Research Article Open Access
Utilising Oesophageal Biodegradable Stent in Benign Pyloric Stenosis: Novel Technique
Hammad Ahmed1*, Qandeel Haitham1, Sajid Mohamed1, Murch Cliff2 and Mahmud Sajid11Department of Gastrointestinal Surgery, Hairmyres Hospital, NHS Lanarkshire, UK
2Department of Radiology, Hairmyres Hospital, NHS Lanarkshire, UK
- *Corresponding Author:
- Ahmed Hammad
Department of Surgery, Hairmyres Hospital
NHS Lanarkshire, UK
Tel: 0044-7923425235
E-mail: ahammadfarrag@yahoo.com
Received date: June 16, 2015 Accepted date: July 14, 2015 Published date: July 25, 2015
Citation: Ahmed H, Haitham Q, Mohamed S, Cliff M, Sajid M (2015) Utilising Oesophageal Biodegradable Stent in Benign Pyloric Stenosis: Novel Technique. J Gastrointest Dig Syst 5:307. doi:10.4172/2161-069X.1000307
Copyright: © 2015 Ahmed H, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License; which permits unrestricted use; distribution; and reproduction in any medium; provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Background: Benign pyloric stenosis in not uncommon problem. Different treatment modalities can be implemented each has its drawbacks. In this present a new technique of placement of biodegradable oesophageal stent for treating gastric outlet obstruction secondary to benign peptic stricture Method: 23 year old lady had long history of gastric outlet obstruction secondary to pyloric stenosis requiring recurrent hospitalisation; she had multiple admissions with repeated endoscopic dilatation which relieves her symptoms of short period. Decision was made of placement of pyloric biodegradable (BD) stent as a salvage treatment prior to resorting to surgery, biodegradable stents are designed for oesophageal placement and the delivery system is short to reach the pylorus in a dilated chronic obstructed stomach.
Abstract
Background: Benign pyloric stenosis in not uncommon problem. Different treatment modalities can be implemented each has its drawbacks. In this present a new technique of placement of biodegradable oesophageal stent for treating gastric outlet obstruction secondary to benign peptic stricture
Method: 23 year old lady had long history of gastric outlet obstruction secondary to pyloric stenosis requiring recurrent hospitalisation; she had multiple admissions with repeated endoscopic dilatation which relieves her symptoms of short period.
Decision was made of placement of pyloric biodegradable (BD) stent as a salvage treatment prior to resorting to surgery, biodegradable stents are designed for oesophageal placement and the delivery system is short to reach the pylorus in a dilated chronic obstructed stomach.
Result: A SX-ELLA oesophageal bio degradable (BD Stent) used to overcome the problem of the short delivery system a novel technique was adopted:
A nylon fishing wire was securely tied to the tip of a pyloric dilatation guide wire, under endoscopic guidance the pyloric dilatation guide wire (with the nylon wire attached to its tip) passed through the stenosed area, the dilator placed in the fourth part of the duodenum and the balloon inflated (position checked under fluoroscopy), the balloon was pulled out while inflated to shorten the length between the oesphagogastric junction and the pylorus, the stent then passed over the nylon wire and diploid across the stenosed area (position checked under fluoroscopy).
Patient seen in follow up three months post procedure with no sign of gastric outlet obstruction and started putting on weight.
Conclusion: This study presents a novel technique of utilising oesophageal BD stent in benign pyloric stenosis. A favourable technical and clinical outcome has been achieved. A larger prospective study is needed to validate such observation.
Keywords:
Pyloric stenosis; Peptic stricture; Biodegradable oesophageal stent
Introduction
Gastric outlet obstruction (GOO) is secondary to benign or malignant cause. The majority of benign strictures are caused by peptic ulcer disease (PUD). Although PUD is a common condition with a yearly incidence of more than 5 cases per 1000 persons [1], less than 5% of PUD sufferers will go on to have GOO. About 2000 operations per year are performed, in USA, to deal with ulcer related complications [2].
