Use of Intraoperative Frozen Section during Mediastinoscopy
Received: 21-Jun-2015 / Accepted Date: 13-Jul-2015 / Published Date: 15-Jul-2015 DOI: 10.4172/2161-0681.1000240
Abstract
Introduction: Staging of mediastinal lymph nodes (MLN) by mediastinoscopy can be of critical importance in assessing candidacy for lung resection. Mediastinoscopy is often performed as a sole procedure, with permanent pathology results guiding subsequent intervention. Our practice has been to perform mediastinoscopy followed by immediate surgical resection, as indicated, based on intraoperative frozen section (FS) assessment. The goal of our review is to evaluate the reliability of FS when compared to permanent section (PS) and to investigate any discordant findings. Materials and methods: A retrospective review of patients with lung cancer that underwent mediastinoscopy from June 2006 to January 2011. All received clinical staging according to NCCN guidelines and were considered potential candidates for surgical resection. Results for FS and PS of MLN were assessed. Results: Staging mediastinoscopy was performed on 191 patients, with a total of 549 MLN undergoing FS and PS analysis. Concordance between FS and PS was found in 545 MLN (99.3%). Discordance was found in 4 MLN (0.7%), each in a different patient. All 4 discordant MLN were initially negative on FS and then found to be positive on PS. Overall accuracy of FS analysis for detecting all malignancy was 97.9%, with 94.3% sensitivity, 100% specificity, 96.7% negative predicted value, and 100% positive predicted value. Conclusion: Our data suggest that for lung cancer patients with potentially resectable tumors, immediate FS analysis of MLN followed by definitive surgery is a reliable and safe strategy. Discordance with final pathology was rare (0.7%) and resulted in improper staging in 1 (0.5%) patient. Advantages of this “fast-track” approach include less medical costs and hastening of time from diagnosis/staging to definitive treatment.
Keywords: Mediastinoscopy; Lung cancer; Frozen section; Intraoperative; Staging
319926Introduction
Lung cancer remains the leading cause of death from cancer for men and women in the United States [1]. In those with suspected or diagnosed lung cancer, accurate disease staging is imperative for developing an appropriate treatment strategy. Despite advances in radiographic (e.g. CT, PET) and diagnostic (e.g. EBUS) methods, mediastinoscopy remains the most commonly employed procedure for mediastinal lymph node (MLN) sampling, as well as the ‘gold-standard’ modality [2,3] (Figure 1).
When mediastinoscopy is utilized to determine candidacy for surgical resection of lung cancer, many practitioners employ a ‘two-stage’ approach with mediastinoscopy first, followed by possible surgical resection days to weeks later after final pathologic assessment. For patients with low suspicion MLN on preoperative imaging, our practice has been to perform mediastinoscopy followed by immediate surgical resection, as indicated, based on intraoperative frozen section (FS) assessment of MLN. Central to this treatment strategy is reliance on the accuracy of intraoperative FS analysis of MLN to guide further intervention decision. However, sparse data exists on the accuracy of FS analysis in this setting. We therefore reviewed our experience with FS and permanent section (PS) pathologic assessment of MLN obtained with mediastinoscopy, to better interpret the benefits and limitations of this approach (Figure 2).
Materials and Methods
All staging mediastinoscopy procedures for potentially resectable lung cancer from August 2006 to January 2011 at the spartanburg regional medical center were reviewed. Most cases involved general surgery resident participation. Following IRB approval, we collected data on FS and PS diagnosis, number and station of lymph nodes collected, assessing pathologist, as well as patient characteristics such as age, comorbidities, and associated procedures.
Inclusion criteria included a diagnosis (pre, intra, or post-operatively) of small cell or non-small cell lung cancer (NSCLC), a completed mediastinoscopy procedure with sampling of at least one MLN, and assessment of lymph node(s) by both FS and PS. No cases were excluded from analysis.
