Use of Living Cellular Bone Matrix for Treating a Failed Ankle Arthroplasty: An Abbreviated Technique and Case Study
Received: 14-Nov-2018 / Accepted Date: 29-Nov-2018 / Published Date: 06-Dec-2018 DOI: 10.4172/2329-910X.1000282
Abstract
Failed arthroplasty procedures can increase the susceptibility of a patient to complications. Salvage procedures require new approaches that are able to improve fusion speed and quality. A recently developed cellular bone allograft, ViviGen® (V-CBM), provides the osteoconductive, osteoinductive, and osteogenic properties needed for rapid and high-quality bone fusion. This cellular bone allograft contains a demineralized bone matrix component in addition to a viable cortico-cancellous bone matrix with osteoblastic lineage-committed bone cells. However, there is little clinical evidence for the use of V-CBM in ankle arthrodesis procedures. This detailed case study presents an outcome of using V-CBM to salvage a failed agility total ankle replacement with talar component subsidence and degenerative joint disease in the subtalar joint on the right ankle and hindfoot. Radiographs showed the femoral head allograft, in combination with V-CBM, was fusing to the native talus and calcaneus by 12 weeks and to native the tibia by six months. The patient was weight bearing at 5 months post-operative, and the significant preoperative pain diminished to a minimal amount. The patient remained completely satisfied with procedure as of the last followup at 23 months post-operative. V-CBM enabled a successful salvage of failed ankle arthroplasty that had been complicated by two failed previous failed replacement surgeries. While not generalizable, this may be the first published case of a cellular bone allograft used in the salvage of a failed ankle arthroplasty. These results support continued research into the clinical use of V-CBM for arthrodesis procedures in the foot and ankle.
Keywords: Cellular bone allograft; Ankle arthrodesis; Degenerative joint disease; Ankle salvage; ViviGen
Level of Evidence
Level 4.
Introduction
Ankle arthroplasty may be used as an alternative to arthrodesis to treat crippling arthritis in certain types of cases. However, failed arthroplasty procedures can increase the susceptibility of a patient to infection along with causing subsidence of the joints [1]. In the event of failure, arthrodesis can be employed as a salvage procedure [2], with the goal of rapid and high-quality bone fusion. Arthrodesis performed under standard conditions is susceptible to a high complication rate [3]. It stands to reason that particularly complex surgeries, such as ankle salvage, require advanced technologies and techniques to improve fusion speed and quality.
Ideal bone grafting materials should be osteoconductive, osteoinductive, and osteogenic. Autograft bone provides these qualities [4], but also has some notable disadvantages such as limited availability and potential morbidity at the harvest site. Recently, cellular bone matrix allografts have been developed which have the advantages of autograft while also avoiding its disadvantages. For example, ViviGen® (V-CBM) contains an osteoinductive demineralized bone matrix component in addition to a viable cortico-cancellous bone matrix, which is both osteoconductive and osteogenic. After recovery and processing, the allograft tissue is cryopreserved in a solution that maintains the viability of osteoblastic lineage-committed bone cells.
Preclinical studies have indicated that bone cells might improve fusion over MSCs by providing improved and directed bone deposition [5] while remaining in the defect site longer [6]. V-CBM has demonstrated success in foot and ankle arthrodesis procedures [7], but there is minimal clinical evidence for V-CBM or any other cellular bone allograft in ankle salvage. This case study presents the outcome of using V-CBM to salvage a failed ankle arthroplasty.
