Research Article Open Access
Use of Cuban Granulated B-Tricalcium Phosphate “Biograft-G” as Maxilar Bone Graft
Pérez Alvarez MC1,2*, Delgado García-Menocal JA2, Almirall La Serna2, Alfonso HA2, Collins J3, Fernández Díaz MI1, Márquez AD1, Rodríguez Hernandez JA1, Rodríguez CO4, Somonte Dávila H5, Guerra Bretaña RM2 and Morejón AL2
1Clínica Stomatological Faculty of Bauta, Bauta, Cuba
2Center for Biomaterials, University of Havana, Ave Universidad, Havana, Cuba
3Escuela Graduate Dentistry, Catholic University of Santo Domingo, Dominican Republic
4Hospital General Surgical Clinical Teaching, “Aleida Fernandez Chardiet” Guines, Artemisa, Cuba
5Hospital General Surgical Clinical Teaching, “Leon Cuervo Rubio”, Pinar del Rio, Cuba
- *Corresponding Author:
- Mayra de la Caridad Pérez Álvarez
Center for Biomaterials
University of Havana
Ave Universidad, Havana Cuba
Tel: +53 47 374197; +53 5237-1238
E-mail: dntimefa@infomed.sld.cu
Received Date: April 30, 2013; Accepted Date: May 25, 2013; Published Date: May 28, 2013
Citation: Pérez Alvarez MC, Delgado García-Menocal JA, Almirall La Serna, Alfonso HA, Collins J, et al. (2013) Use of Cuban Granulated B-Tricalcium Phosphate “Biograft-G” as Maxilar Bone Graft. J Oral Hyg Health 1:103. doi: 10.4172/2332-0702.1000103
Copyright: © 2013 Pérez Alvarez MC, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Oral Hygiene & Health
Abstract
In maxillary bone, several pathologies or lesions may cause maxillary alveolar atrophic (MAA), that is, a bone reabsorption frequently provoked by tooth loses or extractions. Tooth loses or extractions are one of the most common clinical situations observed in patients. The MAA could become a signifi cant functional and aesthetic risk for the use of tooth implants or any other prosthetic rehabilitation. Several biomaterials have been used as bone graft; they must fulfi l requirements like biocompatibility and a suitable function. A synthetic dense ceramic granulate of β-TCP, BIOGRAFT-G® (BIOMAT), in form of irregular shape granules with a grain size between 0.1 mm and 0.4 mm, was used in this study as graft material. The clinical studies include 178 patients, treated in Pre-implantology and Trans-implantology bone remodelling, prevention of residual ridge reabsorption by socket grafting and Periapical Surgical. In the fi nal evaluation of effectiveness after 6 month of surgery most of cases were qualifi ed as Success (98.3%), observing in the treated site a remodeled bone similar to the one in the adjacent tissue and almost no trace of implanted biomaterial. However, 3 cases were qualifi ed as Failure, all of them in patients that underwent the fi lling of dental sockets treatment, caused by the exfoliation of granules or a septic process. According to the obtained results, Biograft-G® proved to be a biodegradable, biocompatible, effectiveness and safety bone graft biomaterial in the studied treatments.
Keywords
β-tricalcium phosphate; Bone defects; Bone repairing; Oral surgery; Pre-implantology surgery; Bone filling
Introduction
The only adult human tissue with the capability of whole regeneration is bone tissue. However, in some cases depending on the defect type and the bone lesion cause, the bone regeneration could be a complex and delayed process [1].
In maxillary bone, several pathologies or lesions may cause Maxillary Alveolar Atrophic (MAA), that is, a bone reabsorption frequently provoked by tooth loses or extractions, which is a very common clinical situation observed in patients. The MAA could become a significant functional and aesthetic risk for the use of tooth implants or any other prosthetic rehabilitation [2,3]. According to several reports, mayor dimensional changes on the alveolar ridge take place during the three first months after tooth extraction, and can be treated with different surgical procedures and bone graft materials [4,5].
Currently, one the surgical procedures most requested by patients after a tooth extraction is the use of metallic implants. This surgical method allows the prevention of MAA when used immediately after tooth extraction and requires the use of a graft material in order to fix the metallic implant. In other cases the recommended treatment is to fill the cavity to achieve a bone remodelling after the placement of a metallic implant. The selection of the appropriate treatment in each case, as well as the suitable biomaterials to be used, must be done by a qualified physician [6-8].
Several biomaterials, that must fulfil requirements such as biocompatibility and a suitable function, have been used as graft material. During the 80´s and 90´s the Hydroxyapatite (HA) was the most common biomaterial used as graft. Once implanted, the HA provides support for new bone growth, allowing the filing of the defect, even in those cases where the bone cannot usually regenerate by itself. Though there is bone regeneration, the permanence of HA due to its stability increases the mechanical strength in the site causing some inconveniences for the placement of endosseous implants [3,9]. For this reason, new biodegradable materials started to be used. This is the case of β-Tricalcium phosphate (β-TCP), a graft biomaterial which has been proved to allow new bone growth and site consolidation in bone defect while the material degrades [1,10].