At our institution, mediastinoscopy is recommended for: (1) patients with primary tumors>2 cm regardless of location in the lung; (2) suspected lung cancer patients with either CT evident mediastinal adenopathy (>1 cm) or PET avid MLN. Patients undergo induction of general anesthesia and are intubated with a single lumen endotracheal tube. A small transverse incision is created 1-2 cm above the manubrium and electrocautery is used to divide the platysma. The strap muscles are then identified and separated vertically in the midline. The pretracheal fascia is thus identified and divided, allowing for visualization of the anterior surface of the trachea. With assistance of a straight retractor, a rigid, lighted mediastinoscope (Wolf, Knittlingen, Germany) is then placed anterior to the trachea under direct visualization. The scope is advanced along the trachea under direct visualization to the level of the carina. Using blunt dissection with a long tip metal suction, appropriate lymph node stations are identified. Care is taken to avoid injury to the innominate artery, left recurrent laryngeal nerve, azygous vein, pulmonary artery and esophagus. We routinely sample lymph nodes from stations 4R, 4L, and 7 [4]. Stations 2R and 10 may also be accessed, as indicated by pre-operative imaging. Lymph nodes are dissected out bluntly, and retrieved with biopsy forceps. Areas of hemorrhage typically respond to gauze packing, with assistance of cellulose-based hemostatic sheets as needed (electrocautery is rarely used). Representative nodes from each station are sent for FS. With confirmed hemostasis, the mediastinoscope is withdrawn under direct vision and the wound closed with absorbable suture.
Upon arrival in pathology, the tissue is treated with Optimal Cutting Temperature Medium (Miles Laboratory, Elkhart, IN) and cooled with cryostat to -25°C. The specimen is divided into 40 µm and then 5 µm slices. It is then placed on a microfast slide, treated with alcoholic formalin for fixation, and processed with rapid hematoxllin and eosin staining. One or two slides are then evaluated by the attending pathologist, and if there is any doubt of the diagnosis additional slides are prepared and evaluated.
Results
During the study time period, 191 patients underwent mediastinoscopy with curative intent based on FS (Table 1). On final pathology, 71 patients (37.1%) had at least one positive MLN, while 120 patients (62.8%) had all negative MLN (Table 2). A total of 549 MLN were assessed by both FS and PS. Concordance between FS and PS was found in 545 MLN (99.3%). All four discordant MLN were initially read as negative on FS and involved four different patients. In each case of FN the MLN of interest contained scant metastatic disease. In this cohort, the overall accuracy of FS in diagnosing all MLN malignancy was 97.9%, with 94.3% sensitivity, 100% specificity, 96.7% negative predicted value, and 100% positive predicted value.
| Total Patients Male Female |
191 117 84 |
| Total MLN Harvested FS+ PS+ FS- PS- |
549 136 140 413 409 |
| Neoadjuvant Therapy Patients MLN Harvested FS+ PS+ FS- PS- |
8 21 1 2 20 19 |
| Additional Procedures: VATS/Pneumonectomy VATS/Lobectomy VATS/Wedge RATS/Lobectomy Thoracotomy/Pneumonectomy Thoracotomy/Lobectomy |
4 34 8 2 25 24 |
| VATS: Video Assisted Thoracoscopic Surgery; RATS: Robotic Assisted Thoracoscopic Surgery | |
Table 1: Patient characteristics.
| Diagnosis of MLN malignancy FS+ PS+ FS- PS- |
(patients) 67 71 124 120 |
| Sensitivity TP/(TP+FN) |
94.3% |
| Specificity TN/(TN+FP) |
100% |
| NPV TN/(TN+FN) |
96.7% |
| PPV TP/(TP+FP) |
100% |
| Accuracy (TP+TN)/(TP+TN+FP+FN) |
97.9% |
Table 2: Results.
MLN from stations 2R, 4R, 4L, 7, and 10R were harvested in our sample data. The median number of MLN sent for both FS and PS was two (range 1-10). No factors (e.g. patient age, reviewing pathologist) could be demonstrated as having association with FS/PS discordance.