Case Description
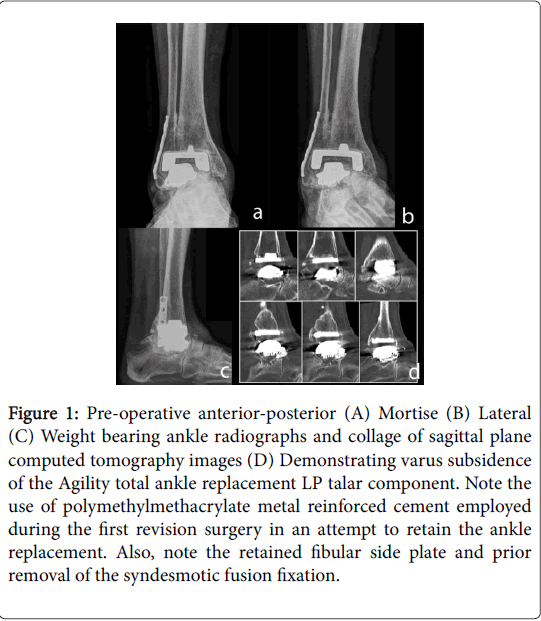
This case was performed at the author’s hospital-based practice. Informed consent was obtained for participation in this case study. A 73-year-old female presented with failed agility total ankle replacement with talar component subsidence and degenerative joint disease in the subtalar joint on the right ankle and hindfoot. The patient had a body mass index (BMI) of 33, pulmonary hypertension, chronic obstructive pulmonary disease (COPD), and a 15-year tobacco habit that had been quit 26 years prior. She was in a great deal of pain, with a score of 10 out of 10 using the visual analog scale (VAS). Medications included diuretics, tramadol, oxycodone, those for anti-seizure/mood-altering, and medication for managing blood pressures. The failed primary agility total ankle replacement took place in 2003 using a tibia size 3.0 mm bottom loaded polyethylene insert and a posterior augmented talar component. The failed revision Agility total ankle replacement was undertaken 10 years later (2013), retaining the tibia while using 2 mm 1/2 column polyethylene insert, size 3 LP talar component, and polymethylmethacrylate cement metal augmentation (Figure 1). A massive talar cyst was also observed. After the revision surgery failed 8.5 months post-operative, the patient was managed with bracing, pain medications, cane, and wheelchair use.
