Use of a Wellness Coaching Model among Urban-dwelling, Low-income Older Adults
Received: 12-Aug-2019 / Accepted Date: 01-Oct-2019 / Published Date: 07-Oct-2019 DOI: 10.4172/2471-9846.1000232
Abstract
Objective: The purpose of this pilot project was to employ a goal-based, individualized behavior-change approach to promote engagement in health care self-management activities and physical activity among vulnerable older adults living in subsidized housing. The specific aims were: (1) to determine the acceptability and feasibility of a wellness coaching model among urban-dwelling, low-income older adults, and (2) to test whether participation in the wellness coaching program would result in higher activation levels, increased physical activity, and an improved, self-rated quality of life and health status when compared to a wait-list control group.
Methods: The project implemented a feasibility study and quasi-experimental design to achieve its aims. The sample included minority older adults residing in one of two subsidized housing sites, both within one large, urban housing authority. Fifteen participants (5 females and 10 males, mean age 77.4 ± 7.9 years) were assigned to the intervention group and 13 older adults (7 females and 6 males, mean age 75.8 ± 9.1 years) from another housing site comprised the wait-list control group, crossing over to the intervention after six months. The intervention was an integrative, geriatric assessment and wellness coaching program introduced to low-income older adults. InterRAI’s Health & Social Check-up and the Lifestyle Survey were the primary data collection tools. Participants also completed the Patient Activation Measure.
Results: Independent t-tests revealed statistically significant improvement in physical activity and self-reported health status and quality of life for the group receiving the intervention for one year compared with those who received the intervention for a short time period.
Conclusion: Urban-dwelling, low-income older adults were able to identify their goals and, through a wellness coaching process, engage in the development of their personal healthy aging plan, facilitating their involvement in health care self-management. Capitalizing on social networks and other low or no-cost options to support goal achievement may be a key strategy in resource-restricted environments.
Keywords: Patient activation; Personalized wellness coaching; Physical activity; Self-management; Low-income older adults; Senior housing, InterRAI
Introduction
At an increasing rate, both rich and poor older adults are living longer despite the presence of chronic disease and illness [1]. The number of older adults, age 65 years or over and currently representing 14.5% of the United States (US) population, is projected to more than double to 98 million by 2060 [2]. The older adults are more likely to experience repeated hospitalizations and/or unplanned visits to their health care provider, while facing increased costs to manage their health [3]. Prolonged life, though desired by many, brings new challenges. Many older adults struggle to maintain quality of life and independence in the presence of complex, chronic diseases and prevailing illness symptoms. With limited access to key resources and support, these challenges are even more profound.
Over 4.5 million (10%) U.S. older adults live below the poverty level with another 2.4 million (5.3%) classified as “near-poor” having an income up to 125% of the poverty level [1]. Low-income elders are a diverse and complex group of older adults who have socioeconomic stressors, low health literacy, chronic co-morbidities, and limited access to health care [4]. They are twice as likely to rate their health as fair or poor (57%) compared to elders in other community settings (27%) [5]. In contrast to higher-income groups, the poorer population in the US continues to experience significant disparities in health and health care [6].
An estimated 6% of adults over 61 years old and, predominantly single women, live in subsidized housing [7]. These vulnerable seniors tend to be more challenged than older adults in general and are at greater risk of having unmet needs [8]. The incidence of pain, depression, chronic disease, and disability is increased among lowincome older adults who often have limited access to care providers to help manage these problems [9-14].
Sufficient evidence exists on promising health-promoting interventions and self-management programs targeting older adults [15,16]. However, one of the primary challenges is motivating people to adopt and sustain behaviors promoted within these programs. By nature of their living environment, low-income older adults in subsidized housing may be well positioned to engage in efforts towards adopting and sustaining health-promoting interventions. Accessing proper community organizations and resources, this particular population may benefit from self-sustaining health interventions. As the US healthcare system continues its efforts towards becoming an efficient, cost-effective model, there is a critical need to provide all persons, and particularly, low-income older adults, with support to promote their independence, enable them to adopt healthy life-style choices, assume responsibility for their own disease management, and ultimately attain an improved quality of life. This outcome is central to the successful aging model.