Employing HA or β-TCP graft in the form of granule material also requires the use of membranes in order to maintain the implanted material in the correct position [11]. Membranes help the bone regeneration process and avoid the interference of soft tissues on the bone cicatrisation, and could be made of polylactic/polyglicolic acid or collagen [12].
Biograft-G® is a synthetic ceramic granulate of β-TCP for bone regeneration, manufactured by the Centro de Biomateriales de la Universidad de la Habana (Biomaterials Centre at the Havana University, BIOMAT). This material has proved to be non cytotoxic, bioactive and biocompatible, according to preclinical and clinical essays [13-15]. This study presents the effectiveness of Biograft-G® as bone graft in pre-implantology remodelling, trans-implantology remodelling, filling of dental sockets and periapical bone defects.
Materials and Methods
A synthetic dense ceramic granulate of β-TCP, BIOGRAFT-G® (BIOMAT), was used in this study in the form of irregular shape granules with a grain size between 0.1 mm and 0.4 mm.
The clinical studies included 178 patients treated with BIOGRAFT-G® to prevent MAA and periapical surgery. All patients gave their informed consent, according to Helsinki Statement. Treatments were carried out in several public dental services in Cuba (in La Habana, Pinar del Rio, Matanzas and Artemisa provinces) and in the city of Santo Domingo, Dominican Republic, between 2009 and 2013. Patients included in these studies were categorized according to the World Health Organization as 0 and 1 general state of health and in a range of age between 18 to 70 years old.
Treatments were classified as Pre-implantology and Trans-implantology bone remodelling, prevention of residual ridge reabsorption by socket grafting and Periapical Surgical.
In all cases, the surgical treatments and toilette of the bone defect were carried out using the conventional method before the refilling with Biograft-G®. The graft material was mixed with sterile water or the patient’s blood before placing it and then covered with a collagen membrane to prevent particle migration [11]. After restoring the mucoperiosteum and the flap, the surgical incision was sutured with 3.0 silk suture and with tissue adhesive Tisuacrylâ (BIOMAT) [16].
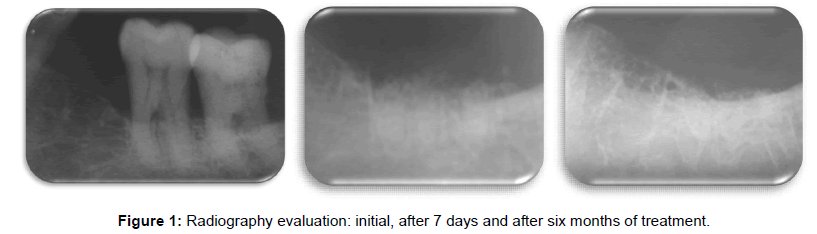
Clinical and radiographic evaluation of the treatment effectiveness was carried out. Clinical evaluation includes: presence of edema, granule exfoliation and presence of infection. The presence of edema was qualified, according to the increase of mucous volume noticed, as Absence for no increase, Slight for a small or medium increase and Severe for a large increase of mucous volume. Granule exfoliation was evaluated as Absence or Occurrence. The presence of infection was evaluated as Absence or Occurrence in accordance with the appearance or not of suppuration. Radiographic evaluation was made in seven days and after six months of implantation and qualified as Satisfactory (more than 80% of filled cavity with radiopacity) or Not Satisfactory (less than 80% of filled cavity with radiopacity).
Treatment effectiveness was qualified as Success or Failure.
Success: when there was absence of edema, infection and granule exfoliation and radiographic evaluation was satisfactory.
Failure: when at least one of the evaluation parameters don’t fulfil the previously mentioned requirements.
Results and Discussion
Patient distribution by sex, age and surgical treatment are shown in table 1. The most common treatment was the filling of dental sockets, in almost 61% of the cases treated. No significant differences on results according to sex and age groups were observed.
| Control variables | Quantity | Percentage |
|---|---|---|
| Sex | ||
| Female | 92 | 52,8 |
| Male | 86 | 47,2 |
| Age Groups | ||
| 18-44 | 86 | 48,3 |
| 45-70 | 94 | 51,7 |
| Surgical interventions | ||
| Pre-implantology remodelation | 34 | 19,1 |
| Trans-implantology remodelation | 19 | 10,7 |
| Filling of dental sockets | 108 | 60,7 |
| Periapical Surgical | 17 | 9,6 |
| Total | 178 | 100 |
Table 1: Patient distribution by sex, age and surgical treatment.