Discussion
Mediastinal staging can be of critical importance in determining candidacy for surgical resection. In our practice, patients with mediastinoscopy rendered negative N2 and N3 MLN are considered candidates for surgical resection. Those patients found to be Stage IIIA on mediastinoscopy are considered for induction therapy (chemotherapy or chemoradiation) with potential for resection or definitive chemoradiation [5]. Those patients with mediastinoscopy proven Stage IIIB disease are not considered surgical candidates and receive definitive chemoradiation [6]. We prefer a “fast-track” of staging mediastinoscopy followed by resection for those patients with a low-suspicion mediastinum based on preoperative PET and CT imaging. Advantages include hastening the time interval from diagnosis to definitive treatment and avoiding two separate operative/anesthetic charges, as demonstrated by a prior report of 15% savings in total hospital charge [7]. Critical to this strategy is the necessary accuracy of FS analysis of MLN during mediastinoscopy. We sought to examine concordance between FS and PS in this setting in order to better evaluate the benefits and limitations of this diagnostic and management strategy.
Prior reports on this topic are limited [8]. A retrospective analysis by Gephardt and Rice [7] compared FS and PS diagnosis of MLN in 122 patients who underwent mediastinoscopy for bronchogenic carcinoma. Thirty-five patients had at least one lymph node with positive FS result, and there were two cases (1.6%) of false-negative FS as compared to PS (Table 3). All false-negative lymph nodes were noted to contain unifocal (microscopic) metastasis. Eight-seven patients underwent immediate thoracotomy based on FS diagnosis, for a calculated potentially avoidable thoracotomy rate of 2.3% (2/87). The authors conclude that FS evaluation is highly reliable in detecting metastatic carcinoma in mediastinal lymph nodes, as well as decreased cost of total hospital bill.
| Total MLN | Total Patients |
Sensitivity | Specificity | NPV | PPV | Accuracy | Potentially Avoidable Thoracotomy | |
|---|---|---|---|---|---|---|---|---|
| [1] | 549 | 191 | 94.3% | 100% | 96.7% | 100% | 97.9% | X |
| [7] | 620 | 122 | 94.6% | 100% | 97.7% | 100% | X | 2.3% |
| [9] | X | 136 | 94.5% | 100% | 90% | 100% | 96% | 2.3% |
| [10] | X | 420 | 99% | 100% | X | X | 99.4% | 2.6% |
| [11] | X | 343 | 75% | 100% | 94% | 100% | 95% | X |
| [12] | 161 | 36 | 94.5% | 100% | 99.1% | 100% | 99.2% | X |
| X - data unavailable | ||||||||
Table 3: Literature comparison
A similar experience was demonstrated by Sanli et al. [9], with a review of 136 patients undergoing mediastinoscopy for primary lung cancer, extrapulmonary cancers, and benign disease. There were five cases of false-negative FS, with four occurring in those with malignant disease and one in a patient with benign disease. There were 43 cases of immediate surgical resection following mediastinoscopy, with one instance of discordance between FS and PS among these patients, for a calculated potentially avoidable thoracotomy rate of 2.3% (1/43). Based on the high sensitivity and specificity, the authors conclude that a reliable decision may be made on proceeding to same-stage resection based on FS results.
Montpreville et al reviewed their experience with FS diagnosis of MLN in 420 patients, utilizing various biopsy methods including cervicotomy (12), mediastinotomy (43), manubriotomy (13), VATS (7) and mediastinoscopy (345) [10]. Tissue sampling was undertaken for a variety of suspected diagnoses in addition to lung cancer (e.g. lymphoma, sarcoid). Final diagnosis of bronchogenic carcinoma was obtained in 202 patients, with 179 samples obtained by mediastinoscopy. There were two instances of false negative FS diagnosis, for a sensitivity of 99% (200/202). There were 46 correct FS diagnoses of non-metastatic MLN, which were followed by immediate thoracotomy, 37 of which were for carcinoma. Both cases involved micrometastases. One of these two patients had previously received chemotherapy, and based on intra-operative FS diagnosis underwent thoracotomy, for a calculated potentially avoidable thoracotomy rate of 2.6% (1/38). In the second instance, the procedure was performed for suspected malignant effusion and no further procedures were planned. The authors conclude that FS can be very important for guiding possible resection of lung carcinoma.