Theoretical Framework
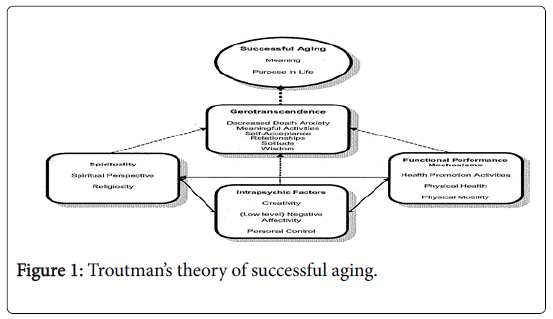
Supporting successful aging requires a personal, multi-factorial approach involving the older adult, significant others, and care providers. Based on Tornstam’s theory of gerotranscendence (1996) and the Roy adaptation model (1984), Troutman developed a midrange level nursing theory of successful aging. Troutman’s theory of successful aging involves three coping processes: 1. functional performance mechanisms, 2. spirituality, and 3. intra-psychic factors [17]. Functional performance mechanisms refer to the use of conscious awareness and choice as an adaptive response to physiologic and physical aging. Spirituality consists of the person’s beliefs and views that relates to something greater than self. Innate features that contribute to the person’s ability to adapt to change and solve problems serve as the basis for the intrapsychic factors. Each of the three processes contribute to the complex process of gero-transcendence and, ultimately, successful aging (Figure 1).
Presently, health care is structured on potential or existing patient problems with care directed towards prevention or management of disease states. Geriatric care, in particular, applies the translation of decades-long scientific research focused on disease states or clinical symptoms. Most previous research efforts have pursued isolated body systems (e.g. cardiac, renal, endocrine); yet an older adult’s daily function is dependent upon effective symbiotic relationships among multiple physical systems. Intertwined within these relationships are the psycho-social, intra-personal, and spiritual elements that have started to receive attention in healthcare and relevant research efforts.
When the older adult is provided opportunity to select health care options and lifestyle strategies that align with their self-identified goals, a comprehensive and holistic approach to successful aging is underway. Formally implemented health care programs that follow this approach are notably absent from the current formal health care system. With an expanding aging population accessing an already strained health care delivery system, new models that assume a person-centered, holistic approach directed towards promoting successful aging among all older adults need to be implemented and evaluated. The purpose of this pilot project was to employ a goal-based, individualized behavior-change approach to promote engagement in health care self-management activities and physical activity among vulnerable older adults living in subsidized housing. The specific aims were: (1) to determine the acceptability and feasibility of a wellness coaching model among urban-dwelling, low-income older adults, and (2) to test whether participation in the wellness coaching program would result in higher activation levels, increased physical activity, and an improved, self-rated quality of life and health status when compared to a wait-list control group.
Materials and Methods
Study design
The project implemented a feasibility study and quasi-experimental design to achieve its aims. An integrative, geriatric assessment and wellness coaching program was introduced to low-income older adults residing in subsidized housing within one large, urban housing authority. Originally developed for older adults residing in continuing care retirement communities, [18], the investigator adapted the wellness coaching program for implementation in a resource restricted environment. The process for the wellness coaching began with an individualized comprehensive assessment. Then, a summarization of the assessment framed the collaboration and conversation with one wellness coach to establish the participant’s life goals and create a healthy aging plan, an individualized road map delineating specific activities directed at personal goal achievement. The healthy aging plan guided subsequent discussions that occurred during the weekly contacts by the wellness coach. The study was approved by the IRB committee of the primary university for this project.
