Saunders.
- Asato K, Mekaru K, Heshiki C (2014) Subchorionic hematoma occurs more frequently in in vitro fertilization pregnancy. Eur J Obstet Gynecol Reprod Biol 181: 41-44.
- Tuuli MG, Norman SM, Odibo AO (2011) Perinatal outcomes in women with subchorionic hematoma: A systematic review and meta�?�analysis. Obstet Gynecol 117: 1205-1212.
- Kyser KL (2012) Meta-analysis of subchorionic hemorrhage and adverse pregnancy outcomes. Proc Obstet Gynecol 2: 4.
- Chhabra A, Lin EC (2014) Subchorionic hemorrhage imaging.
- McPherson JA, Odibo AO, Shanks AL (2013) Adverse outcomes in twin pregnancies complicated by early vaginal bleeding. Am J Obstet Gynecol 208: 56.
- Palatnik A, Grobman WA, Palatnik A (2015) The relationship between first-trimester sub chorionic hematoma, cervical length and preterm birth. Am J Obstet Gynecol 213: 1-4.
- Baranov VS (2009) Genetic passport-the basis of individual and predictive medicine. Saint-petersburg, p: 528.
- Kutteh WH, Davenport WB (2014) Inherited thrombophilias and adverse pregnancy outcomes: A review of screening patterns and recommendations. Obstet Gynecol Clin North Am 41: 133-144.
- Panfilova OY (2012) Clinical significance of the detection of thrombophilia, markers of inflammation and endotheliopathy for the prediction and prevention of repeated premature detachment of the normally located placenta and chorion detachment. Obstet Gynecol Sci 59: 233-237.
- Heller DS, Rush D, Heller DS (2003) Sub chorionic hematoma associated with thrombophilia: Report of three cases. Baergen Pediatr Dev Pathol 6: 261-264.
- Seremak-Mrozikiewicz A, Drews K, Kurzawi�?ska G (2009) The connection between Arg353Gln polymorphism of coagulation factor VII and recurrent miscarriages. Ginekol Pol 80: 8-13.
- Zonouzi P, Chaparzadeh N, Ghorbian S (2013) The association between thrombophilic gene mutations and recurrent pregnancy loss. J Assist Reprod Genet 30: 1353-1359.
- Wells PS, Anderson JL, Scarvelis DK, Doucette SP, Gagnon F (2006) Factor XIII Val34Leu variant is protective against venous thromboembolism: A huge review and meta-analysis. Am J Epidemiol 164: 101-109.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 5587
- [From(publication date):
June-2017 - Jul 09, 2025] - Breakdown by view type
- HTML page views : 3973
- PDF downloads : 1614