At short time evaluation, after seven days of the treatment was carried out, 94.4% of successful cases were observed. There was no infection or presence of dental plaque in any of the cases. However, in patients that underwent the treatment of dental socket filling, the presence of edema was reported in 10 cases and granules exfoliation in 2 of them, while the other treatments did not report any adverse effect.
The presence of edema in a short time may occur as a natural consequence of the surgical intervention, but granules exfoliation should be caused by an incorrect handling of the graft material or the incorrect placement of collagen membrane during the surgical treatment. Similar observations have been reported by other authors, e.g. Kalish et al. [17], that attribute the granules exfoliation to the handling difficulties, mainly due to the lack of cohesion typical on this kind of materials supplied in granule form.
It should be noticed that in cases of implantology remodelling and periapical surgery, the bone cavities has less tendency to present exfoliation of granules due to a more closed shape, in accordance with the results observed in this and other studies [18-21].
In the final evaluation of effectiveness, after 6 months of surgery, most of the cases were qualified as Success (98.3%), observing in the treated site a remodeled bone similar to the one in the adjacent tissue and almost no trace of implanted biomaterial. All Implantology remodelling and periapical surgery treatments were qualified as Success. Only 3 cases were qualified as Failure, all of them in patients that underwent the treatment of dental sockets filling. Failures reported were caused by the exfoliation of granules in 2 of the cases and the other one due to a septic process adjacent to the alveolus that caused the treatment failure after 3 months. These results are similar to the ones reported by other authors [22] that consider the placement of β-TCP P as graft for bone remodelling in dental implants, combined with a reabsorbable membrane, an implantology success treatment.
Figure 1 show radiography of post extraction alveolus after 7 days and 6 months of surgery; at a short time the biomaterial placed could be observed, while after 6 months a newly form bone that allows keeping the desired bone height is observed.
At the end of the study (six months), only a few traces of the material could be seen in the X-ray films images, observing the almost absence of Biograft-G® in the implanted site. Several authors agree that filling dental sockets with bone graft biomaterials at the moment of the tooth extraction to preserve alveolar morphology is an effective treatment to prevent the bone reabsorption and MAA [23-27].
Conclusions
Bone treatments with Biograft-G® demonstrate to be effective in Pre-implantology and Trans-implantology bone remodelling, prevention of residual ridge reabsorption by socket grafting and Periapical Surgical, observing in the treated site a remodeled bone similar to the one in the adjacent tissue and almost no trace of implanted biomaterial after six months. According to the obtained results, Biograft-G® proved to be a biodegradable, biocompatible, effectiveness and safety bone graft biomaterial in the studied treatments.
Acknowledgements
The authors thank the Public Health Cuban Ministry for supporting this work. We also thank the collaboration of the University of Barcelona, Spain.
References
- Dubraska SV (2012) Basic principles guided bone regeneration. Acta Clínica 2: 89-116.
- Pérez M, Delgado J, Viloria GJV, Guerra R, Ortega JJ (2011) Biological response between hydroxyapatite and tricalcium betafosfato in regenerating bone tissue. Acta Bioclinica 1:2.
- Ford Martinell VL, Hanly G, Valenzuela J, Orozco LMH, Zapata SM (2012) Alveolar ridge preservation?: Decision making for dental implant placement. Rev CES Odont 25: 44-53.
- Hämmerle CH, Araújo MG, Simion M; Osteology Consensus Group 2011 (2012) Evidence-based knowledge on the biology and treatment of extraction sockets. Clin Oral Implants Res 23: 80-82.
- Misch CE, Silc JT (2008) Socket grafting and alveolar ridge preservation. Dent Today 27: 146.
- Lang NP, Pun L, Lau KY, Li KY, Wong MC (2012) A systematic review on survival and success rates of implants placed immediately into fresh extraction sockets after at least 1 year. Clin Oral Implants Res 23: 39-66.
- Darby I, Chen ST, Buser D (2009) Ridge preservation techniques for implant therapy. Int J Oral Maxillofac Implants 24: 260-271.
- De Coster P, Browaeys H, De Bruyn H (2011) Healing of extraction sockets filled with BoneCeramic® prior to implant placement: preliminary histological findings. Clin Implant Dent Relat Res 13: 34-45.
- García-Roco Pérez O (2002) Developments in the treatment of alveolar atrophy. Rev Cub Estomat 392: 55-58.
- Galindo P, Sánchez E, Ávila G (2005) Protocolo en sustitutos óseos. Protocolos y guías de práctica clínica en cirugía bucal. [en línea] Sociedad Española de Cirugía Bucal. (SECIB).
- Brkovic BM, Prasad HS, Rohrer MD, Konandreas G, Agrogiannis G, et al. (2012) Beta-tricalcium phosphate/type I collagen cones with or without a barrier membrane in human extraction socket healing: clinical, histologic, histomorphometric, and immunohistochemical evaluation. Clin Oral Investig 16: 581-590.
