Use of PRP in Rhinoplasty
Received: 28-Nov-2016 / Accepted Date: 16-Dec-2016 / Published Date: 23-Dec-2016 DOI: 10.4172/2161-119X.1000280
Abstract
Rhinoplasty is always associated with bruising, nasal swelling, nasal block and pre-orbital edema in the short postoperative period affecting the quality of life of patients negatively. Platelets play an important role in wound healing which has been proven by previous researches in other medical conditions for example: diabetes and wound healing. Those raised my interest to assess the use of PRP in rhinoplasty to assess its effect on wound healing. Platelets rich plasma (PRP) is claimed to fasten healing process reducing postoperative edema, bruising and bleeding.
Keywords: Rhinoplasty; Bruising; Nasal swelling; Edema
253808Introduction
The purpose of this study is to validate the enhanced healing effect of PRP therapy in rhinoplasty with osteotomy.
PRP injection will increase the number of platelets in wound area by 2-3 times which theoretically must increase the amount of growth factors that is released by the platelets locally promoting wound healing [1,2].
This will be assessed by examining the effect of injecting PRP in the surgical site and under the eye on pre-orbital edema, bruising, wound healing, nasal swelling and nasal patency [3].
A prospective study between 2 groups of patients with and without PRP was undertaken to assess the above parameters.
Methods
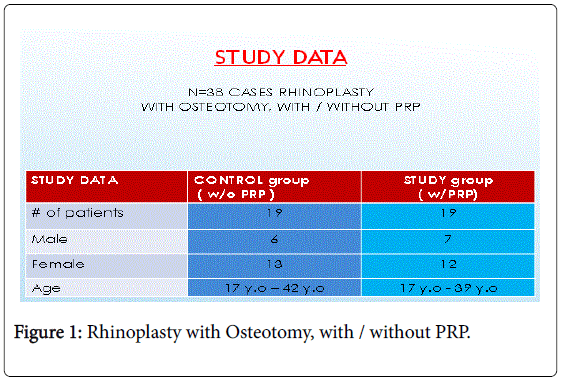
A prospective study of total 38 patients underwent open rhinoplasty with osteotomies. The total 38 patients were divided into two groups. The first group included 19 cases who had open rhinoplasty without PRP therapy and were considered the control group. The second group included 19 cases who had open rhinoplasty plus PRP therapy (Figure 1).
The technique involved harvesting blood at induction of anesthesia. Platelets rich plasma is then separated by centrifuging it and transferred through closed technique to another tube. The tube will then be activated prior to injection; which is usually administered at the end of the surgery and after wound closure. Activated PRP is transferred to 3 syringes, 2 insulin syringes for injection of 1ml under each eye and the rest about 2.5 ml to be injected into the septum (subperichondrial), on the dorsum of the nose and at the sites of osteotomies as well as at the columella around open rhinoplasty wound. Nasal bandaging will follow [4,5].
Patients are followed during their daycare stay then seen in follow up as at 48 h, 5 days, 10 days, 20 days, 30 days and 90 days. We assessed the following outcomes: per-orbital edema, bruising, nasal edema, nasal bleeding and nasal patency in the first 10 days postoperatively.
Originally 56 patients were included but eventually 18 patients were excluded either due to technique (closed rhinoplasty, no osteotomy, etc.) or the patients didn’t show up. So our inclusion criteria were open rhinoplasty with osteotomies and patients attending regular follow up.
Results
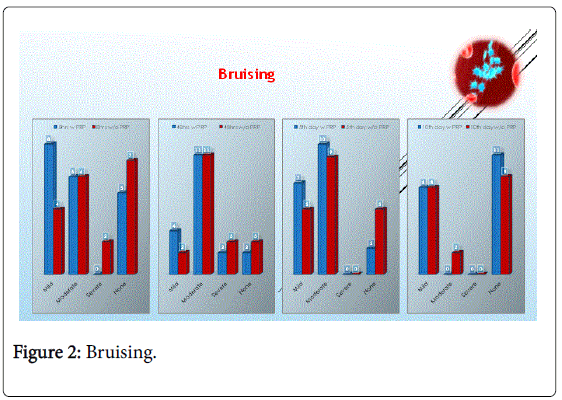
As we can see in the above bar charts bruising is less with PRP in the first few hours but it was almost equal within 5-10 days (Figure 2).
Bruising is rated from 0-5
• 0 means no bruising
• 1-2 means mild
• 3-4 means moderate
• 5 means severe
Bruising is graded according to colour as follows:
• yellow
• green
• purple
• blue
• red
So 1-2 mild, 3-4 moderate, 5 severe
Photos are taken by me or by my assistant and assessed accordingly.