Tools: InterRAI assessment tools, the Health and Social Check-up (HSC) and the Lifestyle Survey (LS), and the Patient Activation Measure (PAM) 10 measurement instrument were used in this project. InterRAI assessment tools are based on a common metric to measure major questions of interest [19] with established validity and reliability [20,21]. The HSC contains a comprehensive set of measures on disease state, clinical complications, cognition, function, mood, social supports, environmental conditions, medication use, health service use, etc. The LS collects personal, preferential data within the context of the wellness domains. Data collected via the HSC and LS are summarized in a Resident Snapshot to guide the coaching process. PAM, a 10-item, self-administered tool assessed the extent to which the participants were informed of and participated in their own health care [22]. The PAM includes psychological factors and personal competencies needed by an individual to manage their own health. Cumulative item responses are segmented into 1 of 4 progressively higher activation levels.
Sample
Inclusion/exclusion criteria: For inclusion in the study, participants had to be 60 years or older, living in subsidized housing within the urban housing authority, and have a language preference of English or Spanish. Older adults under the age of 60 years or not living within the housing authority were excluded.
Sites: The first housing site had 181 units with 42.7% of the residents living below the poverty line [23]. Its population was ethnically diverse with 12% White non-Hispanic, 41.5% Black non-Hispanic, and 43.5% Hispanic. The second housing site, located within the same neighborhood, was made up of 82 units and was used to recruit the wait-list control group. Here, the residents are also ethnically diverse with 3.6% White non-Hispanic, 72.6% Black non-Hispanic, and 21.4% Hispanic [23].
Recruitment: The principal investigator and the wellness coach met with resident service coordinators from both housing sites to review the specific elements of the study. Material and scheduled discussions were presented and posted at the two sites to explain the project. In addition, residents received a written letter inviting them to join the study and participate in the assessment process. The letter indicated that they would receive an in-person contact by program staff and if the resident had any questions, a second personal contact was scheduled.
Phase I: Ten participants from Site #1 initially were enrolled in the wellness coaching program for a 3-month trial. During this period, standard assessment data were collected and monthly, semi-structured interviews conducted to obtain feedback regarding the usability, acceptability, and satisfaction with the coaching process and platform. At the end of the 3-month feasibility trial, a more detailed debriefing via focus group discussion was completed with all project participants to ascertain how best to adapt the coaching process in preparation for the second stage of the research project. The adaptations included culturally specific strategies to increase physical activity and integration of no-cost resources to promote health behaviors. The book, Exercise & Physical Activity: Your Everyday Guide from the National Institute on Aging, was distributed to all enrollees. After determining frequently visited sites, such as place of worship, grocery store, public transportation access, the participants were provided with walking maps to provide direction as well as a mileage and step measure of the walking distance. Information about existing exercise classes within the Housing Authority was shared among the group.
Phase II: After program revisions were complete, five new participants from Site #1 for a 12-month test of the intervention and thirteen new participants from Site #2 for the wait-list control (for the following six months) were recruited. At the end of the six months, Site #2 participants received the intervention. At the completion of the study, all participants received a $10 gift card to the local grocery store.
Measurement of Outcomes
Four primary outcomes of the intervention were assessed in this pilot project: patient activation, physical activity level, self-rated health status, and self-rated quality of life. The first outcome was measured by the PAM. The remaining three outcomes were drawn from the two interRAI’s assessment tools used to complete the comprehensive assessment upon entry into the project, the LS and HSC. The specific outcome measures were selected because they represent aspects of successful aging and confidence towards managing one’s own health and health care.
Analysis
Data analyses were performed using SPSS (Version 23.0). Descriptive, exploratory analyses investigated treatment differences at each time point from both sites. Independent t-tests (p<0.05) were calculated to compare baseline and follow-up results. Analyses were done for the first ten participants testing the feasibility and acceptability of the intervention, the five participants who participated in the intervention six months later, and for the wait-list control group before and after crossing over to the intervention.
Results
The specific aims of this pilot project were to: (1) determine appropriate strategies for implementing the wellness coaching model among low-income older adults from populations with health disparities and (2) to conduct a pilot test to determine whether lowincome older adults who participate in a personalized, strategic wellness coaching model as compared to a wait-listed control group will have higher self-management behaviors of increased activation, increased physical activity, and result in an improved self-rated health status and quality of life.