Figure 1: Pre-operative anterior-posterior (A) Mortise (B) Lateral (C) Weight bearing ankle radiographs and collage of sagittal plane computed tomography images (D) Demonstrating varus subsidence of the Agility total ankle replacement LP talar component. Note the use of polymethylmethacrylate metal reinforced cement employed during the first revision surgery in an attempt to retain the ankle replacement. Also, note the retained fibular side plate and prior removal of the syndesmotic fusion fixation.
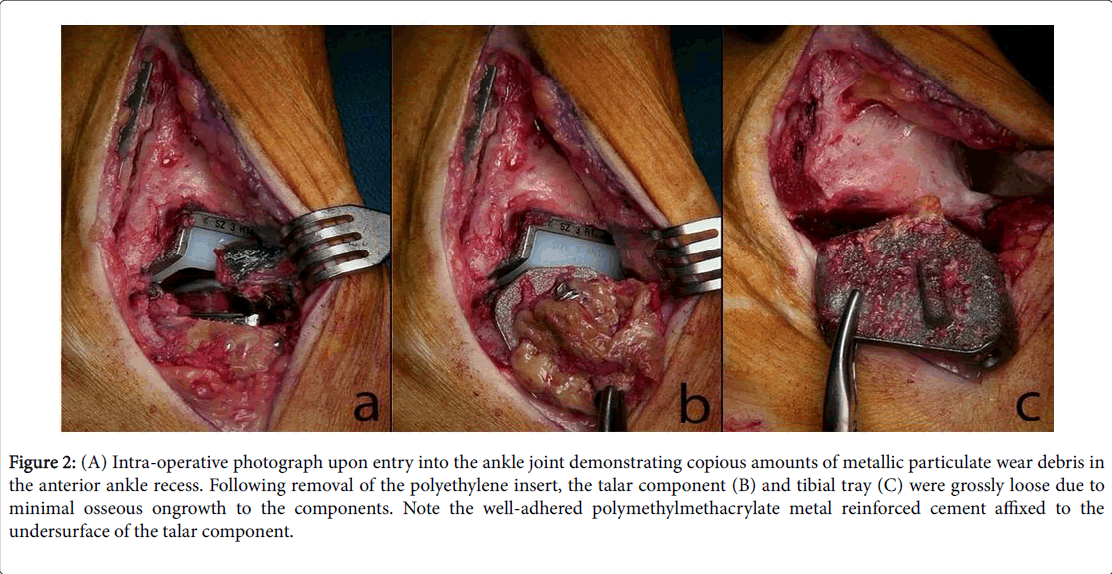
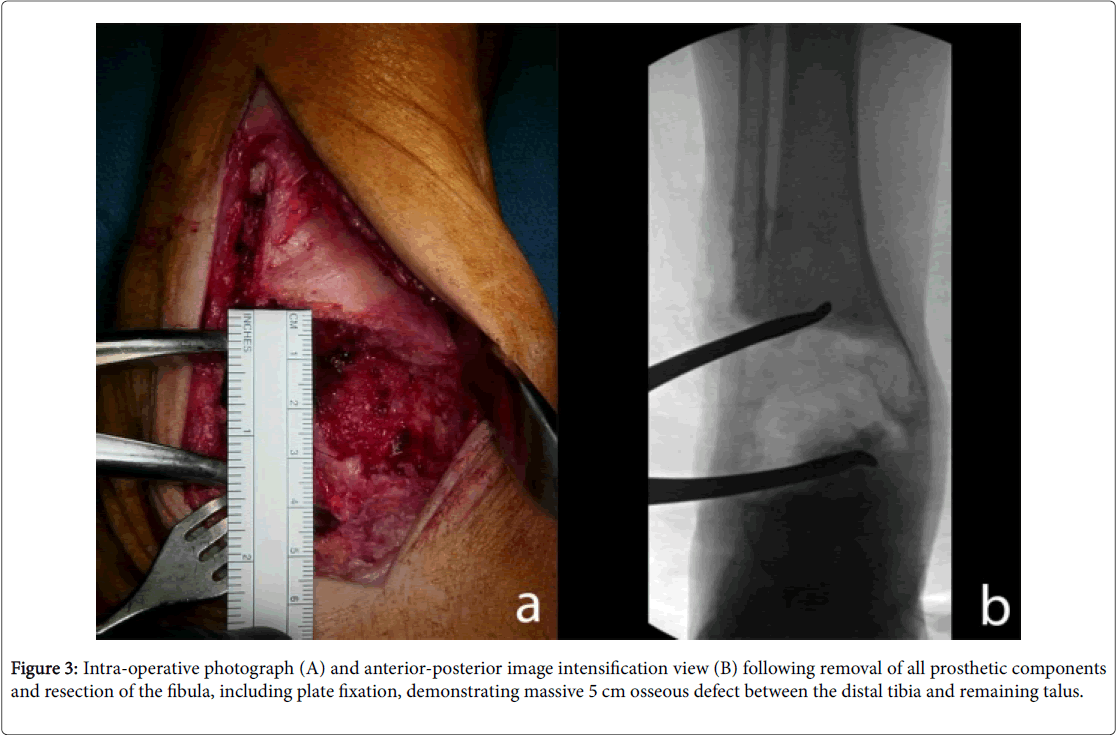
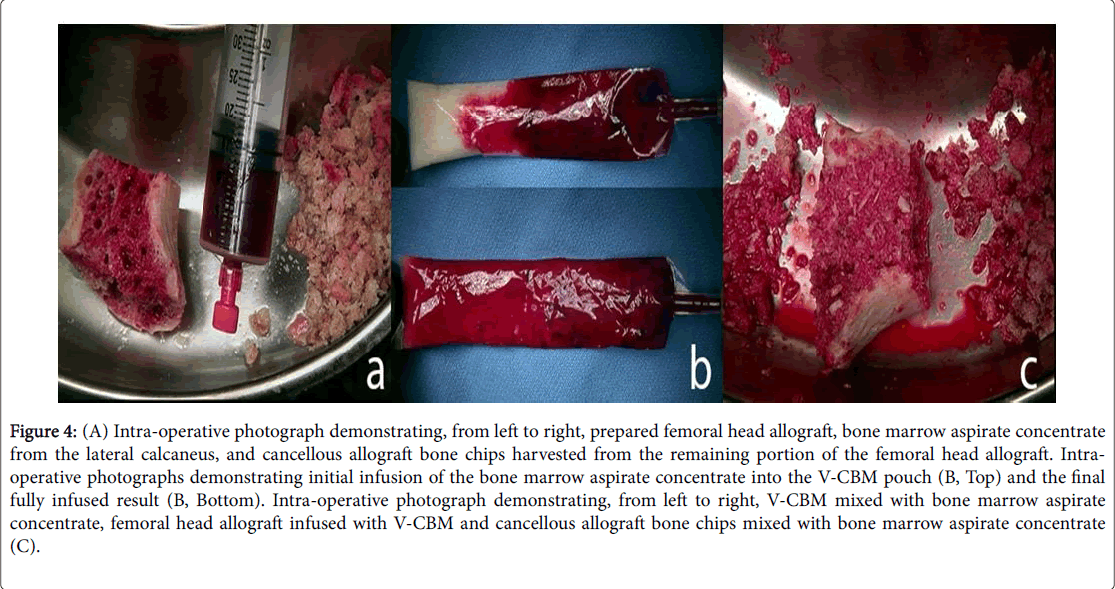
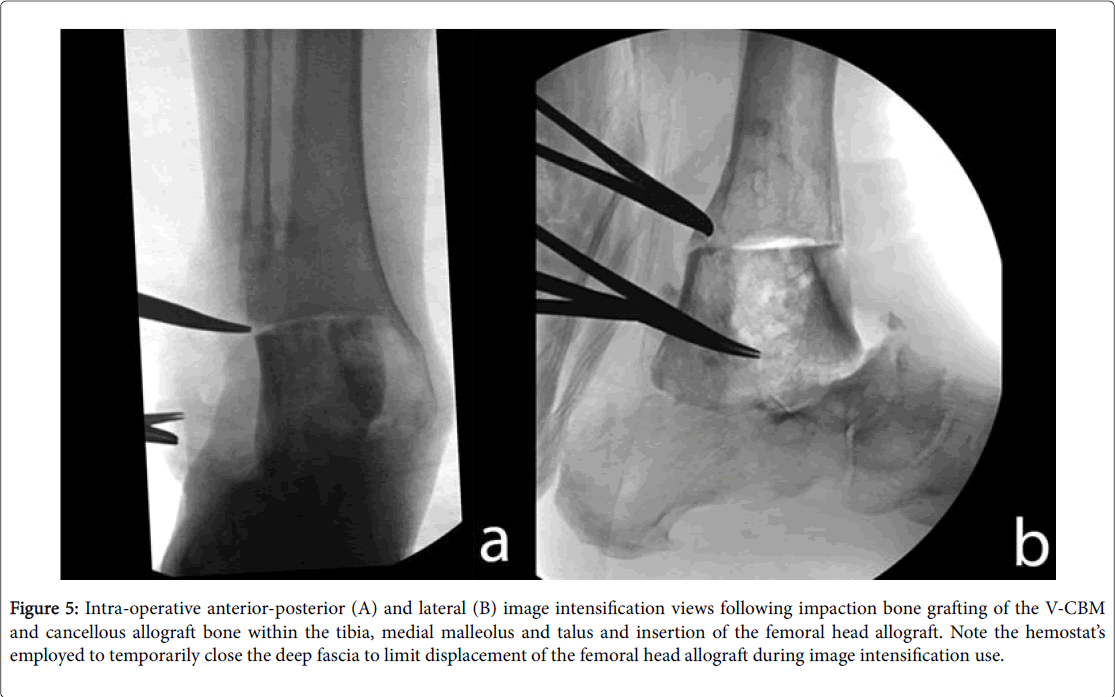
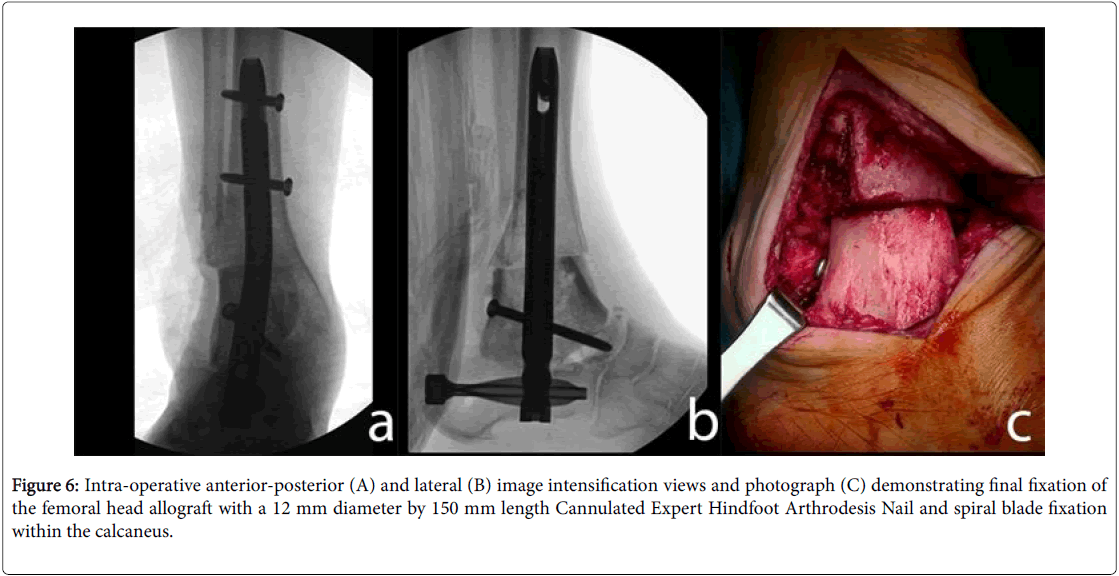
Surgery was performed 18 months after the failed revision agility total ankle replacement. Tourniquet time was 104 minutes. A lateral transfibular approach to the ankle and subtalar joints was taken (Figure 2). The fibula, including retained plate, was resected. The polyethylene insert was removed followed by the talar component with attached polymethylmethacrylate metal reinforced cement, then tibial tray removal (Figure 3). There was no osseous ongrowth to tibial or talar