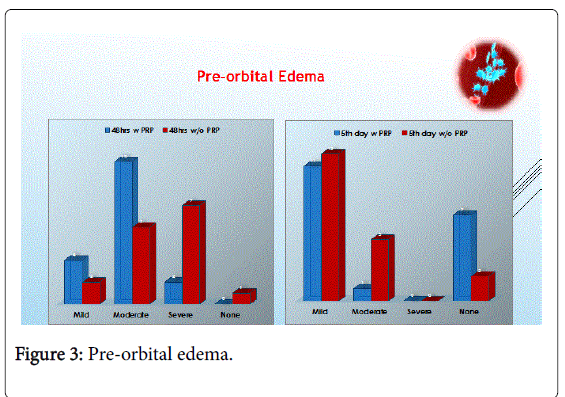
There is significant reduction in pre-orbital edema in the first 48 hours in the PRP group being almost mild to moderate while moderate to severe in the non-PRP group. In the 5th day 40% of PRP group were without pre-orbital edema versus 10% of non PRP group. (I considered mild pre-orbital edema when it is limited to the medial canthus area, sever when edema almost closing the eye while moderate is anything in between) Pre-orbital edema usually starts after 48 h in most cases (Figures 3 and 4).
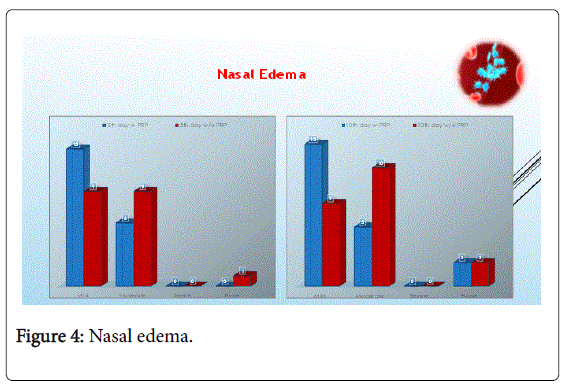
Regarding nasal edema 5th day postoperatively, in the PRP group, 68% had mild nasal edema and 31% had moderate edema versus the non PRP group whom results were 47.3% who had mild edema and 47.3% who had moderate edema. So in conclusion non PRP group had higher number of patients with moderate edema compared with PRP group who had milder nasal edema. In addition, at the 10th day the PRP group had better outcome of nasal edema compared to the non- PRP group; 73.7% versus 36.8% with mild nasal edema respectively and 26.3% versus 52.6% with moderate nasal edema respectively.
Discussion and Conclusion
There is significant improvement in the PRP group in terms of periorbital edema and nasal edema. There is no significant difference between both groups in terms of postoperative bruising. When it comes to bleeding, patients with PRP had better outcome. I feel confident to remove the nasal pack earlier in the PRP group as bleeding is less and edema regresses faster.
Definitely this study included a small sample size, which is a limitation. Future suggestions would be to include larger sample size and randomization to decrease bias. Another thought is to create a grading system to more accurately and objectively measure the studied outcomes.
Also we can extend our study for a month to 3 months regarding nasal edema. As we know that nasal edema may extend to 3 months especially in revision cases!
Overall nasal patency is better with PRP group but we need to construct a better measuring program as rhinomanometery to have more accurate results.
Comparison between primary and secondary rhinoplasty with PRP and an open rhinoplasty technique is still undergoing and data will be published soon!
References
- Pierce GF, Mustoe TA, Altrock BW, Deuel TF, Thomason A (1991) Role of platelet-derived growth factor in wound healing. J Cell Biochem 45: 319-326.
- Nurden AT, Nurden P, Sanchez M, Andia I, Anitua E (2008) Platelets and wound healing. Front Biosci 13: 3532-3548.
- Sclafani AP, Azzi J (2015) Platelet Preparations for Use in Facial Rejuvenation and Wound Healing: A Critical Review of Current Literature.Aesthetic Plast Surg 39: 495-595.
- Sclafani AP (2011) Safety, efficacy, and utility of platelet-rich fibrin matrix in facial plastic surgery. Arch Facial Plast Surg 13: 247-251.
- Lynch MD, Bashir S (2016) Applications of platelet-rich plasma in dermatology: A critical appraisal of the literature.J Dermatolog Treat 27: 285-289.
Citation: Al-Gerrah DA (2016) Use of PRP in Rhinoplasty. Otolaryngol (Sunnyvale) 6:280. DOI: 10.4172/2161-119X.1000280
Copyright: © 2016 Al-Gerrah DA. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 6402
- [From(publication date): 0-2016 - Apr 03, 2025]
- Breakdown by view type
- HTML page views: 5467
- PDF downloads: 935