We initially obtained a target sample of 10 older adults to achieve specific aim #1. During the first six months of the project in examining the feasibility of the intervention, one study participant left the site and moved to a long-term care facility. Within this group, there were 3 females (2 Hispanic) and 7 males (3 Hispanic); ages ranged from 61 to 85 years old. After the initial six months, we recruited an additional five participants from the Site #1 to enroll in the project and receive the intervention. Within this group there were 2 females and 3 males whose ages ranged from 60 to 89.
At the same 6-month point in the project, thirteen study participants were recruited for the wait-list control group from Site #2. These participants ranged in age from 60 to 88 years old. There were 7 females and 6 males, 23 % Hispanic and 77% Black. Baseline at recruitment, 6-months, and one-year follow-up data were collected from this control group. The study participants from Site #2 crossed over to the intervention group after the six months. During the initial six months, they attended health education sessions provided on-site by graduate nursing students. They participated in the wellness coaching intervention for the final six months of the project.
To achieve our first aim, we introduced the intervention to a group of 10 older adult residents. After participating in the intervention for three months, we conducted a focus group discussion with nine of the participants. The results of this discussion led to the development of specific strategies described previously, to support the wellness coaching process and provide key resources to these individuals.
In conducting preliminary, descriptive data analyses, participants were initially placed in one of three sub-groups: Site #1 with an 18- month exposure to the intervention, Site #1 with a 12-month exposure to the intervention, and Site #2, the control group for six months, then cross-over with exposure to the intervention for six months. Subsequently, independent t-tests were performed comparing Site #1 and Site #2 at baseline, six, and twelve months.
Key outcomes
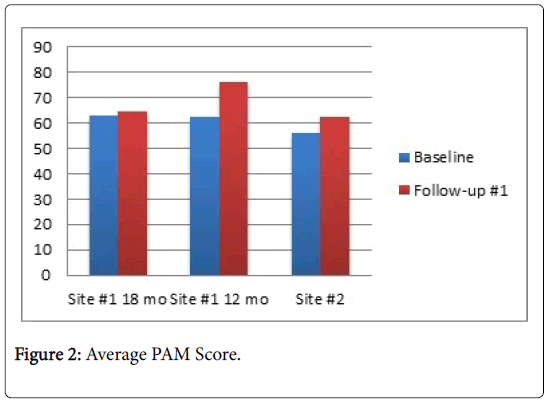
Patient activation: This outcome was measured using a targeted tool, the Patient Activation Measure. All three sub-groups demonstrated an increase in the mean patient activation score from baseline to postintervention but only one of these increases, Site #1, 12-month group, was statistically significant. Comparison of Sites #1 and #2 revealed no statistically significant difference in average PAM scores at baseline and 12-month follow-up. Table 1 provides a summary of the results. Figure 2 displays the average PAM scores for the three sub-groups at baseline and follow-up. There was no significant difference in follow-up PAM scores between Site #1 and Site #2 and t-test results are summarized in Table 1.
| Site #1 | Site #2 | ||||||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | T-value | df | p | |
| Baseline | 62.77 | 7.85 | 56.15 | 9.96 | 1.96 | 26 | 0.06 |
| Follow-up | 68.97 | 12.62 | 62.17 | 12.62 | 1.26 | 22 | 0.22 |
Table 1: T-test results for patient activation score.
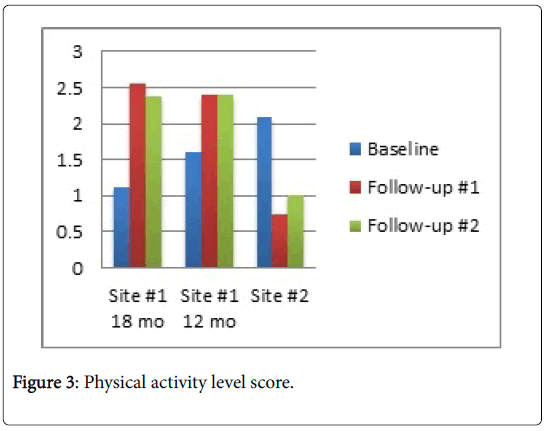
Physical activity level: There were statistically significant improvements in physical activity levels for the participants in each of the Site #1 sub-groups with physical activity level measured as the amount of time spent engaged in exercise or other exercise-type activities. For Site #2, the physical activity level declined from baseline to post-intervention assessment although this decline was not statistically significant. Figure 3 presents the average physical activity level for each sub-group.