- Vignoletti F, Matesanz P, Rodrigo D, Figuero E, Martin C, et al. (2012) Surgical protocols for ridge preservation after tooth extraction. A systematic review. Clin Oral Implants Res 23: 22-38.
- Fernandez DR, Velez UJ, Sosa VR, Carrodeguas RG, Pelayo ZC, et al. (2006) Pathologic evaluation experimental implementation in bone of synthetic hydroxyapatite (Apafill-G). Rev Hab Cienc Méd 54: 11-14.
- Delgado Fernández R, Urbizo Vélez J; Rodríguez Sosa V; Iglesias Rodríguez E (2010) Evaluación de la respuesta hística del beta fosfato tricálcico (Biograft-G) como implante óseo. Rev Cubana Estomatol 47: 124-133.
- Registro Médico Reglamento para la Evaluación y el Control Estatal de Equipos Médicos. Resolución Ministerial No. 184 del MINSAP. Aprobado: 2008.09.22. Gaceta Oficial (CU) 22: 1424–36.
- Pérez M, Fernández I, Márquez D, Bretaña RM (2000) Use of N-butyl-2-cyanoacrylate in oral surgery: biological and clinical evaluation. Artif Organs 24: 241-243.
- Kalish BP, Schuster GS, Peacock ME, Cuenin MF, Swiec GD, et al. (2008) Influence of matrix-suspended demineralized bone on osseous repair using a critical-sized defect in the rat (Rattus norvegicus) calvarium. J Oral Implantol 34: 83-89.
- Álvarez MC, Carrodeguas R, Delgado JA, Fernández I, Márquez D, et al. (1998) Implantation of cuban granulated hydroxyapatite “Apafill-G” in periapical bone defects. Bioceramics. New York, USA.
- García D, García L, Pérez MC, Suarez M, Delgado JA, et al. (2001) Filling of Post-Extraction Dental Socket with Hydroxyapatite Granules APAFILL-G™". Key Engineering Materials. Trans Tech Publications, Switzerland.
- Álvarez MC, Delgado JA, García R, Fernández I, Márquez D, et al. (2007) Generalización en Cuba del Apafill-G para estomatología. Premio Anual de Salud 2006. Edt. Ciencias Médicas.
- Pérez MC (2011) Behavior bone implanted dental alveoli Biograft-G®. Evolution of cases at 6 months.
- Duck MJ, Jiménez GA, Monsalve GL, Segura EJJ, Velasco OE (2010) Guided bone regeneration with nanosurface single-tooth implant and beta-tricalcium phosphate. Adv Periodon Implantol 22: 127-134.
- Fickl S, Zuhr O, Wachtel H, Bolz W, Huerzeler MB (2008) Hard tissue alterations after socket preservation: an experimental study in the beagle dog. Clin Oral Implants Res 19: 1111-1118.
- Cardaropoli D, Cardaropoli G (2008) Preservation of the postextraction alveolar ridge: a clinical and histologic study. Int J Periodontics Restorative Dent 28: 469-477.
- Araújo M, Linder E, Wennström J, Lindhe J (2008) The influence of Bio-Oss Collagen on healing of an extraction socket: an experimental study in the dog. Int J Periodontics Restorative Dent 28: 123-135.
- Barone A, Aldini NN, Fini M, Giardino R, Calvo Guirado JL, et al. (2008) Xenograft versus extraction alone for ridge preservation after tooth removal: a clinical and histomorphometric study. J Periodontol 79: 1370-1377.
- Wang HL, Tsao YP (2008) Histologic evaluation of socket augmentation with mineralized human allograft. Int J Periodontics Restorative Dent 28: 231-237.
Relevant Topics
- Advanced Bleeding Gums
- Advanced Receeding Gums
- Bleeding Gums
- Children’s Oral Health
- Coronal Fracture
- Dental Anestheia and Sedation
- Dental Plaque
- Dental Radiology
- Dentistry and Diabetes
- Fluoride Treatments
- Gum Cancer
- Gum Infection
- Occlusal Splint
- Oral and Maxillofacial Pathology
- Oral Hygiene
- Oral Hygiene Blogs
- Oral Hygiene Case Reports
- Oral Hygiene Practice
- Oral Leukoplakia
- Oral Microbiome
- Oral Rehydration
- Oral Surgery Special Issue
- Orthodontistry
- Periodontal Disease Management
- Periodontistry
- Root Canal Treatment
- Tele-Dentistry
Recommended Journals
Article Tools
Article Usage
- Total views: 13979
- [From(publication date):
July-2013 - Nov 21, 2024] - Breakdown by view type
- HTML page views : 9546
- PDF downloads : 4433