components. Bone resection was performed with hand instruments (currettes, osteotomes) and power tools (rotary burr, drill) to expose viable cancellous bone. A femoral head allograft underwent free-hand preparation to match the osseous defect. Ten cc of V-CBM (LifeNet Health, Virginia Beach, VA) was prepared as described as shown by Figure 4 and then impaction grafted into exposed bone surfaces, the osseous defect, and the femoral head allograft (Figure 5). A 12 mm diameter, 150 mm length Expert Cannulated Hindfoot Arthrodesis Nail (DePuy Synthes, West Chester, PA) and spiral blade were used for calcaneal fixation (Figure 6). Notably, V-CBM remained in place even after irrigation. There were no complications during the surgery.
Figure 2: (A) Intra-operative photograph upon entry into the ankle joint demonstrating copious amounts of metallic particulate wear debris in the anterior ankle recess. Following removal of the polyethylene insert, the talar component (B) and tibial tray (C) were grossly loose due to minimal osseous ongrowth to the components. Note the well-adhered polymethylmethacrylate metal reinforced cement affixed to the undersurface of the talar component.
Figure 4: (A) Intra-operative photograph demonstrating, from left to right, prepared femoral head allograft, bone marrow aspirate concentrate from the lateral calcaneus, and cancellous allograft bone chips harvested from the remaining portion of the femoral head allograft. Intraoperative photographs demonstrating initial infusion of the bone marrow aspirate concentrate into the V-CBM pouch (B, Top) and the final fully infused result (B, Bottom). Intra-operative photograph demonstrating, from left to right, V-CBM mixed with bone marrow aspirate concentrate, femoral head allograft infused with V-CBM and cancellous allograft bone chips mixed with bone marrow aspirate concentrate (C).
Figure 5: Intra-operative anterior-posterior (A) and lateral (B) image intensification views following impaction bone grafting of the V-CBM and cancellous allograft bone within the tibia, medial malleolus and talus and insertion of the femoral head allograft. Note the hemostat’s employed to temporarily close the deep fascia to limit displacement of the femoral head allograft during image intensification use.
Figure 6: Intra-operative anterior-posterior (A) and lateral (B) image intensification views and photograph (C) demonstrating final fixation of the femoral head allograft with a 12 mm diameter by 150 mm length Cannulated Expert Hindfoot Arthrodesis Nail and spiral blade fixation within the calcaneus.