At baseline assessment, there was no significant difference in physical activity level between the two study sites although the average was higher for Site #2 participants. At the 6-month follow-up where only the Site #1 received the intervention, there was a statistically significant difference between the two sites with greater improvements among Site #1 participants. Table 2 summarizes these results. The significant difference was sustained at 12 months.
| Site #1 | Site #2 | ||||||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | T-value | df | p | |
| Baseline | 1.27 | 0.96 | 1.92 | 1.49 | -1.39 | 26 | 0.174 |
| Follow-up 1 | 2.43 | 1.08 | 0.88 | 0.64 | 3.66 | 20 | 0.002* |
| Follow-up 2 | 2.23 | 1.01 | 1.18 | 1.16 | 2.36 | 22 | 0.028* |
Table 2: T-test results for physical activity level.
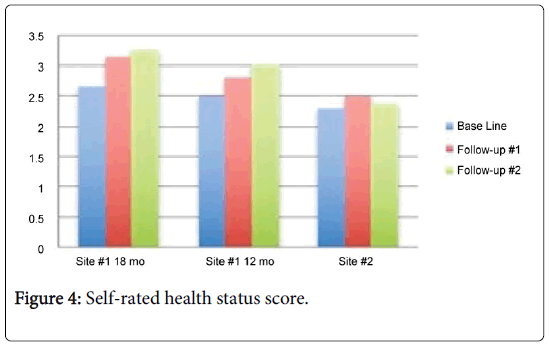
Self-rated health status: Scores for the self-report of health status improved for the two sub-groups from Site #1 and had little variability for the group in Site #2. Average scores for the sub-groups over the length of the project are presented in Figure 4.
Independent group comparisons for health status revealed statistically significant results at the second follow-up, the point at which Site #1 participants had received the intervention for twelve months and Site #2 participants had received the intervention for six months. Table 3 contains the analyses results.
| Site #1 | Site #2 | ||||||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | T-value | df | p | |
| Baseline | 2.6 | 0.74 | 2.31 | 0.85 | 0.972 | 26 | 0.34 |
| Follow-up 1 | 2.86 | 0.77 | 2.5 | 0.53 | 1.15 | 20 | 0.261 |
| Follow-up 2 | 3.08 | 0.64 | 2.36 | 0.81 | 2.41 | 22 | 0.025* |
Table 3: T-test results for health status.
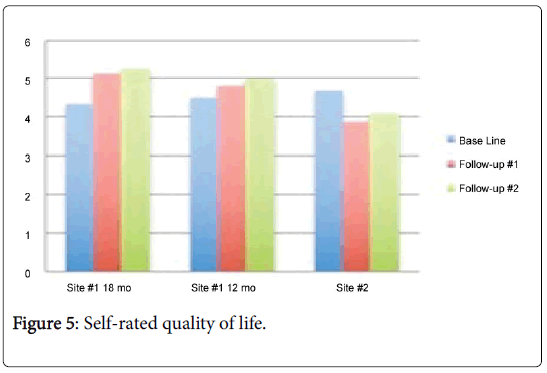
Self-rated quality of life: The scores for the quality of life measure improved for both of the Site #1 sub-groups but worsened for Site #2. For Site #2, the decreased mean score post-intervention was statistically significant. The results are summarized in Figure 5.
There were statistically significant differences in self-rated quality of life between Site #1 and Site #2. While similar at baseline, ratings improved after participating in the intervention for participants from both sites but at the 6- and 12-month follow-up, Site #1 had consistently higher ratings. T-test analysis results are summarized in Table 4.
| Site #1 | Site #2 | ||||||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | T-value | df | p | |
| Baseline | 4.33 | 0.9 | 4.69 | 0.947 | -1.027 | 26 | 0.314 |
| Follow-up 1 | 4.93 | 0.917 | 3.88 | 0.834 | 2.67 | 20 | 0.015* |
| Follow-up 2 | 5.08 | 0.954 | 4.09 | 1.13 | 2.31 | 22 | 0.030* |
Table 4: T-test results for quality of life.