Treatment options for benign GOO include endoscopic pneumatic balloon dilatation (PD), placement of a self-expanding metal stent (SEMS) or surgery, all of which come with their own risks. PD often needs multiple attempts [3] for a lasting result and is associated with an increased risk of perforation [3,4]. SEMS used more frequently in patients with malignant disease, however high complication rate is reported and it can be as high as 25% [5]. Stent migration is the most common complication (17%) [6] and the use of SEMS in benign GOO has a higher migration rate (62%) [7]. Surgery is the final option to choose. It carries an overall complication rate of (16%-61%) and mortality (7%-30%) [8,9].
The newly developed bio-degradable (BD) self-expanding stent has shown promising results in treating benign oesophageal stricture with lower migration rate (9.5%) [10]. Unfortunately, BD stents are only designed for oesophageal strictures with a short delivery system. In this study, we aimed to present a new technique that utilises the BD oesophageal stent in the pylorus to treat GOO secondary to benign stricture.
Material and Methods
Patient
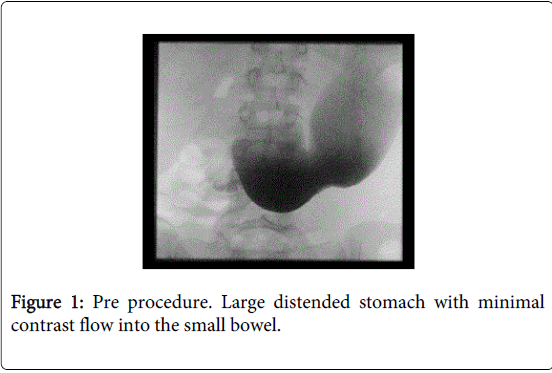
Our patient was a 23 year-old white Caucasian woman who first presented with a 5-week history of epigastric pain and profuse vomiting. On examination, the patient was under-weight and the sign of succussion splash was evident. GOO was confirmed on Barium meal (Figure 1). Gastroscopy showed tight pyloric stenosis due to peptic ulcer. Helicobacter pylori and gastrin testing were negative. Patient had not been using any medications known to cause stomach irritation.
She underwent four times of balloon dilatations over the following five months but each time the GOO relief was short lived. High dose PPI and H2-receptor antagonist did not improve her symptoms. Her nutritional status became concerning as her BMI dropped below 19. She re-presented 5 months later with recurrent obstructive symptoms and her GOOSS (Gastric Outlet Obstruction Scoring System) score was 0. Decision was made to place a pyloric BD stent as a salvage treatment prior to resorting to surgery. The patient was counselled and informed consent was obtained.
BD stents are designed for oesophageal placement and their delivery system is too short to reach the pylorus in a chronically dilated obstructed stomach. Therefore, a novel technique was adopted.
Equipment used
A forward viewing endoscope with working channel 3.7 mm (GIF-2T 240; Olympus Co.).
A wire-guided pyloric balloon-dilatation-catheter: 12 mm-13.5 mm-15 mm (CRE, Boston Scientific).
An oesophageal degradable BD stent (dimensions: 25-31 mm diameter and 120 mm length), delivery system outer diameter 6.0-9.4 mm and active length 75 cm (SX-ELLA; ELLA-CS).
A single-use guide-wire 0.035-inch diameter and 45 cm working length, with angled tips (VisiGlide; Olympus Co).
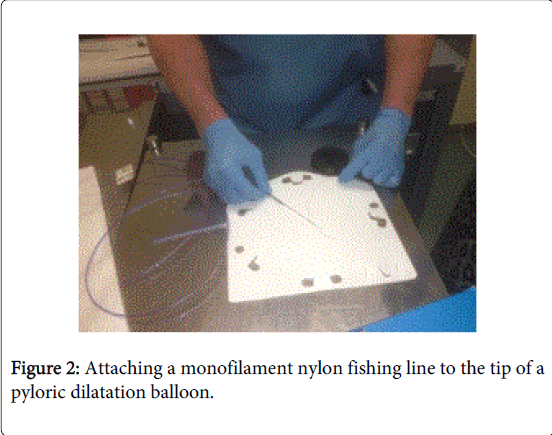
A monofilament nylon fishing wire with a length adjusted to accommodate the stent’s delivery system.