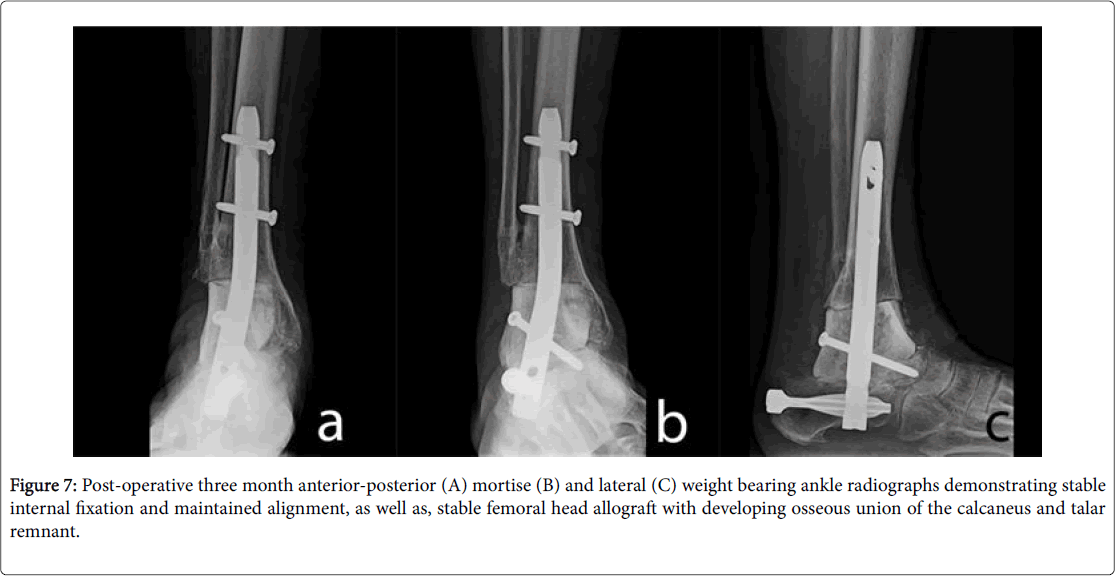
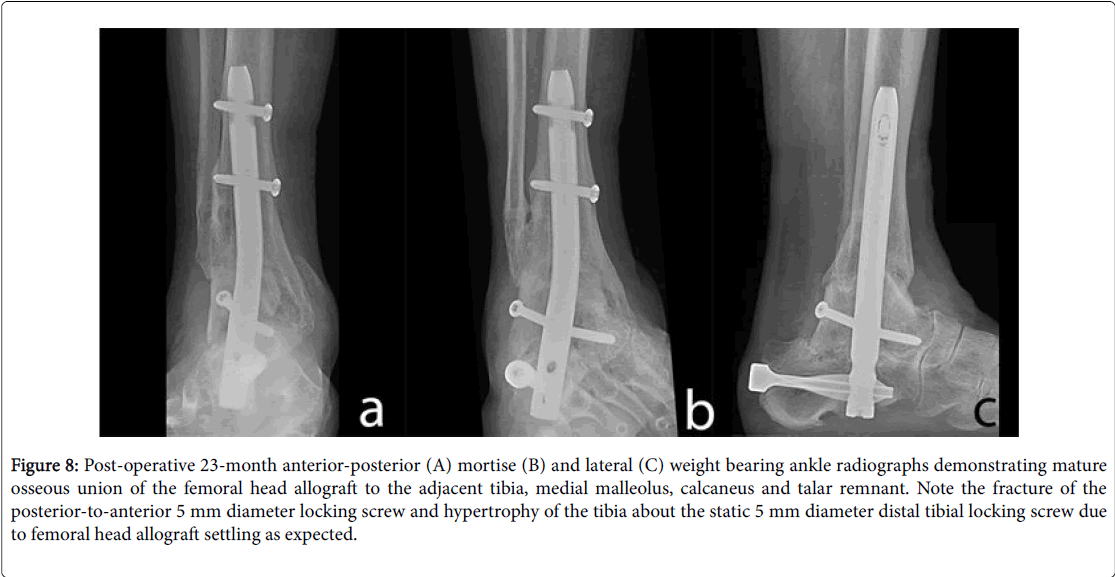
After 12 weeks, radiographs showed that the femoral head allograft was fusing to the native talus and calcaneus. After six months, the femoral head allograft was fused to native tibia (Figure 7). The patient was weight bearing at 5 months post-operative. The preoperative VAS 10 improved to a post-operative 3 in the midfoot/forefoot and no pain to the hindfoot/ankle. The patient was completely satisfied with procedure as of the last follow-up at 23 months post-operative (Figure 8). She does not use a brace, is able to use off-the-shelf shoe gear, and ambulates without a gait aide.
Figure 8: Post-operative 23-month anterior-posterior (A) mortise (B) and lateral (C) weight bearing ankle radiographs demonstrating mature osseous union of the femoral head allograft to the adjacent tibia, medial malleolus, calcaneus and talar remnant. Note the fracture of the posterior-to-anterior 5 mm diameter locking screw and hypertrophy of the tibia about the static 5 mm diameter distal tibial locking screw due to femoral head allograft settling as expected.