Discussion
Our results show modest gains with patient activation and selfreported health status and quality of life. Among all participants, there was an increase in the average PAM score from baseline to the 12- month follow-up. Although the paired comparisons were not statistically significant, the group that received the intervention for twelve months, as opposed to six months, demonstrated higher average activation levels. Chubak et al. [24] found that PAM scores tend to fluctuate over time although an adverse event or change in health status was not associated with lower scores. While health literacy was not assessed among the participants, the wait-list control group did receive health education and both literacy and education have been shown to reduce racial differences in patient activation [25].
Improvement in physical activity levels was more dramatic, particularly for the initial Site #1 sub-group who, after three months, received targeted support to improve this outcome. Promoting walking groups and exercising with friends was encouraged by the wellness coach and appeared to work effectively with the Site #1 participants. Greaney, Lees et al. [26] suggest interventions that counter negative attitudes towards exercise for older adults such that regular exercise is a socially acceptable may improve participation. Older adults who capitalized on their social networks to exercise with others demonstrate improved outcomes and retention [27,28]. Anecdotally, the wellness coach noted that the participants favored walking with a companion or small group to going out alone.
Central to the intervention tested in this pilot project is the use of a healthy aging plan and repeated contacts by the wellness coach. The use of a healthy aging plan parallels implementation intention, an intervention shown to increase physical activity levels [29]. Older adult women reported increased physical activity during a 4-week implementation intention intervention although there was an association between stronger executive function and increased activity suggesting need for optimal cognitive performance [30]. In another study, health action plans that included individualized goals and preferences resulted in increased engagement with exercise and decreased depressive symptoms [31-37].
Limitations
The pilot project was an initial attempt to introduce and modified a wellness program, successful among suburban-based, continuing care retirement community residents (CCRC) for vulnerable, urbandwelling, low-income older adults [18]. Unlike the CCRC setting, recruitment of study subjects was challenging despite use of multiple community events and strategies as well as close collaboration with the resident service coordinator. A small sample size resulted, although racial and ethnic diversity was present. A small number declined to complete the follow-up assessments although the wellness coach continued to contact these individuals at the same scheduled intervals. Upon further reflection and discussions with the wellness coach, a distinguishing factor emerged for the participants from Site #2. Anecdotally, the wellness coach reported that during the 6-month intervention period, some Site #2 participants experienced health issues requiring hospitalizations, rehabilitation, and repeated health care visits. This report concurs with no change assessed for health status, a decrease in quality of life as well as a decrease in the physical activity level for those from Site #2. Thus, comparative evaluation of the wellness coaching intervention must be limited although decline in health status among older adults often occurs and the self-report of health status did not decrease significantly over the study period.
Conclusion
Similar to continuing care retirement community residents, urbandwelling, low-income older adults were able to identify their goals and, through a wellness coaching process, engage in the development of their personal healthy aging plan, facilitating their involvement in health care self-management. Capitalizing on social networks and other low or no-cost options to support goal achievement may be a key strategy in resource-restricted environments. Notably, the increase in physical activity level was an important outcome with benefits extending to other aspects of wellness. Several established health care self-management programs rely on peer leaders to enhance program effectiveness. The use of informal peer support as well as formally trained, volunteer peer mentors among low-income elders is worthy of study, particularly considering the need for low-cost, self-sustaining, scalable programs for a growing older adult population. The less than favorable outcomes from the sub-group that experienced repeated health challenges suggests a need to adjust personal goals based upon a changing health status. Appropriate and innovative strategies must be implemented to help aging adults live with dignity and independence. An informed, active population of low-income older adults has the most to gain through new approaches to personal responsibility, goal-setting, and self-management of their health. Future research to implement and evaluate innovative, cost-effective approaches is needed to best serve this vulnerable population.