Technique
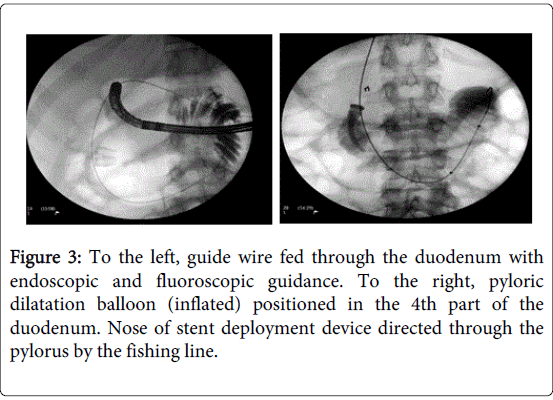
The patient was put under general anaesthesia in supine position. The fishing wire was securely tied to the tip of the pyloric dilatation-balloon-catheter (Figure 2). Then this catheter was passed through the stricture under endoscopic guidance. The catheter was advanced into the fourth part of duodenum where the balloon was inflated under fluoroscopic guidance (Figure 3). The fishing wire, anchored to the inflated balloon in duodenum, was put under tension and the BD stent was passed over it.
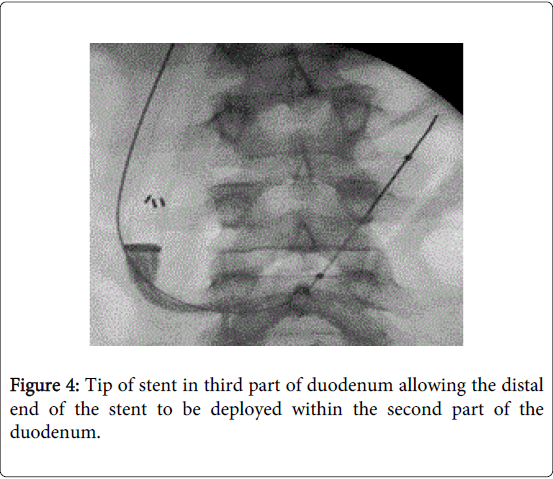
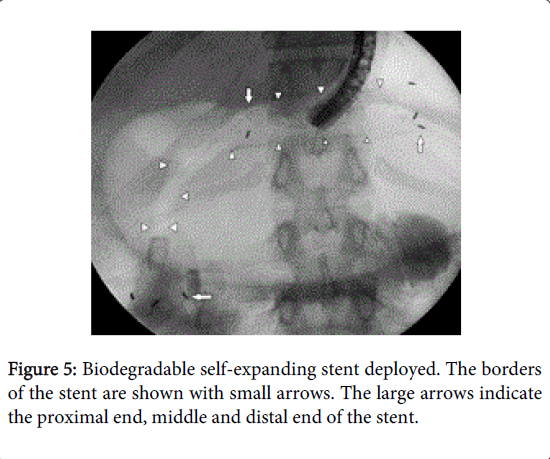
This fishing wire directed the tip of the BD stent through the pyloric stricture and into the second part of the duodenum (Figure 4). The tensed fishing wire reduced the distance needed to travel by the BD stent. When the stent reached the desired position, the balloon was deflated and pulled back completely out of mouth and the fishing wire was cut. 120 mm length stent was then deployed. Stent distal end was in the second part of the duodenum and the proximal end in the stomach (Figures 5 and 6).