Discussion
While structural allografts have been used successfully to convert failed ankle arthroplasty to arthrodesis, the nonunion rates reported in the literature reveal the need for advanced treatments [8]. For example, bone marrow aspirate (BMA) and platelet-rich plasma (PRP) have been used to provide an autogenous source of growth factors. Multiple preclinical and clinical studies support the use of PRP to augment bone healing and reduce complications [9]. One preclinical in vivo study suggested BMA may have greater osseous integration potential over PRP, though clinical significance cannot be inferred [10]. In this case study, BMA and cancellous bone chips were combined with V-CBM with excellent results. Cancellous chips were added to enhance impaction bone grafting without negatively affecting V-CBM’s handling ability, which is especially important for tight bone voids.
Cellular bone allografts are the most recent advancement to promote fusion. A variety of cellular bone allografts have been developed with the goal of providing the osteoconductive, osteoinductive, and osteogenic properties essential for bone healing.
The majority of these allografts include MSCs that may differentiate into bone cells; however, there is concern that multipotent MSCs could erroneously differentiate into adipose, muscle, or cartilage cells [11]. In contrast, V-CBM contains differentiated osteogenic cells that are committed to forming bone tissue. The success of V-CBM in several different types of ankle and foot arthrodesis procedures [7] prompted its use in this complex case. V-CBM enabled a successful arthrodesis despite the complicated nature of this surgery in light of the two previous failures. The patient has remained satisfied with low level of pain after almost two years. This may be the first published case of a cellular bone allograft used in the salvage of a failed ankle arthroplasty.
Conclusion
Although the positive fusion results of this single case study are not generalizable, they do support continued research into the clinical use of V-CBM for arthrodesis procedures in the foot and ankle.
Declarations
Acknowledgements
Special thanks to Brian Samsell and Julie McLean, PhD (LifeNet Health) for writing assistance.
Conflict of interest
TR is a consultant for DePuy Synthes and received support for this work.
References
- Gougoulias NE, Khanna A, Maffulli N (2009) History and evolution in total ankle arthroplasty. Br Med Bull 89: 111-151.
- Makwana NK, Morrison P, Jones CB, Kirkup J (1995) Salvage operations after failed total ankle replacement. The Foot 5: 180-184.
- Lawton CD, Butler BA, Dekker RG, Prescott A, Kadakia AR (2017) Total ankle arthroplasty versus ankle arthrodesis-A comparison of outcomes over the last decade. J Orthop Surg Res 12: 76.
- Khan WS, Rayan F, Dhinsa BS, Marsh D (2012) An osteoconductive, osteoinductive, and osteogenic tissue-engineered product for trauma and orthopaedic surgery: How far are we? Stem Cells Int 2012: 236231.
- Reichert JC, Quent VM, Noth U, Hutmacher DW (2011) Ovine cortical osteoblasts outperform bone marrow cells in an ectopic bone assay. J Tissue Eng Regen Med 5: 831-844.
- Tortelli F, Tasso R, Loiacono F, Cancedda R (2010) The development of tissue-engineered bone of different origin through endochondral and intramembranous ossification following the implantation of mesenchymal stem cells and osteoblasts in a murine model. Biomaterials 31: 242-249.
- Roukis TS, Samsell B (2018) A New Approach to Ankle and Foot Arthrodesis Procedures Using a Living Cellular Bone Matrix: A Case Series. Clin Res Foot Ankle 6: 274.
- Berkowitz MJ, Clare MP, Walling AK, Sanders R (2011) Salvage of failed total ankle arthroplasty with fusion using structural allograft and internal fixation. Foot Ankle Int 32: 493-502.
- Smith SE, Roukis TS (2009) Bone and wound healing augmentation with platelet-rich plasma. Clin Podiatr Med Surg 26: 559-588.
- Stoker AM, Baumann CA, Stannard JP, Cook JL (2018) Bone marrow aspirate concentrate versus platelet-rich plasma to enhance osseous integration potential for osteochondral allografts. J Knee Surg 31: 314-320.
- Magnus MK, Iceman KL, Roukis TS (2018) Living Cryopreserved Bone Allograft as an Adjunct for Hindfoot Arthrodesis. Clin Podiatr Med Surg 35: 295-310.
Citation: Roukis TS (2018) Use of Living Cellular Bone Matrix for Treating a Failed Ankle Arthroplasty: An Abbreviated Technique and Case Study. Clin Res Foot Ankle 6: 282. DOI: 10.4172/2329-910X.1000282
Copyright: © 2018 Roukis TS. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 2786
- [From(publication date): 0-2015 - Nov 23, 2024]
- Breakdown by view type
- HTML page views: 2180
- PDF downloads: 606