A comparative evaluation of surgical staging and resection of lung cancer in one operation (combined) versus two operations (staged) was performed by Kim et al, utilizing FS diagnosis of MLN [11]. Ninety-eight patients had staged procedures. A combined approach was utilized in 319 patients, of which 286 underwent immediate thoracotomy. Of the 406 total patients that underwent mediastinoscopy, 21 (5.2%) had false negative FS diagnosis, 7 (1.7%) had more extensive N2 disease discovered at thoracotomy, and 14 (3.4%) had N2 disease at thoracotomy not accessible to mediastinoscopy. The authors conclude that if requirements for accurate clinical staging (rigorous mediastinoscopy, efficient histologic evaluation) are met, a combined strategy should be offered to any patient that is medically operable and has clinical stage I or II NSCLC.
Clarke et al. compared FS to imprint cytology (IC) in diagnosing MLN obtained by mediastinosocpy [12]. The FS group included 36 patients, with 24 undergoing staging for lung cancer. There was one false-negative finding in a patient who was accurately classified based on another true-positive node diagnosed by FS at the time of mediastinoscopy. Accurate staging was obtained in 23 of the 24 patients evaluated for lung cancer, with 12 patients undergoing immediate surgical resection. The authors found similar results with IC as compared to FS, and confirm IC to be a useful method of rapid MLN diagnosis.
Of the 549 MLN undergoing FS analysis in our series, there were four instances of nodal discordance, each in a different patient. The first case involved a suspicious PET-avid left upper lobe mass with PET positive contralateral mediastinum, suspected clinical stage IIIB. At the time of mediastinoscopy, FS analysis suggested positivity for SCLC at nodal station 4R and negative for tumor at station 7, rendering the patient not a surgical candidate. Subsequent final pathology confirmed positivity for cancer at 4R and also at 7. It was noted by the evaluating pathologist that small collections of metastatic tissue were found on deeper sections of the specimen. This patient received definitive chemoradiation and the false-negative report at the time of mediastinoscopy did not alter the patient’s eventual treatment plan.
The second case involved a patient with clinical stage IIIA biopsy-proven right lower lobe NSCLC, status-post neoadjuvant chemo-radiation therapy. At mediastinoscopy, FS analysis suggested multiple negative nodes at stations 4R and 7 (station 4L was unable to be obtained). The patient then underwent immediate surgical resection of the right lower lobe. Upon PS analysis, one of the two 4R MLN was positive for NSCLC, with a small focus of viable residual metastatic tumor identified.
In the third case, mediastinoscopy was performed on a patient with a suspicious right lower lobe mass. Intra-operative FS analysis suggested positivity for NSCLC in one of two station 7 MLN; final PS pathology was positive for disease in both nodes, with a small rest of tumor cells identified in a vascular space on the lymph node initially diagnosed as negative. The patient did not undergo surgery and was treated with chemo-radiation therapy.
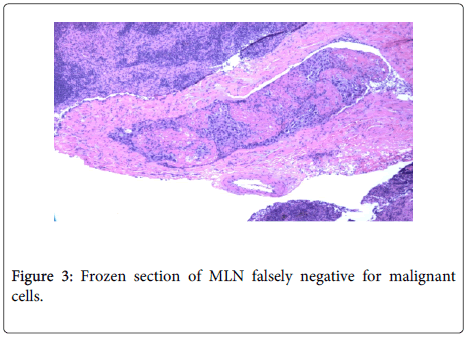
The fourth instance occurred in a patient with diffuse mediastinal adenopathy. Frozen section analysis suggested NSCLC at stations 4R and 7, but negative 4L. PS revealed NSCLC at all three stations with microscopic foci of adenocarcinoma at 4L. No additional procedures were performed at the time of mediastinoscopy. This false-negative FS was an instance of inaccurate staging based on frozen section result alone (3A versus 3B) (Figure 3).