Results
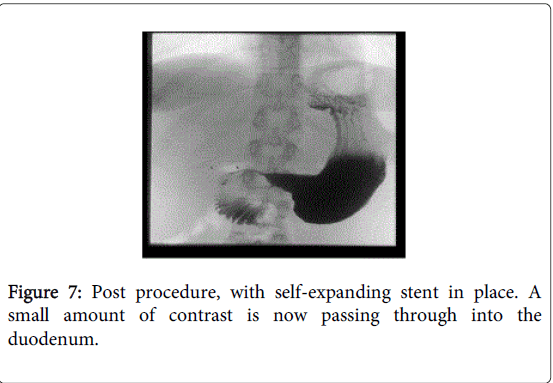
No immediate or late complications occurred after this procedure. In the first 24 hours, patient’s symptoms improved and her GOOSS score improved to 3. Water soluble contrast study was done 24 hours post procedure and showed the passage of contrast into the duodenum (Figure 7). The hospital stay was 10 days: 7 days prior to procedure during which the patient was on total parenteral nutrition (TPN) and 3 days post procedure for weaning off the TPN. Patient’s follow-up at 3 and 6 months post procedure confirmed weight gain and absence of GOO symptoms.
Discussion
SEMS management for malignant GOO has already been established. Recently published meta analysis showed comparable results in major and minor complications between SEMS versus gastrojejunostomy (GJ). However, results were in favour of SEMS in terms of shorter hospital stay, shorter time to tolerate oral intake and lower mortality [11]. Some studies have suggested temporary use of SEMS in benign stenosis of the GI tract [7,12,13]. Choi et al. [7] reported 81.8% symptomatic improvement of benign GOO after SEMS placement however stent migration was the most common complication (62.5%) in this series. Therefore, elective removal of the stent within four weeks of placement was recommended. Three studies [10,14,15] has been published showing the outcome of Ella esophageal BD stent since it became available to use in 2007, all these studies showed technical success rate of 100%, clinical success rate 30%[14] -100% [10,15] and migration rate 9% [10] -20% [14].
The main determinate of symptom recurrence varies according to the pathology of GOO. The stent patency is the main issue in malignant GOO. The reported SMEMS obstruction rate is 12% [16]-18% [11]. Tumour in-growth or over-growth is the main cause of obstruction less frequently is food impaction. The median patency of the SMES is 190 [17]-307 days [16]. In benign GOO symptom improvement and recurrence of obstruction is related to stent migration. Choi et al. [7] suggested that gradual expansion of SEMS over at least one week gives enough time for long lasting therapeutic dilatation. In his serious 100% of cases with early migration (less than one week) has recurrent symptoms versus 22.3% with late migration. To our knowledge, no BD stent had ever been used in benign pyloric stricture.
In this study, we applied the BD stent as a last resort after failure of repeated PD and prior to surgery (GJ). The main obstacle to use the BD stent in the pylorus was the length of its delivery system, which is 75 cm, as it is designed for oesophageal placement. In chronically dilated stomach, the guide wire (over which the delivery system should be mounted) would follow the concavity of the greater curvature of the stomach to enter the pylorus. The delivery system, in this case, would fall short of the length required to reach the second part of duodenum. This leads to technical failure of the stent placement. In order to overcome this problem we adopted a new technique through attaching a monofilament nylon fishing wire to the tip of pyloric dilatation-balloon-catheter. Inflating the balloon beyond the obstruction acted as an anchor. The attached fishing wire straightened and subsequently shortened the line between the oesophagogastric junction and the pylorus. That is reducing the distance needed to travel by the BD stent to the pylorus.
This is a successful report of a novel technique to show the feasibility of using oesophageal BD stent in benign pyloric stenosis, overcoming the problem of the short delivery system in a chronically obstructed stomach, with no recorded immediate or late complication and good outcome, however being a single case report the validity of these results can be questioned. A larger prospective study is needed to validate such observation.
Conclusion
This study presents a novel technique of utilising oesophageal BD stent in benign pyloric stenosis. A favourable technical and clinical outcome has been achieved. A larger prospective study is needed to validate such observation.
References
- Everhart JE, Byrd-Holt D, Sonnenberg A (1998) Incidence and risk factors for self-reported peptic ulcer disease in the United States.Am J Epidemiol 147: 529-536.