Acknowledgement
The authors first wish to acknowledge and thank the older adults who participated in this project. In addition, they wish to recognize the support of the senior research mentors, including Dr. John N. Morris, Dr. Barbara J. Guthrie, and Dr. Carmen Sceppa. Students (Mairead Day, Monica Fernandez del Castillo, Lisa McBride, Paige Marshall, Ngozi Otaluka, Bryanna Seymour, Latoya Browne, Lena Vo, Elaine Cui, Gabriella Rao, Meredith Craig) all assisted with the study. Finally, the authors wish to acknowledge the consistent support from John B. Kane, Senior Program Coordinator of the Boston Housing Authority.
Financial Support
This project was funded by National Institute of Nursing Research (NINR) P20NR015320 and sponsored by NUCare –Northeastern University Center for Self Care & Health Technology and Resources for Nurse Scientists and the Bouvé College of Health Sciences.
Authors’ Contribution
Each author meets the uniform requirements of the Journal of Community and Public Health Nursing criteria for authorship. EPH was responsible for the literature review, study design, methods, analysis and preparation of the manuscript. BL assisted with subject recruitment, data collection, interpretation of results and preparation of the manuscript.
Disclosure
EP Howard is a Fellow in InterRAI.
Conflict of Interest
The authors have no conflict of interest to report.
References
- https://www.census.gov/content/dam/Census/library/publications/2016/demo/p95-16-1.pdf
- https://aoa.acl.gov/Aging_Statistics/Profile/2015/docs/2015-Profile.pdf.
- Lehnert T, Heider D, Leicht H, Heinrich S, Corrieri S, et al.(2011) Review: health care utilization and costs of elderly persons with multiple chronic conditions. Med Care Res Rev 68:387-420.
- Elliott AF, McGwin G, Kline LB, Owsley C (2015) Vision impairment among older adults residing in subsidized housing communities. Gerontologist 1:S108-S117.
- Parsons PL, Mezuk B, Ratliff S, Lapane KL (2011) Subsidized housing not subsidized health: health status and fatigue among elders in public housing and other community settings. Ethn Dis 21:85.
- Anderson EK, Moss TP (2011) Imagery and implementation intention: a randomized Controlled trial of interventions to increase exercise behavior in the general population. Psych Sport Exer 12: 63-70.
- https://www.huduser.gov/portal/sites/default/files/pdf/Worst-Case-Housing-Needs.pdf
- Freedman VA, Spillman BC (2014) The residential continuum from home to nursing home: size, characteristics and unmet needs of older adults. J Gerontol B Psychol Sci Soc Sci 69:S42-S50.
- Aneshensel CS, Wight RG, Miller-Martinez D, Botticello AL, Karlamangla AS, et al. (2007) Urban neighborhoods and depressive symptoms among older adults. J Gerontol B Psychol Sci Soc Sc 62:S52-59.
- Choi NG, Hegel MT, Marinucci M, Sirrianni L, Bruce ML (2012) Association between participant-identified problems and depression severity in problem-solving therapy for low-income homebound older adults. Int J Geriatr Psychiatry 27:491-499.
- Coberly C, Rula EY, Pope JE (2011) Effectiveness of health and wellness Initiatives for seniors. Popul Health Manag 14:S45-50.
- Counsell SR, Callahan CM, Clark DO, Tu W, Buttar AB, et al. (2007) Geriatric care management for low-income seniors: Arandomized controlled trial. JAMA 298:2623-2633.
- Minkler M, Fuller-Thomson E, Guralnik JM (2006) Gradient of disability across the socioeconomic spectrum in the United States. N Engl J Med 355:695-703.
- Thorpe RJ, Weiss C, Xue Q, Fried L (2009) Transitions among disability levels or death in African American and white older women. J Gerontol A Biol Sci Med Sci 64: 670-674.
- Ory MG, Ahn S, Jiang L, Smith ML, Ritter PL, et al. (2013) Successes of a national study of the chronic disease self-management program: meeting the triple aim of health care reform. Med care 51:992-998.