Further review of pathology specimens associated with false-negative FS result was performed. In one case there was a very small focus of tumor in the FS which was missed. In the remaining cases, there was very little tumor present in the MLN, none of which was represented on the FS tissue slices but subsequently identified on PS review.
Our data suggest that for lung cancer patients with potentially resectable tumors, immediate FS analysis of MLN followed by definitive surgery is a reliable and safe strategy. Additionally, analysis of our series demonstrates the importance of thorough MLN sampling, as inaccurate intra-operative staging was prevented in two of the four cases of discordance due to positive findings in additional lymph nodes. One major advantages of this approach includes hastening the time from initial presentation to diagnosis/staging to definitive treatment. Additionally, potential cost savings exist with this “fast-tracking” through the mediastinal staging process as patients incur only one anesthetic/operating room charge. The major disadvantage is the risk of false negative FS resulting in upfront surgical resection, as opposed to neoadjuvant therapy or definitive chemoradiation. Compared to other studies, our rate of false negative FS effecting therapy change was low (1 patient, 0.5%) and we feel the advantages as mentioned above outweigh this small risk.
References
- (2012) National Cancer Institute, Surveillance Epidemiology and End Results (SEER) Cancer Statistics Review 1975-2009.
- Medford AR, Bennett JA, Free CM, Agrawal S (2009) Mediastinal staging procedures in lung cancer: EBUS, TBNA and mediastinoscopy. CurrOpinPulm Med 15: 334-342.
- Mountain C, Dresler C (1997) Regional Lymph Node Classification for Lung Cancer Staging. Chest 111:1718-1723.
- NCCN Clinical Guidelines in Oncology, Non-Small Cell Cancer, Version 2.2013, NCCN.org, NSCLC-7.
- NCCN Clinical Guidelines in Oncology, Non-Small Cell Cancer, Version 2.2013, NCCN.org, NSCLC-10.
- Gephardt G, Rice T (1990) Utility of frozen-section evaluation of lymph nodes in the staging of bronchogenic carcinoma at medistinoscopy and thoracotomy. J ThoracCardiovasSurg 100:853-859.
- Attaran S, Jakaj G, Acharya M, Anderson JR (2013) Are frozen sections of mediastinoscopy samples as effective as formal paraffin assessment of mediastinoscopy samples for a decision on a combined mediastinoscopy plus lobectomy? Interact CardioVascThoracSurg 16: 872-874.
- Sanli M, Isik AF, Tuncozgur B, Akar E, Deniz H et al. (2008) The reliability of mediastinoscopic frozen sections in deciding on oncologic surgery in bronchogenic carcinoma. AdvTher 25: 488-495.
- Montpreville VT, Dulmet E, Nashashibi N (1998) Frozen section diagnosis and surgical biopsy of lymph nodes tumors and pseudotumors of the mediastinum. Eur J CardiothoracSurg13: 190-195.
- Kim K, Rice TW, Murthy SC, DeCamp MM, Pierce CD, et al. (2004) Combined bronchoscopy, mediastinoscopy, and thoracotmy for lung cancer: Who benefits? J ThoracCardiovasSurg127:850-856.
- Clark M, Landreneau R, Borochovitz D (1994) Intraoperative Imprint Cytology for Evaulation of Medistinal Lymphadenopathy. Ann ThoracSurg 57:1206-1210.
Citation: Perry PA, Hird BR, Orr RK, Nguyen CL (2015) Use of Intraoperative Frozen Section during Mediastinoscopy. J Clin Exp Pathol 5:240. DOI: 10.4172/2161-0681.1000240
Copyright: © 2015 Perry PA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 19866
- [From(publication date): 8-2015 - Apr 07, 2025]
- Breakdown by view type
- HTML page views: 15198
- PDF downloads: 4668