- Gibson JB, Behrman SW, Fabian TC, Britt LG (2000) Gastric outlet obstruction resulting from peptic ulcer disease requiring surgical intervention is infrequently associated with Helicobacter pylori infection. J Am CollSurg 191: 32-37.
- Solt J, Bajor J, Szabó M, Horváth OP (2003)Long-term results of balloon catheter dilation for benign gastric outlet stenosis. Endoscopy 35: 490-495.
- Lam YH, Lau JY, Fung TM, Ng EK, Wong SK, et al. (2004) Endoscopic balloon dilation for benign gastric outlet obstruction with or without Helicobacter pylori infection.GastrointestEndosc 60: 229-233.
- Dormann A, Meisner S, Verin N, Wenk Lang A (2004) Self-expanding metal stents for gastroduodenal malignancies: systematic review of their clinical effectiveness.Endoscopy 36: 543-550.
- KimCG, ChoiIJ, LeeJY, Cho SJ, Park SR, et al. (2010) Covered versus uncovered self-expandable metallic stents for palliation of malignant pyloric obstruction in gastric cancer patients: a randomized, prospective study. GastrointestEndosc 72: 25-32.
- Choi WJ, Park JJ, Park J, Lim EH, Joo MK, et al. (2013) Effects of the temporary placement of a self-expandable metallic stent in benign pyloric stenosis.Gut Liver 7: 417-422.
- Maetani I, Tada T, Ukita T, Inoue H, Sakai Y, et al. (2004) Comparison of duodenal stent placement with surgical gastrojejunostomy for palliation in patients with duodenal obstructions caused by pancreaticobiliary malignancies.Endoscopy 36: 73-78.
- Del Piano M, Ballarè M, Montino F, Todesco A, Orsello M, et al. (2005) Endoscopy or surgery for malignant GI outlet obstruction?GastrointestEndosc 61: 421-426.
- Repici A, Vleggaar FP, Hassan C, van Boeckel PG, Romeo F, et al. (2010) Efficacy and safety of biodegradable stents for refractory benign esophageal strictures: the BEST (Biodegradable Esophageal Stent) study.GastrointestEndosc 72: 927-934.
- Nagaraja V, Eslick GD, Cox MR (2014) Endoscopic stenting versus operative gastrojejunostomy for malignant gastric outlet obstruction-a systematic review and meta-analysis of randomized and non-randomized trials. J GastrointestOncol 5: 92-98.
- Acunas B, Poyanlí A, Rozanes I (2002) Intervention in gastrointestinal tract: the treatment of esophageal, gastroduodenal and colorectal obstructions with metallic stents.Eur J Radiol 42: 240-248.
- Laasch HU, Martin DF, Maetani I (2005) Enteral stents in the gastric outlet and duodenum.Endoscopy 37: 74-81.
- Canena JM, Liberato MJ, Rio-Tinto RA, Pinto-Marques PM, Romão CM, et al. (2012) A comparison of the temporary placement of 3 different self-expanding stents for the treatment of refractory benign esophageal strictures: a prospective multicentre study. BMC Gastroenterol 12: 70.
- Vandenplas Y, Hauser B, Devreker T, Urbain D, Reynaert H (2009) A biodegradable esophageal stent in the treatment of a corrosive esophageal stenosis in a child. J PediatrGastroenterolNutr 49: 254-257.
- Van Hooft JE, Uitdehaag MJ, Bruno MJ, Timmer R, Siersema PD, et al. (2009) Efficacy and safety of the new WallFlex enteral stent in palliative treatment of malignant gastric outlet obstruction (DUOFLEX study): a prospective multicenter study. GastrointestEndosc 69: 1059-66.
- Van Hooft JE, van Montfoort ML, Jeurnink SM, Bruno MJ, Dijkgraaf MG, et al. (2011) Safety and efficacy of a new non-foreshortening nitinol stent in malignant gastric outlet obstruction (DUONITI study): a prospective, multicenter study.Endoscopy 43: 671-675.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 15077
- [From(publication date):
August-2015 - Apr 05, 2025] - Breakdown by view type
- HTML page views : 10521
- PDF downloads : 4556