- Powers MA, Bardsley J, Cypress M, Duker P, Funnell MM, et al. (2015) Diabetes self-management education and support in type 2 diabetes a joint position statement of the American Diabetes Association, the American Association of Diabetes Educators, and the Academy of Nutrition and Dietetics. Clin Diabetes 34:70-80.
- Topaz M, Troutman-Jordan M, MacKenzie M (2014) Construction, deconstruction, and reconstruction: The roots of successful aging theories. Nurs Sci Q 27: 226-233.
- Howard EP, Schreiber R, Morris JN, Russotto A, Flashner-Fineman S (2016) COLLAGE 360: a model of person-centered care to promote health among older adults. J Ageing Res Health 1:21-30.
- Hirdes JP, Ljunggren G, Morris JN, Frijters DH, Soveri HF, et al. (2008) Reliability of the interRAI suite of assessment instruments: a 12-country study of an integrated health information system. BMC Health Serv Res 8:277.
- Carpenter GI (2006) Accuracy, validity and reliability in assessment and in evaluation of services for older people: The role of the interRAI MDS assessment system. Age Ageing 35: 327-329.
- Strout K, Howard EP (2014) Application of the Rasch model to measure five dimensions of wellness in community-dwelling older adults. J Nurs Meas 22:268-290.
- Skolasky RL, Green AF, Scharfstein D, Boult C, Reider L, et al. (2011) Psychometric properties of the patient activation measure among multimorbid older adults. Health Serv Res 46:457-478.
- Chubak J, Anderson ML, Saunders KW, Hubbard RA, Tuzzio L, et al. (2012) Predictors of 1-Year Change in Patient Activation in Older Adults with Diabetes Mellitus and Heart Disease. J Am Geriatr Soc 60:1316-1321.
- Eneanya ND, Winter M, Cabral H, Waite K, Henault L, et al. (2016) "Health Literacy and Education as Mediators of Racial Disparities in Patient Activation Within an Elderly Patient Cohort." J Health Care Poor Underserved 27:1427-1440.
- Greaney ML, Lees FD, Blissmer BJ, Riebe D, Clark PG (2016) Psychosocial factors associated with physical activity in older adults. Ann Rev Geron Geriat 36:273-291.
- Chiang KC, Seman L, Belza B, Tsai JH (2008) “It is our exercise familyâ€: experiences of ethnic older adults in a group-based exercise program. Prev Chronic Dis 5:A05.
- Kassavou A, Turner A, French DP (2013) Do intervention to promote walking in groups increase physical activity? A meta-analysis. Int J Behav Nutr Phys Act 10:18.
- Anderson EK, Moss TP (2011) Imagery and implementation intention: a randomized Controlled trial of interventions to increase exercise behavior in the general population. Psych Sport Exer 12: 63-70.
- Hall PA, Zehr C, Paulitzki J, Rhodes R (2014) Implementation intentions for physical activity behavior in older adult women: an examination of executive function as a moderator of treatment effects. Ann Behav Med 48:130-136.
- Holland SK, Greenberg J, Tidwell L, Malone J, Mullan J, et al. (2005) Community-based health coaching, exercise and health service utilization. J Aging Health 17:697-716.
- Bélanger-Gravel A, Godin G, Bilodeau A, Poirier P (2012) The effect of implementation intentions on physical activity among obese older adults: a randomized control study. Psychol Health 28:217-233.
- https://order.nia.nih.gov/publication/exercise-physical-activity-your-everyday-guide-from-the-national-institute-on-aging
- https://www.worldcat.org/title/gerotranscendence-a-developmental-theory-of-positive-aging/oclc/59003690
Citation: Howard EP, Lee B (2019) Use of a Wellness Coaching Model among Urban-dwelling, Low-income Older Adults. J Comm Pub Health Nursing 5:232. DOI: 10.4172/2471-9846.1000232
Copyright: © 2019 Howard EP, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 2912
- [From(publication date): 0-2019 - Apr 29, 2025]
- Breakdown by view type
- HTML page views: 2124
- PDF downloads: 788